
Quality Jobs for Quality Care
The Path to a Living Wage for Nursing Home Workers
November 2015

Page 1
About Massachusetts Senior Care Association
The Massachusetts Senior Care Association represents a diverse set of organizations that deliver a broad
spectrum of services to meet the needs of older adults and people with disabilities. Our members
include more than 500 nursing and rehabilitation facilities, assisted living residences, residential care
facilities and continuing care retirement communities.
Forming a crucial link in the continuum of care, Mass Senior Care facilities provide housing, health care
and support services to 150,000 people a year; employ more than 77,000 staff members; and contribute
more than $4 billion annually to the Massachusetts economy.
Since its founding in 1949, Mass Senior Care's mission has been to improve the quality and delivery of
long term care services in Massachusetts through research, education and advocacy.
Acknowledgments
A team of Massachusetts Senior Care Association staff contributed to this report, including Director of
Labor and Workforce Development Kelly Aiken, Director of Reimbursement Gary Abrahams, Director
of Public Affairs Jennifer Chen and Senior Vice President Tara Gregorio. Mass Senior Care would like to
acknowledge the following Board members for their contributions, insights and critical feedback on this
report: William Bogdanovich, Chairman, Massachusetts Senior Care Association, President and CEO,
Broad Reach Rehabilitation and Skilled Care Center at Liberty Commons; Marva Serotkin, President,
Massachusetts Senior Care Foundation, CEO, The Boston Home; Matthew Salmon, CEO, SALMON
Health and Retirement and Richard Bane, President, BaneCare Management. Special thanks to external
reviewers Steven L. Dawson, Strategic Advisor, PHI on behalf of the National Fund for Workforce
Solutions and Christine Bishop, Atran Professor of Labor Economics, The Heller School for Social Policy
and Management, Brandeis University.

Page 2
Quality Jobs for Quality Care:
A Path to a Living Wage for Nursing Home Workers
Executive Summary
The commitment and dedication of the state’s long term care workforce has propelled Massachusetts into
a position of national leadership in providing quality long term care services to frail elders and people with
disabilities who can no longer live safely in the community. Seventy-seven thousand nursing home staff
work tirelessly in the Commonwealth’s more than 400 long term and post-acute care facilities to ensure
residents and their families receive the quality care and support they need and deserve. Their ability to
deliver quality care is dependent on the quality of their jobs.
While nursing home consumer satisfaction remains high and hospital readmissions have declined, over half
of nursing home staff do not have access to the most essential element of a quality job – a living wage.
Most often this impacts immigrants and single mothers who view their job in a nursing home as a starting
point on a career pathway to making a family-sustaining wage.
Seventy-ve percent of a nursing home’s budget is used to fund employee wages and benets. With
MassHealth funding the care of over two-thirds of nursing home residents, wage increases for nursing home
staff are predominantly dependent upon adequate MassHealth payment by the Commonwealth. Since
2008 there has been little state investment in nursing home care for MassHealth residents. Consequently,
certied nurse aides (CNAs) have seen a mere 4% cumulative increase in actual wages over the last seven
years and a 6% decline in real wages for this 2008-2015 period. CNAs working in other settings such as
hospitals can now earn as much as 20% more, leaving nursing homes at a competitive disadvantage. In
addition, Massachusetts Governor Charlie Baker has committed to a goal of providing a $15 per hour
starting wage for the state’s Personal Care Attendants (PCAs) in 2018.
Ensuring staff stability and job satisfaction is critical to providing quality care in nursing homes. Recruiting
and retaining qualied staff passionate about working with frail elders and people with disabilities is an
ongoing priority for Massachusetts nursing home providers. However, that has become increasingly
challenging. CNA vacancy rates have doubled over the last ve years leaving one in ten positions unlled.
As the economy improves, there is increased recruitment competition among nursing facilities, hospitals,
assisted living residences and home care agencies for CNA staff, which is further exacerbated by a decrease
in the supply of newly trained CNAs. Projected declines in the caretaking workforce, women age 25 to 44,
will only make matters worse over the next 10 years.
Wages play a critical role in dening quality jobs, but other elements such as benets, job security, fair work
schedule, career advancement and a supportive work environment are also crucial. While skilled nursing
facilities offer many of the elements of a quality job, there is opportunity for improvement. A combination
of strategies is needed to create quality jobs that provide higher wages and an improved working
environment to increase retention of existing staff and recruitment of new staff.

Page 3
Recommendations for Investment
The Massachusetts Legislature funded the Nursing Home Quality Initiative beginning in 2000. This multi-
pronged initiative, which became a national model, demonstrated that increased state investment in nursing
homes improved job quality, while enhancing resident care. A similar investment in quality nursing home
care is needed to fund the following recommendations:
• Create a Pathway to a Living Wage – Develop a multi-year funding strategy that includes
both an immediate and annual wage pass-through for the lowest wage workers including CNAs,
dietary, laundry and housekeeping staff, tying the wage increase to the Consumer Price Index.
• Support a Culture of Retention – Fund the rollout and implementation of comprehensive
evidence-based supervisory training for the express purpose of retaining staff and reducing turnover.
• Establish a CNA Scholarship Program – Support more adults in their quest for post-
secondary credentials by providing scholarships for integrated training that includes both
Adult Basic Education/English as a Second Language and CNA training.
By investing directly in nursing home staff, Massachusetts will remain a leader in providing quality care for
residents and their families and improve the lives of thousands of workers across the Commonwealth.

