
Florida Mobile
Integrated Healthcare
Community Paramedicine
Program Guidebook

2
F l o r i d a Mo b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
CREDITS
Ariella Bak Christine Long
Rich Barner Mac Kemp
Jane Bedford Mark Matthews
Juan Cardona Steve McCoy
Wendy Crews Melissa McNally
James Crutcheld John McNamara
Orlando Dominguez, Jr. Scott Moore
Richard Ellis Jerri Regan
Timothy Ewing Daniel Swayze
Joe Goodwin
Evan Weiner
Mike Hall
Lauren Young
Don Hughes
Matt Zavadsky
Linda Liebert-Hall
Integrated Mobile Healthcare Coordinator,
Gainesville Fire Rescue
Community Health Resource Program Coordinator,
Brevard County Fire Rescue
People and organizations who provided assistance or contributed to the Guidebook
EMS Manager,
Highlands County EMS
Deputy Chief of Clinical Affairs,
Leon County Emergency Medical Services
Director of Education and Clinical Services,
Nature Coast Emergency Medical Services
Chief,
Jefferson County EMS
EMS Division Chief,
Coral Springs Fire Department
State of Florida
EMS Administrator
Area Supervisor,
Excelsior Ambulance
Mobile Integrated Healthcare PA,
AMR
Director of Community Paramedicine,
Manatee County Public Safety
Fire Chief,
Sunrise Rescue
Assistant Chief of EMS Operations,
Brevard County Fire Rescue
EMS Resource
Advisors, LLC
Chief of EMS,
Palm Beach County Fire Rescue
Owner,
Health Services Consulting
Community Paramedic,
Sunrise Rescue
Vice-President and COO, Center for Emergency
Medicine of Western Pennsylvania & Project Manager
of CONNECT Community Paramedicine Program
Ambulance Systems Service Director,
Coastal Health Systems of Brevard
EMS Coordinator,
Seminole Tribe Fire Department
CEO,
Nature Coast Emergency Medical Services
Mobile Integrated Health Medical Social Work
Coordinator, Palm Beach County Fire Rescue
Fire Chief,
Satellite Beach Fire Department
Chief Strategic Integration Ocer,
MedStar Mobile Healthcare
President,
Liebert-Hall & Associates, LLC

Chapter 2
What’s Need Got to
Do with It?
3
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
TABLE OF CONTENTS
Chapter 3
24
Stakeholders
A. Template Outline for Business Plan
B. Template Budget
C. Template Memorandum of Agreement (MOA)
D. Template Organizational Chart
E. Template Marketing Plan
F. Template Patient/Client Satisfaction Survey
G. Template Performance-Based Job Description
H. Sample Mobile Integrated Healthcare Provider Referral Entry into Care
I. Sample Mobile Integrated Healthcare Provider Initial Contact Form
J. Example Palm Beach County MIH Pilot Program
04
Introduction
The purpose of this Guidebook is to do
just that – guide you
30
Chapter 4
Developing Your Program Plan
Chapter 5
44
Developing Your Program Budget
53
Chapter 6
What Difference Did You Make?
62
Chapter 7
Sustaining Your Program
66
Chapter 8
Tying It All Together
Chapter 1
Mobile Integrated
Healthcare – Community
Paramedicine
(MIH-CP), Models, and
Legal Considerations
05
18
Manatee County Florida Community Paramedicine Manatee County Florida Community Paramedicine
Manatee County Florida Community Paramedicine
APPENDIX
78

INTRODUCTION
4
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
The purpose of this Guidebook is to do just that – guide you through the research, analysis, planning, development, and successful
launch of your own customized Florida Mobile Integrated Healthcare – Community Paramedicine (MIH-CP) Program. This resource
is straight-forward and easy to read. In addition to guidance, it provides recommendations and lessons learned from MIH-CP
programs in Florida, advice from experts across the country, with expanded resources and templates.
This Guidebook is not designed to tell you what you must do,
but to provide suggestions and ideas on what to consider in
developing your own MIH-CP. As you read it, remember that
not all the information in the Guidebook will apply to you or
your organization. Use it to think through the elements of
your program and remember that a successful program must
be anchored in your community.
The Guidebook is organized linearly – take each step by step,
so you end up with an operational program. However, it is
strongly recommended that you use the Budget Template
found in Appendix B as you work through the chapters. You
will be prompted to insert nancial information into the
budget throughout the Guidebook. So, as you develop your
program, enter even the most basic information on your costs
and revenue.
Entering your cost and revenue information will help you when you get to Chapter 5 where you’ll complete your program budget.
(Yes, even if all your revenue is through your organization, you will need to develop a budget to help you get initial support for
your MIH-CP and monitor the sustainability of your program.)
The authors of this Guidebook conducted interviews with
eleven organizations who operate MIH-CP Programs in
Florida. During the interviews we asked questions about why
they started their MIH-CP, how they did it, the funding used,
the challenges they faced, what changes they would make in
their implementation, and what advice they would give to an
organization wanting to begin a MIH-CP. We have integrated
their experiences, thoughts, and advice into this Guidebook to
help you identify what will work in your community.
As the vision of your program becomes clearer, reect on
what you’ve done and evaluate if there are things you need to
do differently. Also, look for the ripple effect. For example,
changing something in the stang may impact the medical
direction, or the expense of a staff member, or how you reach
your target market. A change in almost any piece will make a
difference in your budget.
Chapter 8 is the culmination of the steps presented in the Guidebook. This Chapter presents a case study illustrating the material
we covered and is meant to provide ideas on the content and format of a business plan for the design and implementation of a
MIH-CP program in Florida. We hope this Guidebook proves useful and encourages you to think about how a MIH-CP Program can
transform your community and the people you serve.
Realize you’re not going to change things
overnight. Create a culture. This is a
marathon, not a sprint.
Don Hughes
Overall, this is the future of not only
healthcare, but of EMS. By evolving the
paramedicine profession into more of
a clinician role, EMS will no longer be
merely a transportation benefit.
Melissa McNally

5
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
This Chapter provides denitions and descriptions of different types of Mobile Integrated Healthcare - Community Paramedicine
Programs and reviews Florida statutes that regulate the practice of a community paramedic.
What is Mobile Integrated Healthcare – Community Paramedicine?
This question was answered by the National Association of Emergency Medical Technicians (NAEMTs) in the introduction to their
report on the Mobile Integrated Healthcare and Community Paramedicine 2nd National Survey, a link to which is included in the
references and resources at the end of this Chapter. Their denition is as follows:
CHAPTER 1
Wrap your head completely around the
CP program – have a solid understanding
of the program before starting.
Juan Cardona
Mobile Integrated Healthcare - Community Paramedicine,
Models, and Legal Considerations
Mobile integrated healthcare - community paramedicine (MIH-CP) is the provision of healthcare
using patient-centered, mobile resources in the out-of-hospital environment. MIH-CP is provided by a
wide array of healthcare entities and practitioners that are administratively or clinically integrated
with EMS agencies, while CP is one or more services provided by EMS agencies and practitioners
that are administratively or clinically integrated with other healthcare entities.
The NAEMT report goes on to describe
the range of services provided by MIP-
CP programs as including:
• Sending EMTs, paramedics or
community paramedics into the
homes of patients to help with
chronic disease management and
education, or post-hospital discharge
follow-up to prevent hospital
admissions or readmissions.
• Navigating patients to destinations
such as primary care, urgent care,
mental health or substance abuse
treatment centers instead of
emergency departments to avoid
costly, unnecessary hospital visits.
• Providing telephone triage, advice
or other assistance to non-urgent
911 callers instead of sending an
ambulance crew.
• Using telemedicine technology
to facilitate interactions between
patients in their home and medical
professionals in hospitals or other
locations.
Given the inclusive nature of the
NAEMT’s denition of MIH-CP and the
broad nature of the types of services
they provide, it is safe to say, there is no
one model for MIH-CP Programs. The
best model is the one that works in your
community.
Manatee County Florida Community Paramedicine
Learn about what is
happening nationally and get
out of the area to see what’s
going on.
Juan Cardona
C h a p t e r 0 1

6
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Across the nation, 78% of respondents to the NAEMT survey
indicated their model was focused on preventing hospital
readmissions for conditions that have hospital penalties such
as chronic lung disease, coronary artery bypass graft surgery,
heart attacks, heart failure, hip and knee replacements, and
pneumonia. Frequent EMS and emergency department users
were targeted by 78% of survey respondents. The respondents
were able to report multiple targets, so the percentage of
respondents is more than 100%.
Chronic disease management for conditions such as congestive
heart failure, hypertension, COPD, asthma, and diabetes was
targeted by 68% of respondents. The fourth area targeted
by MIH-CP Programs was assessment and navigation to
alternative destinations that was reported by 50% of the
respondents. Home health support was cited by 45% of
respondents, and 45% of respondents indicated they were a
primary care/physician extender model.
The remainder reported their target areas as hospice support
(20%), 911 Nurse Triage (7%), and 11% reported other target
areas that included wound care, knee replacement follow-up,
and mental health crisis screening and navigation.
1.
Abbeville County’s Community Paramedic Program
Updated/reviewed May 2018
• Need: To reduce non-emergent visits to the
emergency department as well as inpatient stays in
rural South Carolina.
• Intervention: A community paramedic program
was started in Abbeville County, providing in-home
preventive care to patients.
• Results: Emergency room visits have decreased by
58.7%, and inpatient stays by 60%. Many patients
previously needing consistent services now only
need occasional check-ups.
2. Livingston County Help For Seniors
Updated/reviewed January 2018
• Need: Meeting the health needs of geriatric patients
in rural Livingston County, New York.
• Intervention: The Help for Seniors program was
developed and using its vodcasts, local EMTs were
trained in geriatric screening methods and health
needs treatment.
• Results: In addition to developing a successful model
for educating EMS personnel, the program screened
over 1,200 individuals and identied various risks
among the geriatric population.
The Rural Health Information Hub (RHI Hub) assembled examples of rural MIH-CP Program models. The programs are described
along three parameters, need, intervention, and results. The following information may be found at
https://www.ruralhealthinfo.org/project-examples/topics/community-paramedics
and was taken directly from the RHI Hub website.
Monkey Business Images/Shutterstock.com
C h a p t e r 0 1