Page 4
Introduction
Seventy-seven thousand dedicated nursing home staff deliver high quality care to frail elders and people
with disabilities every day in the Commonwealth’s 400 long term and post-acute care facilities. As a result
of the tireless commitment and dedication of its workforce, Massachusetts is a national leader in providing
quality long term care services to individuals who can no longer live safely in the community. Massachusetts
facilities have among the highest percentage of Department of Public Health “deciency free” nursing
facilities compared to the national average. Consumer satisfaction remains high and hospital readmissions
have steadily declined. As the population ages and demand for long term care services continues to rise,
these quality accomplishments can only be maintained and improved upon when nursing home staff are
recognized and supported for their commitment to providing excellent care.
Quality care in all facilities is dependent on quality jobs and staff stability. Hiring and retaining qualied
staff passionate about working with frail elders and people with disabilities remains an ongoing priority
for Massachusetts nursing home providers. However, state underfunding for nursing home services has
resulted in non-competitive wages and high staff vacancy rates. Seventy-ve percent of a nursing home’s
budget is used to fund employee wages and benets. And, with MassHealth funding the care of over two-
thirds of nursing home residents, a nursing home’s ability to invest in staff is largely dependent upon state
funding. As a result, many nursing home workers, particularly certied nurse aides (CNAs) and dietary,
housekeeping and laundry aides, cannot afford to do the work they love because of persistent low wages.
This often forces staff to seek employment elsewhere and leads to disruptions in resident care. It is
critically important to ensure that staff instability does not negatively impact quality of care for residents
and their families.
Forty thousand full-time and part-time entry level positions in nursing homes offer a critical employment
gateway for immigrants, women previously out of the labor market, young adults and others seeking a
healthcare career. The majority of entry level staff work as CNAs, providing direct care and companionship
to residents while assisting with activities of daily living such as eating, walking and bathing. Equally
important to the lives of residents is ancillary staff indirectly associated with patient care such as dietary,
housekeeping and laundry aides.
The entry level nursing home workforce is predominantly women between the ages of 18-44 and highly
diverse with 48% of CNAs self-identifying as Latino or nonwhite (American Community Survey, 2010).
Many are single parents with young children. Frequently a rst job in a nursing home is a career starting
point and can provide a pathway to advanced education and a family sustaining wage.
Yet, in today’s environment these entry level nursing home workers do not have a clear pathway to a living
wage - the most essential element of a quality job. Skilled nursing facilities do offer many other elements
of a quality job, including benets, job security, fair work scheduling and career advancement. However, a
sustained approach to high quality jobs for high quality care requires investing in wages, workers and the
work environment.
Page 5
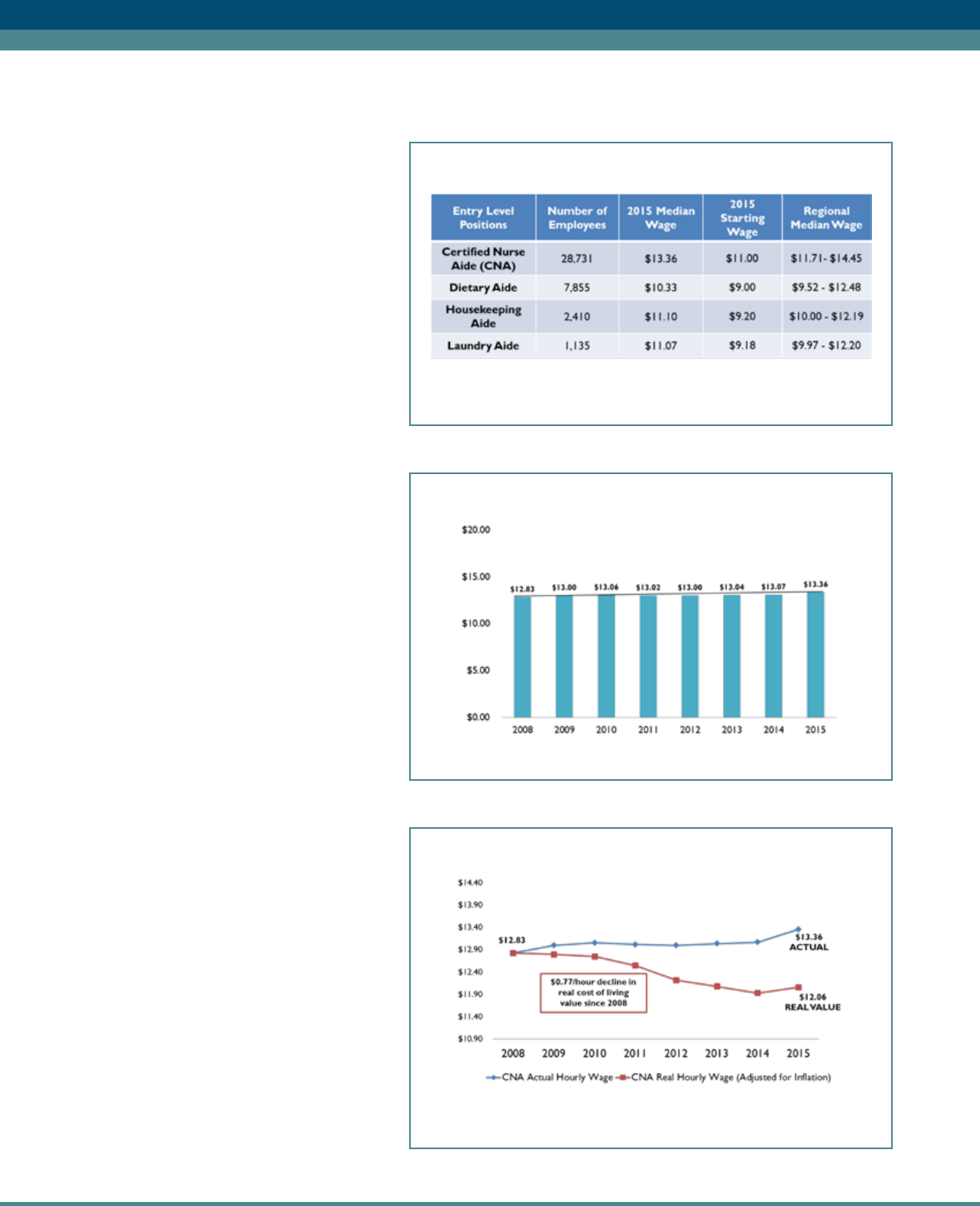
Current Entry Level Staff Wages
Although their services are vital to
maintaining the health, dignity and quality
of life for nursing home residents, the
2015 statewide median CNA wage is
only $13.36 per hour or $2,316 per
month if working full-time. Median
ancillary staff wages are even lower
ranging from $10.33 to $11.10 per
hour. Across the state, regional wage
variation exists as well (See Appendix
for a breakdown of wages by county).
These low wages dramatically impact the
quality of jobs and the lives of nursing
home workers and their families.
CNA wages have remained stagnant,
growing only 4% cumulatively from
2008-2015 (Chart 1). If adjusted for
ination, CNA real wages have actually
fallen by 6% through 2015. As seen in
Chart 2, this represents a $.77/hour
decline in real cost of living value over
this seven year period. By contrast, the
cost of living in the Metro Boston Area
increased by 11% for this period. And,
with the fair market rent of a two-
bedroom apartment totaling $1,494
per month in Metro Boston, a CNA
would have to spend about 60% of her
annual wages on housing (National Low
Income Housing Report, 2013). Across
the state, the cost of living for CNAs
has signicantly outpaced wage increases
(MSCA, 2015).
Sources: Mass Senior Care Association Annual Employment Survey,
2015 and CHIA Nursing Home Annual Cost Report
Table 1: 2015 Entry Level Staff Wages
Chart 1: Median CNA Hourly Wage (2008-2015)
Source: Mass Senior Care Association Annual Employment Surveys
Chart 2: Real vs Actual CNA Wages (2008-2015)
Sources: Massachusetts Senior Care Annual Employment Surveys
and CPI – Bureau of Labor Statistics