7
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
3. Rugby Community Paramedic Program
Added November 2017
• Need: Low patient volumes, a shortage of EMS
volunteers, and an aging population in a 5-county
North Dakota region required a change in the way
the Rugby EMS team delivered care.
• Intervention: Through the Rugby Community
Paramedic Program, EMS staff bring medical care
to patients transitioning back into their homes,
including those with chronic conditions and hospice
patients.
• Results: The program’s early intervention methods
helped reduce the number of emergency room
admissions and the escalation of medical conditions.
Patient satisfaction has improved, and the program
has gained the trust of patients and medical staff in
Rugby and surrounding areas.
4. Eagle County Community Paramedic
Updated/reviewed February 2017
• Need: Rural areas nationwide have shortages of
primary care providers and home health programs.
• Intervention: Eagle County Paramedic Services is
utilizing community paramedics in the provision
of non-acute home care and assistance with
immunizations and screenings in rural areas where it
is dicult for these services to be accessed.
• Results: The pilot program was featured at the
2010 International Roundtable on Community
Paramedicine. After 18 months of implementing the
program, a net total of $288,028 in healthcare costs
was saved
• 9-1-1 Nurse Triage
• “EMS Loyalty” Program
• Readmission Avoidance
• Hospice Revocation Avoidance
• Observation Admission Avoidance
• Home Health Partnership
A helpful MIH-CP summary reference is the National
Rural Health Association Policy Brief titled: Principles for
Community Paramedicine Programs. Other resources include
two texts titled Mobile Integrated Healthcare: Approach to
Implementation (2016) and Community Health Paramedicine
(2018). References for these resources are located at the end
of this Chapter.
An example of an urban MIH-CP program is MedStar Mobile.
They serve the Fort Worth Texas area and 14 surrounding cities
and are considered a municipal governmental agency (public
utility model). The MedStar service area covers 421 square
miles and is home to almost 1 million residents. With a budget
of $40 million, it employs approximately 460 employees and
provides 125,000 responses annually.
Operating a MIH-CP Program since 2009, the initial focus
of MedStar’s program was on high system users for whom
individual care plans were developed. These care plans
included scheduled home visits with follow up with the client’s
primary care provider. Current programs are described as
Patient Navigation Models and Mobile Integrated Healthcare
models.
. As reported by MedStar and available at their website:
http://www.medstar911.org/mobile-healthcare-programs
their models now include:
C h a p t e r 0 1

Delivery Model
Florida MIH-CP
Survey Respondents
2017
N=11
NAEMT National Survey
Respondents
2018
N=129
Public, Fire-based 55% 33%
Public, Municipal, County, or Regional 9% 21%
Public, Hospital Based 0 8%
Private, Nonprot 9% 11%
Private, For-Prot 9% 11%
Private, Hospital-based 9% 16%
Tribal 9% 0
8
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
For purposes of this document, the terms Community Paramedicine Program and Mobile Integrated Healthcare are used together
and referred to as MIH-CP.
Florida’s MIH-CP
Consistent with the NAEMT’s denition
of MIH-CP, the Access to Care
Committee of the Florida Emergency
Medical Services Advisory Council has
dened Mobile Integrated Healthcare -
Community Paramedicine (MIH-CP) as:
Findings from the recently completed
survey of eleven Florida MIH-CP
programs who self-reported operating a
MIH-CP program, one respondent made
the distinction between a community
paramedic program and a mobile
integrated healthcare program. This
interviewee felt that Mobile Integrated
Healthcare is a more inclusive term
recognizing the contributions of other
professionals working with paramedics
on multidisciplinary teams. When asked
to choose if they were a Community
Paramedicine Program or Mobile
Integrated Health Healthcare Program,
70% of the respondents to the NAEMT
survey categorized their program as
“Community Paramedicine” and 31%
self-described as offering “Mobile
Integrated Healthcare” services.
Using the data from the previously
described survey of Florida’s MIH-
CP programs, Table 1 presents the
distribution of Florida’s programs by
delivery model comparing it to the
NAEMT national survey.
Table 1: Comparison of the Distribution of Florida MIH-CP Programs to MIH-CP Programs by Type of Delivery Model
The provision of healthcare using patient-centered, mobile resources in the out-of-
hospital environment. MIH -CP is provided by a wide array of healthcare entities and
practitioners that are administratively or clinically integrated with EMS agencies and or
other healthcare entities.
C h a p t e r 0 1

9
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Model 1 – Private for Prot Model 2 – Public Fire Model 3 – Private Non Prot
Focus / Goal
Provide access to concierge
medicine to all in the community.
Primarily the reduction in frequent yers
Reduce COPD / CHF
readmissions to hospital
within 90 day period
Services
24/7 operation
Provide telehealth services,
including medical evaluations and
rapid on-site testing.
Advocacy; resource identication/referral
education; safety/home
assessment; chronic disease
management
Home visits: vital signs,
appearance, medication
reconciliation, and health
safety checks
Stang
1 FTE Paramedic is dedicated to
the
program, ½ FTE using overtime or
part-time Paramedics.
Varies by size of department and services
provided: Some programs have no
Paramedic because the only focus is on
advocacy and resource navigation, not
direct medical care. Others have up to 3
FTE Paramedics with CP coordinators and
administrative support. Some also utilize
volunteers, such as medical and pharmacy
school interns to support program, and
people to provide client transportation to
address any unmet needs.
1 FTE Paramedic
Partners
Hospice;
Fire Department for
part-time stang
Hospice; Senior Centers; Transportation
organizations; Home Health Care; Police;
Social Service; Public Health; Mental
Health; Homeowners Associations; Nursing
Homes; Visiting Nurses; Primary Care
Professionals; Pharmacies; 211 Resources;
TOPS; Veterans Clinic; Hospitals; Insurance
companies; Food pantries; Homeless
shelters; Churches; Civic organizations;
Local government; Education institutions;
Department of Children & Family Services
Hospitals; Police; Fire; Social
Service agencies
Funding
Start-up: All internal funding Start-up: Grants and internal funding Start-up: Internal funding
Ongoing: 100% self-pay. Collect
monies up front, no insurance
billing.
Ongoing: Internal and some grants
Ongoing: 100% self-pay through the
hospital
Metrics Social Media talk
Reduction in 911 calls; Alignment with
resources and/or primary care physician;
Savings/Cost avoidance; Patient health
improvement; Patient satisfaction survey;
Medication compliance; length of program
stay; ER visits; Average ambulance
transportation cost; Provider satisfaction;
Readmission rates; Ambulance hospital
diversion; Pre and post Quality of Life and
Activities of Daily Living indicators
Hospital tracks COPD / CHF
readmissions
Florida Models
Of the 11 MIH-CP programs interviewed in the state of Florida, there are 11 different models. Each one has a unique format,
focus, operations, and funding. Table 2 displays characteristics of selected Florida models.
C h a p t e r 0 1
Table 2: Characteristics of Selected Florida Models

10
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Greatest challenge was…identifying and knowing
where to find resources to help your clients.
Ariella Bak
Medical Direction
NAEMT’s Mobile Integrated
Healthcare and Community
Paramedicine (MIH-CP) 2nd
National Survey asked the 129
MIH-CP programs across the
country about the role the
medical director played in their
program. Protocol development
was the most given response
at 88%, followed by quality
assurance at 78%, immediate
online medical direction 54%,
continuing education 53%,
development and support of care
plans 50%, initial training was
also 50%, and healthcare system
integration was 40%. Looking at
these responsibilities, you can
see why the selection of the right
medical director is so important
to your program.
Under Florida statute 401.265,
EMS services are required to
provide emergency care under
the license and direction of a
physician medical director. The
medical director supervises
and is directly responsible
for the medical performance
of the EMT’s and paramedics
performing the medical
procedures in the eld. They are
required to advise, consult, train,
counsel, and oversee the delivery
of services, including maintaining
quality assurance processes.
As previously mentioned,
paramedics and EMT’s may
perform health promotion and
wellness activities including
blood pressure screenings in
a nonemergency environment
within the scope of their training,
and under the direction of a
medical director. The medical
director may provide this
direction outside of the provision
of emergency care and is liable
for any act or omission of any
EMT or paramedic acting under
his/her supervision and control
when performing these services.
The selection of your medical
director is crucial. Look for your
medical director early in your
MIH-CP development process.
This early engagement will help
you establish strong standard
operating procedures and
protocols with effective quality
These models give you a cross-section of
just how different your program can be
based on the identied need, the focus
of your program, and the community
resources available to support it.
City of Gainesville Florida Community Paramedicine
C h a p t e r 0 1