Page 6
What is a Living Wage?
A living wage provides a wage and benets package that takes into account the area-specic cost of living,
as well as the basic expenses involved in supporting a family. By working a single full-time job, an individual
should be able to rent an apartment and pay for other monthly expenses like food and transportation. In
the calculation of a living wage, the Crittenton Women’s Union Economic Independence Calculator takes
into consideration monthly expenses, cost of child care and health care, regional cost of living and taxes.
Using their calculator, a nursing home CNA making the state’s 2015 median base hourly wage will not meet
the living wage requirements for a single parent with one child living in Massachusetts. For example, in 2013
the living wage in Waltham exceeds $24 per hour for one adult with a school aged child. For one adult
living in Waltham, the living wage was $15.05/hour.
Across the state, the CNA base hourly wage meets less than 70% of the standard living wage for a family of
one adult and one child. This is particularly alarming because many low wage workers are single parents and
Massachusetts ranks among the least affordable states for center-based preschool care (Child Care Aware,
2014).
To make ends meet, many CNAs and ancillary staff hold more than one job and rely on public benets.
Anecdotal evidence and CNA interviews suggest the majority of low wage staff juggle multiple jobs and
sometimes work 75-80 hours per week. The Paraprofessional Healthcare Institute (PHI) reports that over
54% of CNAs and home health aides in Massachusetts receive some form of public assistance such as
MassHealth or Food and Nutrition and 42% live in households earning incomes below 200% of the federal
poverty level (PHI, 2012 and 2015).
Why Nursing Homes Cannot Pay Their Employees A Living Wage
Nursing homes are a major economic contributor both statewide and in local communities across the
Commonwealth. In many rural communities, nursing homes are the largest healthcare employer in the
region. Every year the sector generates $4.3 billion in economic activity with $3 billion in labor spending.
As seen in Chart 3, $.75 of every nursing facility “dollar” funds employee wages and benets which means a
nursing home’s ability to invest in staff is dependent upon state funding.
Table 2: “Living Wage” vs. Actual CNA Wage in Waltham
Source: Economic Independence Calculator, Crittenton Women’s Union, 2013;
Mass Senior Care Association Annual Employment Survey (Actual CNA Wage, 2015)

Page 7
In comparison to other healthcare employers such as hospitals and home health agencies, state funding is a
much more critical determinant of nursing home wages. With the care of over two-thirds of nursing home
residents paid for by MassHealth, Massachusetts nursing facilities are uniquely dependent upon state funding
to ensure quality resident care and quality jobs. Years of MassHealth underfunding for nursing home care
has caused a $37 per day gap between the cost of providing resident care and MassHealth payment. This
funding crisis has made it virtually impossible for
nursing home providers to ll staff vacancies and
make meaningful investments in their workforce.
It is important to highlight this direct relationship
between adequate Medicaid funding for nursing
home care and increases in wages for nursing
home employees. From 1999-2008, MassHealth
made signicant investments in nursing home care
and nursing homes passed along these Medicaid
rate increases to their staff through annual wage
hikes. Since the start of the “Great Recession” in
2008, there has been little growth in MassHealth
funding for nursing home care (See Chart 4). As a
result, CNA wages stagnated for the period 2008-
2015, growing only 4% over the entire seven year
period from $12.83 per hour to $13.36 per hour (see Chart 1). The inability of nursing homes to provide
wage increases has understandably resulted in valuable staff leaving for higher paying jobs in other parts of
the healthcare system including hospitals, where CNAs can earn over 20% more (See Chart 5).
Chart 3: Breakdown of Nursing Home Spending
Source: DHCFP/CHIA Nursing Home Cost Reports
Chart 4: Direct Link Between Annual
Medicaid Rate Changes and Nursing Home
Wage Increases (1999-2013)
Source: DHCFP/CHIA Nursing Facility Cost Reports,
Prepared by Mass Senior Care Association
Chart 5: Health Care Aide Wage and Medicaid
Dependency by Provider Type (2014)
Sources: Mass Senior Care Association Annual Employment Survey,
2014 (NF); Home Care Alliance of Massachusetts 2014 Employment
Survey (Home Health Agency); and Bureau of Labor Statistics
Occupational Employment Statistics (Hospital)

Page 8
Critical Demand for Services
Even as consumers receive more care and services in their homes, the demand for long term care services
over the next 15 years is expected to rise dramatically to keep pace with the growth of the over 65
population. From 2015 through 2030, the 75-84 age cohort will increase by close to 70%. “Younger”
seniors age 65-74 will grow by over 40%. Both cohorts will increase demand for short stay post-acute and
rehabilitative care in skilled nursing facilities. The 85+ age cohort, the group most likely to need long term
care services, will grow substantially (over 21%) but at a slower pace than the 65 through 84 population
over the next 15 years (UMass Donahue Institute 2015 Population Projections, March 2015). While many
older adults will seek to engage services enabling them to age at home or in their communities, nursing
home care will be critical for those who can no longer safely age in place or need assistance during short
term recovery.
With the state’s successful “Community First” policy and increased investments in community-based
services, many individuals who need residential long term care services are accessing nursing home care
later in their illness. Their acuity level increases the demands on frontline staff, requiring additional training
to keep pace with delivering quality care in a more complex environment. All of these factors reinforce the
critical importance of stabilizing the nursing home workforce now and ensuring access to quality jobs.
Staff Vacancies Expected to Increase
The nursing home provider community has a history of workforce shortages that ebb and ow with the
economy. In September 2015, Massachusetts posted a 4.5% unemployment rate compared to 5.1% at the
national level. As the state moves to a full employment economy, competition for low wage workers is
expected to increase across all industries. In previous periods of full employment, PHI notes that “prevailing
wage rates have made it difcult for many long term care providers to compete for workers with employers
offering less physically and emotionally demanding low wage jobs” (PHI, 2003).
In ve years, the CNA vacancy rate has nearly doubled to 10.6%. As illustrated in Chart 6, one in ten
unlled CNA positions across the state equates to approximately 2,270 open and unlled positions (MSCA,
2015). Vacancy rates and the number of open positions vary across the state, with Middlesex, Worcester
and three Western Massachusetts counties (Franklin, Hampshire and Hampden) accounting for almost half
of all vacant CNA positions. These counties have the highest concentration of nursing homes in the state.
Chart 6: CNA Vacancy Rates and Estimated Unlled Positions (2015)
*Western Mass = Franklin, Hampshire and Hampden Counties
Source: Mass Senior Care Association Annual Employment Survey, 2015