11
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
be used for both EMS and MIH-CP programs. In the
references and resources section of this Chapter, there
are possible provisions to be included in a medical
director’s contract as well as an interview guide to help
you gauge your medical director’s level of commitment
to and understanding of MIH-CP.
Encourage your medical director to be involved with the
Florida EMS Advisory Council and the Florida Association
of EMS Medical Directors. Additional information about
these groups is found in the references and resources
section at the end of this Chapter.
Finally, in addition to a dedicated medical director, you
may want to use other providers for medical direction,
advice, or consultation based upon the design of
your program. For instance, a person’s primary care
physician or a specialty physician may provide that
direction for a specic client.
Hospital Flexibility (Flex) Program Workplan. A brief
description of selected documents follows providing a
list of potential focus areas for MIH-CP Programs.
Florida’s SHIP identies goals for the state’s public
health system in 8 priority areas that include:
• Health Equity
• Maternal & Child Health
• Immunizations
• Injury, Safety & Violence
• Healthy Weight, Nutrition & Physical Activity
• Behavioral Health both Mental Illness and
Substance Abuse
• Sexually Transmitted Disease (STDs) as well as other
infectious diseases
• Chronic Diseases and Conditions, including
tobacco-related illnesses and cancer
Budget Note: Insert the annual cost of your MIH-CP medical director into the expense line “medical direction
contract fees.” If your MIH-CP medical director is also your medical director for emergency operations, only
include the additional cost for the responsibilities of a MIH-CP program, if any.
control processes, enabling you to identify problem
areas early in the development process.
The medical director should understand the latest
approaches to healthcare being promoted and
evaluate the healthcare trends and service gaps
in your community. You need someone who will
wholeheartedly support the idea of a MIH-CP Program
and be an active participant in the development and
ongoing champion in support of it. One organization
that responded to the interview about their MIH-CP
stressed the importance of medical direction and
of nding a medical director who is open to and
comfortable with paramedics doing things outside of
the traditional “paramedic” duties.
And, if your current EMS medical director does not
meet these criteria, you may select a different medical
director for your MIH-CP program. While it is unusual,
there is no requirement that the same medical director
Alignment
MIH-CP Programs offer cost-effective and ecient
solutions to perennial issues challenging not only
Florida’s healthcare system but our nation’s. MIH-CP
Programs target the medically underserved who suffer
from debilitating conditions that are not only caused by
acute conditions (trauma, infectious diseases) but from
chronic diseases that often require on-going care and
treatment. Successful disease prevention and wellness/
health promotion are grounded in community-wide
interventions. Your local health department is the
organization charged with improving the health of the
county’s population and working with them on common
problems is a cost-effective approach.
MIH-CP Programs have a vital role in achieving the
Florida Department of Health’s (FDOH) Strategic
Plan, the State Health Improvement Plan (SHIP), your
county’s Community Health Improvement Plan (CHIP),
the Florida Department of Health, Emergency Medical
Services State Plan 2016 – 2021, and the Medicare Rural
These goals are further dened by strategies and objectives. A theme throughout the goals, strategies, and
objectives is that goal achievement rests on the collaboration and active engagement of state, local and other multi-
level organizations. The SHIPs goals address persistent issues challenging Florida’s healthcare system that demand
a collaborative response. In this way, resources are leveraged, redundancies eliminated, and problems solved.
C h a p t e r 0 1

12
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
The Florida Department of Health, Bureau of
Emergency Medical Oversight (BEMO), Emergency
Medical Services published the Emergency Medical
Services State Plan (EMSSP), 2016-2021.
The EMSSP identied ve strategic priority areas, each
with an articulated goal/s:
■ Strategic Priority 1: EMS Industry Health and Safety
□ Goal 1.0: Ensure a commitment to the health and
safety of the EMS industry and the citizens and
visitors of Florida
■ Strategic Priority 2: Clinical and Operational
Performance
□ Goal 2.0: Use health information technology to
improve the eciency, effectiveness, and quality
of patient care coordination and health care
outcomes
■ Strategic Priority 3: EMS System Infrastructure and
Finance
□ Goal 3.1: Attract, recruit and retain a prepared,
diverse and sustainable EMS workforce in all
geographic areas of Florida
□ Goal 3.2: Establish a nancially sustainable
infrastructure, which includes processes and
effective use of technology and communication
supporting all EMS systems functions
■ Strategic Priority 4: Readiness for Emerging Health
Threats
□ Goal 4.0: Demonstrate EMS readiness for emerging
health threats and natural or manmade disasters
■ Strategic Priority 5: Community Redevelopment and
Partnerships
□ Goal 5.0: Integrate EMS with health planning and
assessment processes to maximize community
partnerships and expertise in accomplishing its
goals
MIH-CP Programs and the Florida Department of Health Emergency Medical Services
State Plan 2016 - 2021
Photographee.eu/Shutterstock.com
C h a p t e r 0 1

13
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Each of the strategic priorities has strategies and objectives, and Strategic
Priority 5 explicitly references community paramedic (MIH-CP) programs. The
strategies and objectives for Strategic Priority 5 are as follows:
■ Strategy
□ Provide injury prevention programs to the public
□ Promote the increase of EMS agencies developing community
paramedic programs
□ Improve community health
■ Objectives
□ Increase the percentage of EMS agencies conducting fall prevention
programs from 28.5% to 40% by December 2018
□ Increase the percentage of EMS agencies conducting opioid use and
naloxone awareness programs from 13.5% to 35% by December 2018
□ Increase the percentage of EMS agencies conducting safety
programs sponsored or recommended by the Florida Department of
Transportation (FDOT) from 19.2% to 30% by December 2018
□ Increase the percentage of EMS agencies conducting drowning
prevention programs from 30% to 50% by December 2018
□ Increase the percentage of EMS agencies conducting programs to
reduce infant mortality from 18.5% to 30% by December 2018
□ Increase the percentage of EMS agencies offering cardiovascular health
and wellness programs pursuant to section 401.272, F.S., from 26.4% to
40% by December 2018
□ Increase the percentage of EMS agencies providing HIV health and
wellness programs pursuant to section 401.272, F.S., from 6.4% to 25%
by December 2018
□ Reduce the number of adult low acuity ED visits from 14.15% to 10% by
December 2018
□ Increase the number of EMS agencies with protocols that actively refer
children and adults for early intervention and treatment of mental
health disorders from 0 to 25 by December 2018
□ Increase the percentage of EMS agencies offering immunization
programs pursuant to section 401.272, F.S., from 6.4% to 25% by
December 2018
The following objectives included in the EMSSP are also included in the SHIP;
the information was taken directly from the EMSSP:
□ Increase the percentage of EMS agencies conducting fall prevention
programs from 28.5% to 40% by December 2018
□ Increase the percentage of EMS agencies conducting drowning
prevention programs from 30% to 50% by December 2018
□ Increase the percentage of EMS agencies conducting programs to
reduce infant mortality from 18.5% to 30% by December 2018
□ Increase the percentage of EMS agencies providing HIV health and
wellness programs pursuant to section 401.272, F.S., from 6.4% to 25%
by December 2018
□ Increase the percentage of EMS agencies offering immunization
programs pursuant to section 401.272, F.S., from 6.4% to 25% by
December 2018
Focusing on objectives that are found in both
SHIP and the EMSSP ensures your alignment
with Florida’s state initiatives.
If you are considering aligning your MIH-CP
with the SHIP and the EMSSP, developing
alliances with other community organizations
and groups working in these areas is an
important rst step.
For example, you may enter into a
Memorandum of Agreement with your local
health department to align your MIH-CP
program with the priority areas identied
in your county’s Health Improvement Plan.
If the area identied for improvement is
immunizations, you are in alignment with the
SHIP and the EMSSP.
A template for a Memorandum of Agreement is
included in Appendix C.
C h a p t e r 0 1
Manatee County Florida Community Paramedicine