Page 9
As vacancy rates increase so does job stress for incumbent CNAs who often are left to work short staffed
and additional hours. In 2015, an estimated $40 million was paid to nursing facility staff for overtime as well
as additional expenditures for contracting with temporary nursing agencies.
Despite the high number of nurse aide training programs, competition for qualied CNA staff is increasing.
Originally only employed by nursing homes, CNAs now nd work in hospitals, assisted living, residential
mental health facilities, and home care agencies. In fact, the nurse aide has become the “universal worker”
for employers in many care settings. Employers value the basic skills development provided by the training,
as well as the competency assessment required by the state certication process and the certied nurse
aide registry maintained by the Massachusetts Department of Public Health (DPH). Competition is
exacerbated by a 5% drop in the number of new nurse aides added to the nursing aide registry from state
scal year 2014 to state scal year 2015 (Massachusetts Department of Public Health, 2015).
Current demographic projections suggest that the primary labor force, comprised of women age 25 to 54,
is expected to shrink over the next 10 years. This will likely further decrease the number of caregivers
available for the growing number of people who will require long term care services.
Staff Stability Impacts Quality of Care
Skilled nursing facilities in Massachusetts boast a higher than average staff retention rate when compared to
national statistics. The 2015 Massachusetts Senior Care Association wage and salary survey data indicates
that 70% of CNAs have worked in the same facility for one year or more. Many facilities have a strong core
of long term, dedicated employees. However, a smaller percentage of employees turn over more frequently.
This staff turnover impacts the continuity of resident care and costs the provider community an estimated
$35 million every year (MSCA, 2015).
In addition to disrupting continuity of care, high turnover rates and job dissatisfaction result in deteriorating
performance on quality indicators such as use of physical restraints, catheter use and pressure ulcers.
Conversely, when staff satisfaction is high nursing homes report fewer resident falls, fewer pressure ulcers,
and decreased use of catheters. Improved staff satisfaction also translates into reduced staff turnover and
absenteeism (Castle, 2007).
Studies have identied a number of factors that are associated with CNA job satisfaction, including higher
pay, assistance in alleviating job stress, and supervisors who show care and concern for their well-being.
The Institute of Medicine found that positive supervision can greatly increase direct care workers’ sense of
value, job satisfaction and intent to stay (Institute of Medicine, 2008). Supervisors and managers who are
trained to support staff and engage them in decision making demonstrate a higher level of care and concern
resulting in higher retention rates (Commonwealth Corporation, 2007).
Registered nurses and licensed practical nurses manage and supervise CNAs, yet few nurses have been
afforded adequate management skills training in their nursing education or have any experience supervising
staff before taking on the responsibility in a nursing home. Training for supervisors supports the pivotal role
that managers play in creating a culture of retention.

Page 10
Dening Job Quality Beyond Wages
While wages play an important role in dening quality jobs, other indicators contribute to the denition
as well, including: benets such as paid time off, health insurance, job security, fair work schedule, and a
supportive work environment. PHI maintains that the essential elements of a high quality job are fair
compensation, opportunities for professional growth and adequate support. Using these standards,
Massachusetts nursing homes offer higher quality entry level positions than many other industries. Some
examples include the following:
Benets: All nursing home staff have access to paid time off with an average of 27 days including vacation
and sick leave. A majority of facilities offer short and long term disability to full-time staff. While retirement
benets and health and dental insurance are also available, entry level staff are often unable to afford
participation in these programs. Many low wage staff rely on MassHealth for individual and family health
insurance.
Work Schedule and Job Security: Nursing homes offer year round stable jobs with consistent hours.
A variety of 24/7 work options are available to workers including full-time, part-time and per diem shifts.
There is no mandated overtime. Advance scheduling is the norm offering staff one or two week notice of
the upcoming schedule.
Career Advancement Opportunity: Nursing homes offer a career pathway for CNAs to become a
licensed practical nurse (LPN) or a registered nurse (RN), both positions that pay a family-sustaining wage.
In some facilities, interim pathway steps also include becoming a senior CNA. For those who need basic
skills development in order to advance, almost every community college across the state is working with
local nursing homes to provide easy access to college prep courses and adult basic education. Over 70%
of employers offer tuition assistance to employees to support additional education. There is also a 30 year
history within the provider community of supporting advancement opportunities by contributing to the
Massachusetts Senior Care Foundation Scholarship program which, over that time, has distributed some
$2.7 million in scholarships to 1,500 employees. However, the educational pathway to a family-sustaining
income for many is long and has opportunity costs, especially when juggling more than one job and a family.
Supportive Organizational Culture: Many Massachusetts nursing homes have created an organizational
culture modeled on principles of resident-centered care that promote choice, purpose and meaning in daily
life for frail elders and persons with disabilities. In a resident-centered care organization, staff form stronger
relationships with residents and their families because they consistently take care of the same individuals
enabling them to know a person’s preferences and better anticipate their needs. Staff is highly valued in
these types of organizations and it results in increased retention rates and improved quality outcomes.
Participating in Decision Making and Engaging in Continuous Quality Improvement: Enabling
CNAs and others to participate in decision making including care planning is an important aspect of
organizational culture and job satisfaction. Promoting continuous quality improvement in a manner that
integrates CNAs in the care planning process and provides specic tools for improving communications
and interactions with residents is equally important. Massachusetts nursing homes are leaders in
quality improvement initiatives, such as OASIS, a unique non-pharmacological approach to reducing
the use of antipsychotic medications in nursing home residents. Through a grant made possible by the
Massachusetts Department of Public Health, Bureau of Health Care Quality and Safety, staff from nearly
75% of Massachusetts nursing homes have participated in OASIS training, gaining the knowledge and tools