14
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Florida established a Medicare Rural Hospital
Flexibility (Flex) Program that is funded by
the federal Oce of Rural Health Policy,
Department of Health and Human Services.
These federal funds are available to create rural
health networks, promote the regionalization
of rural health services and improve access to
healthcare for rural populations.
Flex Program areas are:
1. Quality improvement
2. Financial and operational improvement
3. Population health management and EMS
integration (optional)
4. Designation of Critical Access Hospitals
(required if requested)
5. Integration of innovative healthcare
models (optional)
The Florida Flex program is overseen by the Florida Department of Health.
In developing rural healthcare systems, the Flex program promotes
collaboration among rural providers, critical access hospitals (CAHs), and
emergency medical service (EMS) providers.
Annual work plans are developed and monitored to track success in the
required and selected optional program areas. Florida’s Flex Work Plan for
2017-18 includes three goals; two required and one optional. Under each
goal, there are activities that may be incorporated into a MIH-CP Program.
Adapted from the Florida Flex Plan and displayed below are the selected
goals, objectives, and activities that lend themselves to a MIH-CP Program:
■ Goal 1: Improve the quality of care provided by critical access
hospitals
□ Objective: Assist CAHs in implementing quality improvement
activities to improve patient outcomes
○ Activities:
» Improve patient safety in CAHs and the community by
ensuring all healthcare providers and eligible patient
populations receive their inuenza vaccinations.
» Improve transitions of care from CAHs to other healthcare
settings to improve patient outcomes
■ Goal 3a. To understand the community health and EMS needs of CAHs
□ Objective: Annually – Determine collective issues and trends in
population health management for CAHs
○ Activities:
» Conduct (participate) in assessments, identify needs,
establish improvement strategies
Another theme running through the documents described above is
that the goals, strategies, and objectives align with the national effort
spearheaded by the Institute of Healthcare Improvement (IHI). The IHI’s
Triple Aim calls for improving population health, improving the client’s care
experiences (including quality and satisfaction), and reducing per capita
healthcare costs.
Florida’s EMS service providers are rallying to meet these
challenges, and MIH-CP programs present a potential
intervention to effect system-wide change.
MIH-CP and the Flex Program
C h a p t e r 0 1
Manatee County Florida Community Paramedicine

15
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Chapter 1 References and Resources
1. NAEMT’s Mobile Integrated Healthcare and Community Paramedicine (MIH-CP) 2nd National Survey provides
current data on MIH-CP programs across the U.S. This includes start-up costs, target markets, services provided,
partnerships, stang, and payment. http://www.naemt.org/docs/default-source/2017-publication-docs/mih-cp-
survey-2018-04-12-2018-web-links-1.pdf?Status=Temp&sfvrsn=a741cb92_2
2. The Rural Health Information Hub provides information on rural health issues and MIH-CP programs.
Examples of rural MIH-CP models are found at https://www.ruralhealthinfo.org/project-examples/topics/
community-paramedics
3. National Rural Health Association, Policy Brief titled Principles for Community Paramedicine
Programs. Available at https://www.ruralhealthweb.org/getattachment/Advocate/Policy-Documents/
PrinciplesforCommunityParamedicineSept-2012.pdf.aspx?lang=en-US
4. The federal Oce of Rural Health Policy funded a study to look at the evidence base for community
paramedicine in rural communities. Their ndings evaluated delivery systems, challenges, and the role of state
Flex programs can play in supporting the development of these programs. Karen B. Pearson, MLIS, MA, John A.
Gale, MS, George Shaler, MPH, University of Maine, February 2014. Community Paramedicine in Rural Areas:
State and Local Findings and the Role of the State Flex Program. http://www.exmonitoring.org/wp-content/
uploads/2014/03/pb35.pdf
5. Zavadsky, M. and Hooten, D. 2016. Mobile Integrated Healthcare: Approach to Integration. Burlington, MA:
Jones & Bartlett Learning.
6. Pollack, A.N. (ed.) 2018. Community Health Paramedicine. Burlington, MA: Jones & Bartlett Learning.
7. MedStar Mobile. Information available at http://www.medstar911.org/
8. Florida Statutes and Community Paramedicine
The governing Florida laws for EMT’s and Paramedics are under Title XXIX Public Health, Chapter 401,
specically, Part III on Medical Transportation Services. The law cited for enabling Community Paramedicine is
Florida Statute 401.272(1)-(3), which states:
(1) The purpose of this section is to encourage more effective utilization of the skills of emergency
medical technicians and paramedics by enabling them to perform, in partnership with local county health
departments, specic additional healthcare tasks that are consistent with the public health and welfare.
(2) Notwithstanding any other provision of law to the contrary:
(a) Paramedics or emergency medical technicians may perform health promotion and wellness
activities and blood pressure screenings in a nonemergency environment, within the scope of their
training, and under the direction of a medical director. As used in this paragraph, the term “health
promotion and wellness” means the provision of public health programs pertaining to the prevention of
illness and injury.
(b) Paramedics may administer immunizations in a nonemergency environment, within the scope of
their training, and under the direction of a medical director. There must be a written agreement between
the paramedic’s medical director and the county health department located in each county in which
the paramedic administers immunizations. This agreement must establish the protocols, policies, and
procedures under which the paramedic must operate.
C h a p t e r 0 1

16
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Chapter 1 References and Resources
(3) Each medical director under whose direction a paramedic administers immunizations must verify and
document that the paramedic has received sucient training and experience to administer immunizations.
The verication must be documented on forms developed by the department, and the completed forms must
be maintained at the service location of the licensee and made available to the department upon request.
Florida Statutes Title XXIX Public Health: 401.272 Emergency medical services community healthcare.
http://www.leg.state..us/statutes/index.cfm?App_mode=Display_Statute&Search_String=medical%20
directors&URL=0400-0499/0401/Sections/0401.272.html
9. The Florida Statutes Title XXIX Public Health: 401.265 a description of medical directors is found at
http://www.leg.state..us/statutes/index.cfm?mode=View%20Statutes&SubMenu=1&App_mode=Display_
Statute&Search_String=medical+directors&URL=0400-0499/0401/Sections/0401.265.html
10. The Florida Administrative Code governing medical direction is 64J-1.004. It provides an outline of
provisions for a medical director’s contract:
• Name and relationship of the contracting parties.
• A list of contracted services inclusive of medical direction, administrative responsibilities, professional
membership, basic and advanced life support review responsibilities, and reporting requirements.
• Monetary consideration inclusive of fees, expenses, reimbursement, fringe benets, clerical assistance
and oce space.
• Termination clause.
• Renewal clause.
• Provision for liability coverage.
• Effective dates of the contract.
https://www.rules.org/gateway/ruleNo.asp?id=64J-1.004
11. The Health Insurance Portability and Accountability Act of 1996 (HIPAA) is a law impacting every aspect
of medical condentiality and is important to consider in developing a MIH-CP program. You can access it at
https://aspe.hhs.gov/report/health-insurance-portability-and-accountability-act-1996
12. For a deeper look at the legal issues based on the expanding roles health professionals play in CP programs,
this report by The Association of State and Territorial Health Ocials is a good analysis. James G. Hodge, Jr.,
JD, LLM, Daniel G. Orenstein, JD, Kim Weidenaar, JD, (2014). Expanding Roles of Emergency Medical Services
Providers: A Legal Analysis. http://www.astho.org/Preparedness/ASTHO-EMS-and-Law-Report/
13. Melody Glenn, Olivia Zoph, Kim Weidenaar, Leila Barraza, Warren Greco, Kylie Jenkins, Pooja Paode
& Jonathan Fisher (2017). State Regulation of Community Paramedicine Programs: A National Analysis,
Prehospital Emergency Care, 22:2, 244-251, DOI: 10.1080/10903127.2017.1371260, https://tandfonline.com/
doi/abs/10.1080/10903127.2017.1371260?journalCode=ipec20
14. Community Paramedicine Services by the Minnesota Department of Human Services
available at http://www.dhs.state.mn.us/main/idcplg?IdcService=GET_DYNAMIC_
CONVERSION&RevisionSelectionMethod=LatestReleased&dDocName=dhs16_177475
C h a p t e r 0 1

17
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Chapter 1 References and Resources
15. While this 2010 article is older, it provides a good overview of different MIH-CP services across the country
and discusses opportunities and challenges in the areas of funding, regulation, roles, education, medical
direction, stakeholders, and evaluations. Joint Committee on Rural Emergency Care, National Association
of State Emergency Medical Services Ocials, National Organization of State Oces of Rural Health. State
Perspectives Discussion Paper on Development of Community Paramedic Programs, December 2010.
http://www.nasemso.org/Projects/RuralEMS/documents/CPDiscussionPaper.pdf
16. Florida Department of Health, State Health Improvement Plan available at
http://www.oridahealth.gov/about-the-department-of-health/about-us/state-and-community-health-
assessment/ship-process/index.html
17. The Florida Department of Health Emergency Medical Services State Plan 2016-2021. http://www.
oridahealth.gov/provider-and-partner-resources/advisory-councils-stakeholder-groups/ems-advisory-council/_
documents/ems-strategic-plan.pdf
18. Florida Medicare Rural Hospital Flexibility (Flex) Program is available at
http://www.oridahealth.gov/programs-and-services/community-health/rural-health/index.html
19. Additional information about the IHI and its Triple Aim may be found on their website: http://www.ihi.org/
engage/initiatives/TripleAim/Pages/default.aspx and http://www.ihi.org/Topics/TripleAim/Pages/default.aspx.
20. The Journal of Emergency Medical Services has a Mobile Integrated Healthcare section. It’s a good way
to stay current on what’s happening in the industry: http://www.jems.com/adminstration-and-leadership/
community-paramedicine-and-mobile-healthcare.html?c=1
21. Sample Medical Director Interview Questions to determine their interest, passion, and involvement:
■ What do you know about the Mobile Integrated Healthcare / Community Paramedicine (MIH-CP) healthcare
models?
■ What do you see as the greatest unmet healthcare need in our community?
■ Under the Florida laws, paramedics work under the direction of a medical director, the MIH-CP model does not
change the paramedic’s scope of practice, but it does change the role of the paramedic. Are you comfortable with
this change in the role of the paramedic working under your license?
■ Are you interested in being the medical director for a MIH-CP program in our community?
■ Are you willing to be involved in the development of our MIH-CP program?
■ Are you willing to be a part of any presentation of our community program to potential stakeholders, clients, and
resource providers?
22. Florida Association of EMS Medical Directors: http://www.emlrc.org/faemsmd/about/
23. Florida EMS Advisory Council: http://www.oridahealth.gov/provider-and-partner-resources/advisory-
councils-stakeholder-groups/ems-advisory-council/
C h a p t e r 0 1

18
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k C h a p t e r 0 2
CHAPTER 2
What’s Need Got to Do With It?
Chapter 2 presents a discussion of need assessment that includes why agencies conduct needs assessment, what goes into a
needs assessment, and where to go to get the data to make a data-driven decision regarding areas for program development.
Do your research about legitimate CP
programs and travel to see how they
operate. Look for volume – is there a real
need to do the program?
Joe Goodwin
Manatee County Florida Community Paramedicine
Characteristics or variables you use to describe your
population are ones that are associated with access to
care and health status. Some of the variables associated
with access to care and health status include (but are not
limited to) emergency department utilization, frequency
of 9-1-1 calls, reasons for 9-1-1 calls, age, income,
educational level, the presence of disease (morbidity),
causes of death (mortality), self-perceived health status,
and the ability to carry out one’s activities of daily living.
If you answered “everything,” you’re on the right track!
The organized and purposeful examination of a group of
people (population) to identify new areas for program
design and implementation is a needs assessment. Using
data, you describe the population. Where the population
is located denes the geographical area that you are
serving or proposing to serve.
If you are a county-funded organization, the population
you serve may be legislatively dened as all residents of
the county. In this case, the county is your geographically
dened service area. Within that geographically dened
area, you may identify a population of interest (target
population) that may benet from a new program
(intervention).

19
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Data Sources
There are two basic data sources for a needs assessment, and these are data either internal to the organization or external
to the organization. Internal organizational data is your organization’s administrative data that includes client records
and billing data. According to the report summarizing the ndings from the NAEMT 2nd National Survey on Mobile
Integrated Healthcare and Community Paramedicine, the overwhelming majority (82%) of the current MIH-CP programs
across the country used their records to determine community needs. Table 3 was excerpted from the NAEMT report and
demonstrates the reliance on internal administrative data. Your organization’s administrative data is a valuable resource
that should be carefully reviewed and leveraged in your research. Be sure to seek data from potential stakeholders as it
will help them to relate to and ultimately, engage in the project.
In 2004 Florida created the
Emergency Medical Services
Tracking and Reporting System
(EMSTARS) that in turn participates
in the National EMS Information
System (NEMSIS). EMSTARS is a data
collection and analysis system that
captures incident-level data from
participating EMS providers.
The data may be used for
benchmarking to see how your
experience compares to other EMS
providers and for assessing process
and procedures that would benet
from a plan, do, act, check quality
management process. Several
EMSTARS’ data elements are helpful
when assessing the need for a MIH-
CP Program including reasons for
calls and whether a transport took
place.
Included in EMSTARS version 3.4
are questions regarding whether an
organization has MIH-CP protocols,
whether rural counties have MIH-
CP protocols, and the number of
community paramedic events.
Table 3: Data Sources
C h a p t e r 0 2
82%
EMS data
(such as from
electronic patient
care reports or
dispatch)
69%
Hospital
Admission/
Discharge
Data
63%
Population
Demographics
62%
Emergency
Department
Data
50%
Public Health
Data
22%
Utilization
Data From
One Or More
Ambulatory
Care Practices
10%
Other
09%
Law
Enforcement
Data
08%
Data From
Telephone
System (Acd,
Etc.)

20
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
■ Health Plans: Compare health plans on quality of care, member
satisfaction, coverage areas by county, accreditation status, and
claims payment performance. You can also compare monthly
health plan premium rate options and nd additional resources
on many health insurance topics.
■ Hospitals and Ambulatory Surgery Centers: View performance
and outcome data on selected medical conditions and
procedures in these types of health care facilities.
■ Emergency Room Care: Read educational information about
when and how to use an emergency room, what to do in a
medical crisis, alternatives to emergency room care and other
helpful information.
■ Prescription Drugs: View comparative prices at Florida
pharmacies for the top 100 most prescribed drugs in Florida.
You choose the county where you live and a drug you want
to price. The website displays the current price for most
pharmacies in your county.
Another source of information
and data is the Florida
Department of Health, Agency
for Health Care Administration’s
(AHCA) Florida Health Finder. As
noted on their website, there is
information that compares the
quality and cost performance of
hospitals, ambulatory surgery
centers, health plans, nursing
homes, and prescription drugs:
Of note for MIH-CP programs is the
emergency room data. For more
information about Florida Health Finder,
visit the website at
http://www.oridahealthnder.gov
C h a p t e r 0 2
Photographee.eu/Shutterstock.com

21
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Screenshot 1
Focus on the client’s needs and provide
empathetic, patient centered care.
Richard Ellis
When looking for external data,
the Florida Department of Health
Community Health Assessment
Resource Tool Set (CHARTS) is
one of the rst places to nd data
for your needs assessment. The
county is the unit of analysis in
the CHARTS data set. Your county
health department uses CHARTS
data to gauge the health of the
county and prioritize areas for
intervention and improvement.
The CHARTS website is located at
http://www.healthcharts.com/
charts/ChronicDiseases/default.
aspx.
Screenshot 1 is the Chronic
Disease report from the CHARTS
for Alachua County. If you cannot
read it, please go online, nd the
table, and take a minute to look
at it. There are some helpful
things to notice. Variables for
Alachua County are presented
as well as data for the State and,
also the U.S. Healthy People 2020
Goal.
These two columns provide
comparative data for Alachua
County so one may assess if the
indicator is “better” or “worse”
than the rest of the State, and
how well the county is doing in
accomplishing the U.S. Healthy
People 2020 Goal. By way of
review, the U.S. Healthy People
2020 Goal is a federal initiative
that establishes health-related
goals and monitors the health of
the U.S.
State and federal data provide useful benchmarks for comparison. When writing a grant application, funders want to know
what makes the population you propose to serve unique or worthy of funding. Given that poverty is a risk factor for poor
health, Alachua County would highlight the fact that their population has a higher proportion of individuals below the
poverty level. The rate for Florida is 16.1%, and the rate for Alachua County is 24.2%. The difference between your county’s
number, Florida’s number, and the Healthy People Goal is used to highlight inequities or gaps that exist. These inequities
point you to potential areas for intervention around which you may design and implement a MIH-CP.
C h a p t e r 0 2

Delivery Model Any County Florida U.S. Benchmark
Length of Life Ranked 60th
Premature Death 10,012 6,893 5,200
Poor Physical Health Days 4.4 3.7 2.5
Poor Mental Health Days 4.6 3.8 2.3
Health Behaviors Ranked 35th
Adult Obesity 27% 26% 25%
Adult Smoking 24% 18% 14%
Physical Inactivity 26% 23% 20%
Injury Deaths 109 69 50
Social & Economic Factors Ranked 46th
Children in Poverty 29% 25% 13%
22
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
The greatest challenge was the volume of
need in the community.
Lauren Young
Table 4: Any County Health Rankings Compared to Florida and U.S. Benchmarks
The Robert Wood Johnson Foundation (RWJF) publishes the County Health Rankings. This initiative provides information on
nearly all U.S. counties ranking them on 30 indicators. The indicators are grouped as follows:
Table 4 is an example of the some of the information available at the RWJF site (http://www.countyhealthrankings.org).
The selected indicators included in Table 4 may be particularly helpful if your MIH-CP is focused on healthy-life measures
and chronic diseases. These are two areas that align with the Florida Department of Health’s strategic initiatives.
Of the 11 MIH-CP Programs in Florida who reported operating a MIH-CP program and were respondents to a recent survey,
82% (9) stated they started their programs based on a needs assessment using internal data regarding high volume users.
Of the two remaining respondents, their parent organization selected the focal area in one organization and the other, a
funding source dictated it.
Budget Note: Add the cost of your data collection
and analysis into your budget as a Miscellaneous
expense.
1. Health Outcomes
a. Length of Life
b. Quality of Life
2. Health Factors
a. Health Behaviors
○ Tobacco Use
○ Diet & Exercise
○ Alcohol & Drug Use
○ Sexual Activity
b. Clinical Care
○ Access to Care
○ Quality of Care
c. Social and Economic Factors
○ Education
○ Employment
○ Income
○ Family & Social Support
○ Community Safety
d. Physical Environment
○ Air & Water Quality
○ Housing & Transit
C h a p t e r 0 2
Let the data drive your discovery of what is needed in your community.