Page 11
that enable them to provide more individualized care to a broad range of residents, including those with
dementia. The active participation, engagement and leadership of CNAs, built on the strong relationships
they have with their residents, have contributed to OASIS’ success in improving dementia care and a 29%
reduction in antipsychotic drug use for long-stay residents in Massachusetts nursing homes (CMS Quality
Measures, 2011-2015).
While skilled nursing facilities meet many of the quality jobs criteria, it is just a foundation and there is a
critical need for improvement. Multiple strategies are needed to create quality jobs that provide higher
wages and an improved working environment to increase retention of existing staff and create a welcoming
environment to new employees.
State Investment in Workers Pays Off
History of Investment in Quality Jobs
The late 1990s was a period of economic distress for the nursing home provider community, creating
instability that threatened quality and access to care, evidenced in high turnover and vacancies among direct
care workers. In response, the Massachusetts Legislature enacted and funded the Nursing Home Quality
Initiative rst in 2000. Additional signicant investments in the nursing home workforce were also made in
subsequent years. The initial $42 million initiative focused on increasing high quality nursing home care for
residents and families by providing good jobs and opportunities for frontline caregivers (Eaton, 2001). The
core components of the initiative included: 1) a wage pass-through for direct care workers; 2) an education
and training program for workers and supervisors entitled the Extended Care Career Ladder Initiative
(ECCLI); 3) a direct care worker scholarship program; and 4) a statewide nursing home resident family
consumer satisfaction survey.
Improving Job Quality by Increasing Wages and Training
The Nursing Home Quality Initiative had a dramatic impact on Massachusetts’ nursing homes and their
workers. The wage pass-through allocated funds provided through Medicaid reimbursement for the express
purpose of increasing compensation for direct care workers. This resulted in a 15% increase in CNAs
median hourly wage from $10.22 in 2000 to $11.73 in 2003.
ECCLI was a career pathway program for CNAs and home health aides with the primary goal of enhancing
the quality and outcomes of resident/client care while simultaneously addressing the dual problems of
recruiting and retaining a skilled direct care workforce. From 2000-2010, 9,000 frontline staff and managers
from over 175 facilities participated in ECCLI training activities. Evaluation of the program demonstrated
that opportunities for education and career advancement improved frontline workers’ sense of self-
condence and respect which led to improvements in the quality of resident/client care. For example,
results showed that the rate of worsening behavioral symptoms were signicantly reduced among resident
in nursing home that participated in ECCLI, compared to those that did not participate (Commonwealth
Corporation, 2007). Supervisory training fostered an environment of trust and respect which signicantly
impacted staff satisfaction. Providing English as a Second Language (ESL), adult basic education (ABE) and
career readiness courses enabled more staff to develop the needed basic skills to pursue post-secondary
education. In many cases, staff advanced from CNA to a LPN or RN thereby securing a family-sustaining
wage. Finally, offering career ladders and training opportunities made organizations more attractive to
potential new employees thereby improving staff recruitment efforts.