23
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Chapter 2 References and Resources
1. NAEMT’s Mobile Integrated Healthcare and Community Paramedicine (MIH-CP) 2nd National Survey provides
current data on MIH-CP programs across the U.S. This includes start-up costs, target markets, services provided,
partnerships, stang, and payment. http://www.naemt.org/docs/default-source/2017-publication-docs/mih-cp-
survey-2018-04-12-2018-web-links-1.pdf?Status=Temp&sfvrsn=a741cb92_2
2. Florida Prehospital EMS Tracking and Reporting System (EMSTARS) is available at
http://www.oridaemstars.com/
3. Florida Department of Health, Agency for Health Care Administration provides quality and cost information
on health plans, hospitals and ambulatory surgery centers emergency room care, and prescription drugs. This
resource is available at http://www.oridahealthnder.gov/index.html
4. The Florida Department of Health’s CHARTS website is located at
http://www.healthcharts.com/charts/ChronicDiseases/default.aspx
5. The Florida Agency for Healthcare Administration web site FloridaHealthFinder.gov
This site assembles and displays provider/facility utilization and performance data. Types of data available
include emergency department utilization and cost at http://www.oridahealthnder.gov/index.html
6. The World Bank published a free, online guide for conducting a needs assessment. The reference and site
are as follows: A Guide to Assessing Needs: Essential Tools for Collecting Information, Making Decisions,
and Achieving Development Results. World Bank. © World Bank. https://openknowledge.worldbank.org/
handle/10986/2231 License: CC BY 3.0 IGO.
7. Zavadsky, M, and Hooten, D. 2016. Mobile Integrated Healthcare: Approach to Integration. Burlington, MA:
Jones & Bartlett Learning.
8. Pollack, A.N. (ed.) 2018. Community Health Paramedicine. Burlington, MA: Jones & Bartlett Learning.
9. Robert Wood Johnson Foundation. County Health Rankings. Provides information on how U.S. counties rank
on health measures. http://www.countyhealthrankings.org
10. Another source of health-related information is the Gallup Well-Being initiative. Available at http://news.
gallup.com/topic/COMMUNITY_WELLBEING.aspx
C h a p t e r 0 2

24
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k C h a p t e r 0 3
CHAPTER 3
Identifying Stakeholders
This Chapter introduces stakeholders and the importance of considering both internal and external stakeholders. An important
task of the program leader/administrator is to engage stakeholders early and often.
Several tools can help your thinking, organization, and engagement of stakeholders, and we will look at one of them, the Power
versus Interest Grid.
For purposes of this discussion, power and interest are
operationalized as:
1. If an individual or group has access to the resources
needed to solve a problem or resolve an issue, they have
power. Power bases include wealth, status, knowledge,
and skill.
2. An individual or a group’s interest is a function of
whether they are affected by the issue, change, or
disruption in the status quo. Interest will vary by the
degree to which the issue, change, or disruption of the
status quo affects the individual or group.
Stakeholder identication, as well as their ongoing
engagement, takes time and energy, and organizations
that commit to the engagement of stakeholders are
better able to manage program implementation and
harness the creative knowledge and communication
capacity of stakeholders.
Several scholars who study program implementation
describe stakeholders along two dimensions, both
power and interest. For a more detailed discussion of
power versus interest see the work of Crosby & Bryson
(2005), the reference is at the end of this Chapter.
Finding people that encourage your
innovative thinking and outside the
box approach is the key to program
development and success. Develop
champions to support the program – in
other words, rally the stakeholders.
James Crutchfield
Totsapon Phattaratharnwan/Shutterstock.com
Stakeholder Analysis

High Power/Low Interest High Power/High Interest
Low Power/Low Interest Low Power/High Interest
25
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Communication with stakeholders
should be continuous and consistent
Richard Ellis
Stakeholders with high
power and high interest
will likely have the most
inuence on a problem or
solution, and a program
leader must manage these
stakeholders closely. This
group may make or break
the stakeholder alliance
if their interests are not
seriously considered.
Note that groups with high
power and low interest also need
attention, and the program leader
should work to sway them into the
high power/high interest quadrant.
The effective leader will attempt
to frame the issue or solution in
such a way as to inspire interest,
harnessing stakeholder energy
to help work on the identied
problem. The program leader
who can frame the issue and
solution, create a powerful and
persuasive message, and fully
engage stakeholders is a visionary
leader. Typically, your target clients
are assigned to the low power/high
interest quadrant. Even if they have
low power, they are important,
and leaders should reach out to
them and seek their input. Clients
may become powerful program
champions if they are treated with
respect and as partners.
A power-versus-interest grid typically helps determine which stakeholders’ interests and power bases should
be considered to address the problem or issue at hand. It also helps highlight coalitions to be encouraged
or discouraged, what behavior should be fostered, and whose buy-in should be sought or who should be “co-
opted.”
Table 5 displays the power versus interest grid and is constructed by categorizing stakeholders into one of
four groups:
High Power/Low Interest
High Power/High Interest
Low Power/Low Interest
Low Power/High Interest
Table 5: Power Versus Interest Grid
George Rudy/Shutterstock.com
C h a p t e r 0 3

26
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
It is important to consider both internal and external stakeholders. For example, if you are the MIH-CP champion in your
organization and your boss thinks MIH-CP’s are a waste of time, your efforts may be in vain. In this case, your boss has high
power/low interest and can derail your efforts. Moving your boss to the high power/high interest quadrant may solve this
problem. Recognizing internal weaknesses exist is the rst step in developing strategies to turn the weaknesses into strengths.
Included in Appendix J is a document describing the Palm Beach County Fire Rescue MIH Pilot Program focused on high frequency
callers. It is an example of a concise description of a program that would be helpful to inform stakeholders including your local
radio stations and newspapers. You may even turn them into champions.
Organizing a Local Alliance
Whoever leads the program must be all
in and excited about the program.
Wendy Crews
For purposes of this discussion,
an alliance is the group of
stakeholders and other individuals
or groups that you have organized
to help you. Organizing an alliance
is an important task, and they
are an important variable in all
stages of the program design and
implementation. The relationship
between the program leader
and the stakeholders is key as
stakeholders may be powerful
foes or allies. Since trust is at
the heart of a relationship, all
communication must be open,
honest and frequent. The program
leaders must communicate
effectively, listen, seek to
understand, and put the needs of
the stakeholders above their own.
By carrying out these activities,
leaders will create an environment
of trust.
The program leader works with
stakeholders to identify problems
and solutions, as well as resources
in the community that are already
focused on the need/problem. The
stakeholders provide important
information regarding the political,
social, and cultural waters that the
leader must navigate.
Potential alliance members you
may include:
■ Primary Care Providers
■ Nursing Home Professionals
■ Hospice Professionals
■ Hospital Administrators
■ Senior Center Representatives
■ Visiting Nurses Professionals
■ Third Party Payors
■ Law Enforcement Representative
■ Fire Department Representative
■ Social Service Agency
■ Representative
■ Public Health Representative
■ Pharmacy Professional
■ Mental Health Professional
■ Federally Qualied Health
Centers
■ Local Charities Representative
■ (based on the type of service)
■ Civic / Veterans Organizations
■ Education Institutions
■ Potential vendors (e.g.,
Telemedicine)
■ Church Representative
■ Public Representative
■ Local Government
Representative
■ State Government
Representative
■ Transportation Organizations
C h a p t e r 0 3
27
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Keep in mind that all parties must see value when participating in the program. NAEMT’s Mobile Integrated
Healthcare and Community Paramedicine (MIH-CP) 2nd National Survey illustrates the quid pro quo of
referrals between stakeholders and your MIH-CP Program and the information in Table 6 came from that
report. It summarizes the quid pro quo modied to show the central position of your MIH-CP Program. Be
sure to think about how you can provide value to the stakeholders, not just what they can do for you.
One tool you can use to help craft your message is a NAEMT resource, EMS 3.0: Explaining the Value to
Payers. It provides talking points and answers to key questions asked by specic types of stakeholders. You
can nd it at http://www.naemt.org/docs/default-source/2017-publication-docs/ems-3-0-talking-points-to-
payers-2018.pdf?sfvrsn=952fcb92_2
Historically, it has been dicult getting third-party payors, such as insurance companies, to partner with
MIH-CP programs. But, that is starting to change. After piloting projects with MIH-CP programs throughout
the nation, they are now more interested in talking about and developing partnerships with MIH-CP’s to
provide services.
Be multifaceted – everyone can be used
to help a patient. Look at community
options because each is unique (Meals
on Wheels, churches, etc.). Be sure
to also consider national partners as
resources.
James Crutchfield
Table 6: MIH-CP Referrals
67% Hospitals
58% Physician groups/clinics
40% Home health
36% Social service agencies
35% Care management organizations
30% Law enforcement
24% Mental healthcare facilities
26% Other EMS agencies
25% Hospice
23% Public health agencies
19% Addiction treatment centers
17% 3rd party payers
(such as insurance companies)
10% Nursing homes
8% Urgent care facilities
51% Social service agencies
50% Home health
48% Mental healthcare facilities
43% Addiction treatment centers
39% Physician groups/clinics
39% Hospice
35% Care management organizations
28% Hospitals
25% Public health agencies
24% Urgent care facilities
10% Nursing homes
10% Law enforcement
9% Other EMS agencies
8% 3rd party payers
(such as insurance companies)
Referrals To MIH-CP Referrals From MIH-CP
MIH-CP
PROGRAM
C h a p t e r 0 3

28
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Matt Zavadsky, Chief Strategic Integration
Ocer at MedStar Mobil Healthcare,
recommends you be selective. Your focus
should be on the organization’s largest
third-party payor, not the one you bill the
most. For example, if Medicaid is billed
$600K, but only pays $200K, and XYZ
company is billed $300K and pays $250K,
they should be partnering with XYZ, not
Medicaid. Zavadsky goes on to say,
“You
want to bring those organizations to
the table to see if they are interested
in developing a new model where they
pay for all responses irrespective of
transport.”
Leaders need visionary skills to develop a shared
understanding of community problems, build
support for benecial solutions, and develop
a commitment to collective action. They need
political skills to turn a proposed solution into a
specic program. One important consideration:
The relationship between the stakeholders and the
program leader may disintegrate if the program
leader is perceived as biased towards one group
or another. The effective program leader must
nurture the stakeholder alliance by participating in
honest and open dialogue.
Also, the program leader may not be able to
give the stakeholders everything they desire,
but this must be communicated in open and
honest dialogue. Always consider that alliances
will disintegrate if the program leader fails to
communicate, communicates in a biased manner,
lacks objectivity, has preconceived solutions, has a
personal agenda, and does not listen to members.
The payors have finally awaken.
Matt Zavadsky
More communication with stakeholders
that is continuous and consistent.
Richard Ellis
What It Takes to Lead a Local Alliance
C h a p t e r 0 3

29
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Chapter 3 References and Resources
1. An older text, but a classic that presents a depth discussion of Power Versus Interest Grids and approaches
to solving perennial and thorny public problems. Crosby, B. & Bryson, J. (2005). Leadership for the Common
Good: Tackling Public Problems in a Shared-Power World, 2nd Edition. Jossey-Bass.
2. Potential alliance members may be found through your regional Healthcare Coalition. To learn more and nd
the one in your region: http://www.oridahealth.gov/%5C/programs-and-services/emergency-preparedness-
and-response/community-preparedness/healthcare-coalitions.html
3. The National Association of County & City Health Ocials provides resources for engaging public health
system partners, stakeholders, and community members. It has PowerPoint presentations, a webinar on
facilitating diverse groups, and many tools and forms for engagement. http://archived.naccho.org/topics/
infrastructure/CHAIP/partner-engagement.cfm
4. For more information on Federally Qualied Health Centers go to https://www.cms.gov/Outreach-and-
Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/fqhcfactsheet.pdf
5. Find your county’s Federally Qualied Health Center at https://ndahealthcenter.hrsa.gov/
6. NAEMT’s Mobile Integrated Healthcare and Community Paramedicine (MIH-CP) 2nd National Survey: http://
www.naemt.org/docs/default-source/2017-publication-docs/mih-cp-survey-2018-04-12-2018-web-links-1.
pdf?Status=Temp&sfvrsn=a741cb92_2
7. NAEMT EMS 3.0: Explaining the Value to Payers. http://www.naemt.org/docs/default-source/2017-
publication-docs/ems-3-0-talking-points-to-payers-2018.pdf?sfvrsn=952fcb92_2
C h a p t e r 0 3

30
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k C h a p t e r 0 4
CHAPTER 4
Developing Your Program Plan
marketing. An example might be:
“Our mission is to
improve the health of every person in our county by
bringing healthcare to their door.”
A helpful YouTube video called Ted Talk by Simon
Sinek illustrates the importance of the “why.” A link is
provided in the resources at the end of this Chapter.
Bring together a diverse group of individuals to
watch the video and work on the development of an
inspirational mission statement. Include people with
differing viewpoints and experiences in this activity
to maximize the generation of ideas and, ultimately,
their buy-in to the program. Individuals to consider
are potential stakeholders/alliance members and
customers, internal leaders, and potential employees of
the program.
Any discussion of what you may do in response to
your needs assessment that used internal, external, or
both types of data, must be based on solid and clearly
dened vision, mission, and goals.
A vision statement is the “Where are we going?”
statement. It should be an aspirational description of
what we want to achieve or accomplish. An example
is:
“To have XYX County free of all preventable illness
and injury.”
It’s a high-level picture of where we want
to be in the future.
Your mission statement is the heart of your MIH-CP.
It is the “why” you are doing it. Everything else ows
from that “why.” It guides what you do and how you
do it. It’s the basis of all your communications and
Clarify your mission, vision, and purpose
for the program. Establish what you want
to accomplish.
Orlando Dominguez, Jr.
What will you do: Mission Matters
Manatee County Florida Community Paramedicine

Goals
Establish strategic partners to support the provision of bringing
healthcare to their door.
Improve the health of residents with diabetes.
Strategies
Create a strategic partner development plan with supporting
materials.
Develop an in-home chronic disease management system for
diabetes.
Objectives
Within the rst 6 months, establish agreements with at least 4
strategic partners to either provide the services “to their door”
or funding to support a Community Paramedic to deliver the
services.
Within the rst 6 months, test the in-home chronic disease
management system with 20 diabetic residents and perform a
baseline health analysis.
31
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
If you’re in it just for the dollars, don’t
do it. Do it for the right reasons: your
mission. Mission matters.
Richard Ellis
Once, you have your inspirational program vision and
mission compare it to your organization’s mission
statement, vision, and goals. Are you in alignment with the
organization? If you are, this gives you leverage in seeking
support and funding because you can emphasize that your
program will help the organization achieve its mission,
vision, and goals. However, if it is not in alignment, the
opposite is true. You may have a challenge “selling” it to the
leaders of your organization. If that is the case, see if you
can revise your program mission to be in alignment with
your organization’s mission.
Program Goals
Strategies and Objectives
Your program goals should dene how you want to achieve your mission. After articulating your goals operationalize
them by specifying strategies and objectives. Using the example mission from above, how do you improve the health of
every person in your county by bringing healthcare to their door? There can be multiple goals focused on different ways
of meeting the mission. Possible goals for this mission statement might be:
■ Establish strategic partners to support the provision of bringing healthcare to their door.
■ Improve the health of residents with diabetes.
These are just 2 examples – you need to have that direction of how your program is going to achieve its mission in your
goals.
Your strategies are more dened actions you are going to take to achieve the goal and your objectives are very tactical
and measurable. Table 7 provides an example goals, strategies, and objectives.
Table 7: Goals, Strategies, and Objectives
C h a p t e r 0 4

32
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Developing Your Implementation Plan
Finally, verify that your program goals, strategies, and objectives are not in conict with others in your community. You want to
build on other’s work in the community or complement the services they are currently providing. A MIH-CP should not duplicate
or compete with the currently available resources. If you have a conict, see if you can work together to accomplish common
goals, strategies, and objectives or consider addressing another gap in healthcare or unaddressed need in your community.
Working together and not in silos creates higher success rates for everyone involved.
You’ve identied the need or problem to work
on, stakeholders to engage in your alliance, and
developed your vision, mission, goals and objectives.
This is where you describe your intervention – the
what. Again, what are we going to do to accomplish
the program goals? Strongly consider, an evidence-
based practice that has been shown to eliminate
the problem you identied, stop it in its tracks, or
minimize its consequences.
Your program implementation plan includes a
description of:
■ How the proposed MIH-CP services are appropriate
to meet the identied needs.
■ Who are the leaders, managers, and other staff
executing the program?
■ What does the organizational chart look like and
who reports to whom?
■ Will there be a single person doing everything or are
other staff required?
■ How the program integrates with other community
services, providers, other levels of care, and
referrals.
■ The evidence-based practice, best practice, or
data-driven innovation that will be part of the
program. For example, if you are conducting a
fall reduction program the U. S. Department of
Health and Human Services, Centers for Disease
Control and Prevention’s Preventing Falls: A Guide
to Implementing Effective Community-Based Fall
Prevention Programs is an example of an evidence-
based practice you could use.
■ A description of the organization’s standard
operating procedures (SOP) that are on-hand or will
be developed.
When you prepare your implementation plan,
include appropriate and reasonable time-framed
tasks (i.e., infrastructure planning, staff recruitment
and retention, facility development/operational
planning, information system acquisition), as well as
individuals charged with their completion.
Consider evidence-based interventions.
If none exist, consider data-driven
innovation.
Lauren Young
City of Gainesville Florida Community Paramedicine
C h a p t e r 0 4