Page 12
Increasing Supply of CNAs
The Direct Care Scholarship Program was designed to increase the supply of direct care workers. From
2001-2008, the program provided free training and state certication to 3,800 people enabling them to
work as CNAs and home health aides in nursing homes and community settings across the state. Program
outreach and free training removed barriers for those who could not otherwise afford the cost of training.
It also provided people with the credentials needed to access a stable career with opportunities for
professional growth.
Increased Satisfaction with Nursing Homes
As part of the Legislature’s investment in the Nursing Home Quality Initiative, the Massachusetts Department
of Public Health measured consumer satisfaction of family members with relatives in the Commonwealth’s
nursing homes. In 2004, after four years of investment, the statewide survey found an exceptionally high
degree of satisfaction with the care their loved ones received. By 2007, nine out of ten surveyed said
they would recommend their loved one’s nursing home to a friend or family member (Massachusetts
Department of Public Health, 2007).
Ultimately, the Nursing Home Quality Initiative demonstrated that adequate and sustained state investment
in nursing homes and their staff resulted in higher quality nursing home care for residents and families as
well as higher quality jobs and increased opportunities for frontline caregivers. From 2000-2005, CNA
vacancy rates dropped 40% from 15% to 9% and the use of temporary agency staff dropped by 78%. At
the same time, CNA retention rates improved by 16% which resulted in 78% of full-time CNAs maintaining
employment at the same nursing home for 12 months or more (MSCA, 2000-2005). ECCLI has since
gone on to become a national model for workforce development, promoting public-private partnerships to
strengthen the long term care workforce and improve the quality of long term care services.
Recommendations
It is imperative that the state increase its investment in nursing homes across the Commonwealth. The
quality of resident care and the quality of jobs depends on it. Massachusetts Senior Care Association offers
the following recommendations.
Create a Pathway to a Living Wage
CNAs and ancillary staff earn some of the lowest wages in the state, and even with Massachusetts' universal
health care law, many struggle to afford adequate health coverage for themselves and their families.
Creating a pathway to a living wage for these workers will ensure a decent wage that supports their families
and helps stabilize the workforce caring for frail elders and people with disabilities in nursing homes across
the Commonwealth. Similar to Governor Charlie Baker’s commitment to providing a $15 per hour starting
wage for Personal Care Attendants (PCAs) in 2018, MassHealth should establish a pathway to a living wage
for nursing home CNAs and ancillary staff.
The state should develop a multi-year strategy that utilizes an annual wage pass-through that both
incrementally raises wages in a signicant manner and takes into consideration the regional wage variation
that exist in the state. To ensure continued progress, it should create a mechanism to enable the state to
fund yearly wage updates consistent with the Consumer Price Index (CPI).

Page 13
Support a Culture of Retention
In January 2015, the Health Workforce Research Center on Long-Term Care at the University of California
San Francisco recommended increasing national and state investments in education and training as a
means to improve direct care worker recruitment and retention. Both the Institute of Medicine (2004)
and Massachusetts ECCLI ndings indicate supervisory training positively impacts job satisfaction, feelings
of respect and value and overall retention rates for all direct care workers. Training nurse managers to
become better supervisors and leaders is necessary to create an organizational culture of retention for
all staff.
The state should support the rollout and implementation of comprehensive evidence-based supervisory
training for the express purpose of retaining staff and reducing turnover. Using a train-the-trainer model,
employers will increase the knowledge, skills and attitudes managers need to support staff stability and
reduce turnover, foundationally supporting this key component of quality jobs.
Establish a CNA Scholarship Program
Throughout the state, a signicant number of individuals, including nursing home ancillary staff (dietary,
laundry and housekeeping), aspire to become CNAs but do not have the language or literacy skills
necessary to enter into a training program. Many work multiple jobs while attending ABE or ESL programs
to improve their English and numeracy skills. Their progress is typically measured in years. To increase the
supply of CNAs, it is recommended the state fund a CNA Scholarship Program that supports more adults
in their quest for post-secondary credentials by providing integrated ABE/ESL with CNA training. The
Integrated Basic Education and Skills Training (I-BEST) is a national model developed in Washington state
that accelerates the pathway to higher level employment by bridging technical skills and language literacy
teaching. Scholarship funds should be used to offset the cost of training as well as provide stipends to adult
learners so they can reduce the number of work hours to concentrate on completing the I-BEST program
in an expedited amount of time.

Page 14
Sources
American Health Care Association, (2009). Improving Staff Satisfaction: What Nursing Home Leaders are Doing.
Retrieved from http://www.ahcancal.org/facility_operations/workforce/documents/staffsatisfaction.pdf
Barbarotta, Linda. (2010). Direct Care Worker Retention: Strategies for Success. Institute for the Future of
Aging Services. Retrieved from http://www.leadingage.org/uploadedFiles/Content/About/Center_for_Applied_
Research/Publications_and_Products/Direct%20Care%20Workers%20Report%20%20FINAL%20(2).pdf
Castle, Nicholas G, and John Engberg, (2007) “The Inuence of Stafng Characteristics on Quality of Care in
Nursing Homes.” Health Services Research 42.5 (2007): 1822–1847.
Child Care Aware, (2014). Parents and the High Cost of Childcare: 2014 Report. Retrieved from http://www.usa.
childcareaware.org/advocacy/reports-research/costofcare/
CliftonLarsonAllen LLP, (2012). Mapping the Future: Estimating Massachusetts Aging-Services Needs 2010-2030.
Commissioned by the Massachusetts Senior Care Association.
Crittenton Women’s Union, (2013). Economic Independence Calculator. Accessed from website on November
5, 2015. http://www.liveworkthrive.org/research_and_tools/economic_independence_calculator
Dawson, Steven L., and Rick Surpin, (2001). Direct Care Healthcare Workforce: The unnecessary crisis in long
term care. Aspen Institute.
Dill, Janette S.; Morgan, Jennifer Craft; & Kalleberg, Arne L., (2012). Making Bad Jobs Better: The Case of Frontline
Health Care Workers. In Warhurst, Chris, Carre, Françoise, Findlay, Patricia, Tilly, Chris, Lloyd, Caroline, Smith,
Chris & Warhurst, Chris (Eds.), Are Bad Jobs Inevitable?: Trends, Determinants and Responses to Job Quality in
the Twenty-First Century (pp. 110-27). New York: Palgrave.
Eaton, Susan, et al., (2001). Extended Care Career Ladder Initiative (ECCLI): Baseline Evaluation Report of a
Massachusetts Nursing Home Initiative. Harvard Business School.
Frogner, B. and Spetz, J., (2015). Entry and Exit of Workers in Long-Term Care. San Francisco, CA: UCSF Health
Workforce Research Center on Long-Term Care. Retrieved from: http://healthworkforce.ucsf.edu/sites/
healthworkforce.ucsf.edu/les/Report-Entry_and_Exit_of_Workers_in_Long-Term_Care.pdf
Heineman, Janice M, et al., (2007). The Qualitative Evaluation of ECCLI. Commonwealth Corporation Research
and Evaluation Brief, volume 5, issue 2. Retrieved from http://www.leadingage.org/uploadedFiles/Content/About/
Center_for_Applied_Research/Publications_and_Products/ECCLI_Qualititative_Brief.pdf
Institute for the Future of Aging Services, (2007). Extended Care Career Ladder Initiative (ECCLI) Qualitative
Evaluation Project Final Report. Prepared for Commonwealth Corporation. Retrieved from http://www.
leadingage.org/uploadedFiles/Content/About/Center_for_Applied_Research/Center_for_Applied_Research_
Initiatives/ECCLI_Final_Report.pdf
Institute for the Future of Aging Services, (January 2007). The Long-Term Care Workforce: Can the Crisis Be
Fixed? Retrieved from http://phinational.org/research-reports/long-term-care-workforce-can-crisis-be-xed

Page 15
Institute of Medicine, (2008). Retooling for an Aging America: Building the Healthcare Workforce. Retrieved
from http://iom.nationalacademies.org/en/Reports/2008/Retooling-for-an-Aging-America-Building-the-Health-
Care-Workforce.aspx
Massachusetts Department of Public Health, (2007). Nursing Home Survey Results.
Massachusetts Department of Public Health, (2015). Nursing Assistant Program Analysis.
Massachusetts Senior Care Association, (2000-2015). Annual Employer Wage Survey Results. Waltham,
Massachusetts.
National Low Income Housing Coalition. Retrieved from report entitled: Out of Reach 2013.
National Research Corporation, (2012). 2011-12 National Survey on Customer and Employee Satisfaction
in Nursing Homes. Retrieved from http://www.ahcancal.org/research_data/stafng/documents/snf_
nationalreport2012.pdf
PHI PolicyWorks, (2015). Paying the Price: How Poverty Wages Undermine Home Care in America. Retrieved
from www.PHInational.org/payingtheprice
PHI and Institute for the Future of Aging Services, (2003). State Wage Pass-Through Legislation: An Analysis.
Workforce Strategies, no. 1. Retrieved from http://phinational.org/research-reports/state-wage-pass-through-
legislation-analysis
Plumb, Scott, (2001). Where Will Your Mother Go?: A special report on the crisis engulng nursing homes in
Massachusetts and its implications for the care of our frail elders and disabled citizens. Massachusetts Extended
Care Federation.
Seavey, Dorie, (2004). Better Jobs Better Care Practice Policy Report: The Cost of Frontline Turnover in Long-
Term Care. Retrieved from http://phinational.org/research-reports/cost-frontline-turnover-long-term-care
Stone, Robin I., (2008). The Origins of Better Jobs Better Care. The Gerontologist. Vol 48. Special Issue 1, 5-13.
United States Census Bureau, (2010). American Community Survey. https://www.census.gov/programs-surveys/
acs/data.html
Wilson, Randall, (2006). Invisible No Longer: Advancing the Entry-level Workforce in Health Care. Jobs for the
Future. Retrieved from http://www.jff.org/publications/invisible-no-longer-advancing-entry-level-workforce-health-
care
Zacker, Heather B., (2011). Jobs to Careers Practice Brief: Creating Career Pathways for Frontline Health Care
Workers. Retrieved from http://www.jff.org/sites/default/les/publications/J2C_CareerPathways_011011.pdf

Page 16
Appendix
2015 Median Hourly Wages by County
Source: Mass Senior Care Association Annual Employment Survey, 2015

800 South Street, Suite 280, Waltham, MA 02453
Tel: 617.558.0202 Fax: 617.558.3546 1.800.CARE FOR
www.maseniorcare.org