28%
Single
encounter
only
30 days or less
31 to 90 days
91 to 180
days
More than
180 days
9%
10% 10%
43%
33
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Define a specific program and build
processes around it, because the
process allows you to expand to
other types of problems once you
have them in place.
Don Hughes
Regarding policies and procedures, every program should
have clear statements of their policies and procedures that
lead to the articulation of standard operating procedures
(SOPs). It is important to actively involve the medical
director in their development since the Community
Paramedic’s scope of work is based on medical direction.
Policies and Procedures
Specic SOPs to include as part of your program are the
following:
■ General Physical Assessments
■ Home Safety Assessments
■ Medication Reviews and Reconciliations
■ Emergency Situations
■ Patient Consents in compliance with the Health Insurance
Portability and Accountability Act (HIPAA)
■ MIH-CP Entry into Care and Discharge
■ Quality Assurance
Other questions to ask and for which you may need SOPs are: How do clients and referring providers or organizations
reach you? Will clients call a dedicated line or the main number? What are the advantages and disadvantages of using
Email? If you need to develop SOPs, the NAEMT MIH-CP Toolkit provides sample SOPs and forms that may be used to
develop your own program’s SOPs. Be sure to customize the SOPs to match the design of your program and the services
you provide.
Table 8 is from the 2nd National Survey on Mobile Integrated Healthcare and Community Paramedicine. It illustrates
the length of time patients are enrolled in the 129 organizations that responded to the NAEMT survey. It is helpful to
get a “ballpark” idea of what you might expect. This information may be useful as you plan your program and develop
a SOP for how clients enter your MIH-CP Program.
Appendix H is a sample MIH Provider Referral Entry into Care Form and Appendix I is a sample MIH Provider Initial
Contact Form. Use the forms to develop your customized enrollment SOP.
Table 8: Length of Enrollment
How long are patients enrolled in the MIH-CP Program?
C h a p t e r 0 4

34
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Identifying the resources within
the community, and establishing
the reliability, availability, supplies
and qualifications was the greatest
challenge to starting a MIH-CP
program.
Orlando Dominguez, Jr.
Finding an employee who wanted to
do it was the challenge. Getting the
data was easy and talking to people
is easy.
John McNamara
Resource Guide
Selecting a Leader
Brevard County Florida Community Paramedicine
C h a p t e r 0 4
As you’ve been developing the mission of your MIH-CP,
there must be a person with the vision of what it will
look like, the passion for getting over challenges, and
the desire to make it run well. This is who you want to
lead the program! You need to select someone who
doesn’t have an “I’m doing it because I was told to”
attitude. Find the real champion to lead your program
– and it may not be the one with the most experience or
the most senior person!
Several of the MIH-CPs in Florida interviewed are
operated by re departments, and one of the issues
they have encountered is the department seniority
system. The system may limit the selection of the MIH-
CP leaders, and, at times, prevents them from placing
the real champion in the leadership position. This
may be a challenge you need to address early in your
program development.
As discussed earlier, leadership skills are not the same
as emergent or acute care skills needed to work directly
with a patient. Look for leadership skills and traits,
such as excellent listening/communication, a heart
for service, empowers others, patience, commitment/
dedication, humility, respectfulness, foresight/visioning,
honesty/integrity, innovative, inspirational/passionate,
and transparent/authentic.
Budget Note: Insert the annual cost of your leader’s
salary and benets under payroll expenses – Salaries
of Leader and Staff. Keep in mind that the actual cost
is not just the salary of the person, but the employer
required matching taxes, unemployment insurance,
workers compensation, retirement benets, and insur-
ance.
Developing a compendium of resources is so important.
While it is everyone responsibility to identify community
resources, it is strongly recommended that someone
is assigned to update and continuously maintain a
Community Resource Guide for the program. Most
county social service agencies already have and use a
community resource guide. However, you may want to
remove or add resources which are specically focused
on your program services. Resources may include
medical equipment/supplies, prescription assistance,
and the name and location of food pantries. Creating a
guide for your agency’s program is an essential duty to
ensure overall program success.

35
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Take time to find ‘good’ staff – they
will make or break your program.
Ariella Bak
Stang
Staff Skills
C h a p t e r 0 4
Things you need to consider are:
■ Does the MIH-CP program t into your current organizational chart? To whom does the leader of the MIH-CP program report?
Or, do you need a separate organization chart for your MIH-CP program?
■ Do you need MIH-CP coverage 24/7, part-time or full-time staff?
■ Will you operate every day or only during the week or weekends?
■ With the shortages in the EMS industry, does it have to be a paramedic? Can it be another medical provider or a partner? Can
it be a non-medical person?
■ How many people do you need to operate it, such as eld personnel, partnership/alliance management, billing, reporting, data
analysis, and administration?
Based on your responses to these questions, the next steps are developing your organizational chart, stang plan, and job
descriptions. For your organizational chart, you can either build on and modify your current organizational chart or use
the template in Appendix D to develop a new one.
Your stang plan is a key component of your business plan that describes the number and types of people to involve,
what they will be doing, and when they will be doing it. After your stang plan is complete, develop job descriptions
for each staff person, including the leader. In the job description, dene the education and experience qualications,
responsibilities, and desired skills. Include any additional expectations of the position, such as continuing education
requirements.
Recently, a MIH-CP online student described the work of Community Paramedics as being focused on closing the gap
between emergency room care and care in less costly settings. So, how are the skills of an emergency care Paramedic
different than the skills of a Community Paramedic? This was a question asked in the interviews with the 11 MIH-CP
organizations in Florida. Here are paraphrases of what they said:
Once you have your leader, you will need to develop
an organizational chart, job descriptions, and a stang
plan. Many MIH-CPs begin their program by placing a
light duty paramedic in a community paramedic role.
■ We hire both pre-hospital Paramedics and Community
Paramedics based on the same criteria. All medics require
critical thinking and problem-solving skills, but we also look
for compassionate Community Paramedics.
■ Looking for expanded history taking and physical
examination skills so that the Community Paramedic can
see broader health concerns.
■ A willingness to take on unplanned service calls.
■ A willingness to expand the scope of practice and do things
outside of EMS critical care.
■ Additional pharmacy and lab training is a plus.
■ Soft skills, communication, and all skills considered part of
an individual’s emotional intelligence.
■ An ability to get things done.
■ Experience navigating the healthcare system.
■ Advocacy skills.
Skills you should look for when hiring Community Paramedics for your MIH-CP are good problem solving, strong advocacy,
excellent listening/communication, observant, a heart for service, patience, versatile technical abilities, compassion,
commitment/dedication, respectfulness, honesty/integrity, innovative, passionate, and authentic.

36
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
The skills in the CP program require more
detective work and root cause analysis
capabilities.
John McNamara
Keep in mind that not all the MIH-
CP skills are taught in paramedic
training programs, and employees
in the MIH-CP program may
not know what is required or
understand the MIH-CP paradigm.
The MIH-CP is a paradigm shift
from the traditional pre-hospital
paramedic practice. It is a shift in
practice and the thought process.
The skills previously described
are consistent with the
recommendations of Dan Swayze.
In his 2015 article published
in JEMS, he identies the core
competencies for community
paramedics as the following:
1. Expanded Patient Assessment
2. Therapeutic Communications
3. Understanding Mental Health
4. Patient Navigation & Advocacy
Swayze goes on to highlight the
concept of localization. That is to
say; programs are unique to their
social, cultural, and geographical
context. Consider your
community’s social, cultural, and
geographical context as you design
your program and recruit and train
staff.
NAEMT’s Mobile Integrated
Healthcare and Community
Paramedicine (MIH-CP) 2nd
National Survey asked the 129
MIH-CP programs about personnel
requirements. Field EMS experience
was by far the most common
response at 88%.
College-based community college
paramedic education was 27%.
Some required more specialized
training, 27% required behavioral
health crisis intervention training,
21% required critical care training,
and 7% required community health
work certication.
A template Performance-Based
Community Paramedic Job
Description is included in Appendix G.
Budget Note: Add the salary cost
of your staff and the salary of your
leader under payroll expenses –
Salaries of Leader and Staff. And, be
sure to once again add the addition-
al costs of benets for the staff to the
leader benets.
Budget Note: If you plan to staff us-
ing overtime, include the salary and
benets of the staff under the over-
time row as overtime is at a higher
rate of pay than standard pay.
Manatee County Florida Community Paramedicine
C h a p t e r 0 4

37
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Training / Skill Development
Levels of Community Paramedic Training
C h a p t e r 0 4
Often initial and ongoing training expenses are overlooked. In the section above, you’ve identied the job responsibilities
and skill sets necessary for your program. How will you either obtain those skills, enhance them, or maintain them for a
successful program?
What type of initial training is necessary to launch your program? Will you send the person to training outside of your
organization? If so, you need to consider not only the tuition and fees, but the associated travel expenses, such as
transportation, hotel, and meals. If you are conducting in-house training or doing training on-line, be sure to include any
associated expenses as well.
You may also want to plan for enhancing the skills sets of the staff. Evaluate what skills will expand or elevate your
program to greater success. Will a special certicate or degree be of value to the individual and your MIH-CP program?
There are various levels of training for Community
Paramedics. Here are some examples:
Bachelor of Science – Community Paramedicine Specialization
Seminole State College of Florida offers a medical specialty
degree in Community Paramedicine. The candidate must
have an Associate’s degree with a 2.0 GPA or higher,
completed a Florida Department of EMS approved
paramedic program or be eligible for certication as a
Florida paramedic, or be a certied Florida paramedic. The
program covers legal and ethical aspects, communications,
research, economics, systems, management, general
education courses (i.e., math, science, history); and specic
CP programs in delivery and practice of community
paramedicine. Total hours is 120.
Associate in Science Degree Program:
Northern Maine Community College, Presque Isle, ME
offers an Associate degree in Community Paramedicine.
Required courses are Health & Safety Compliance;
Community Paramedicine; English Composition; CP
Skills Lab; CP Clinical; Leadership in EMS; Community
Paramedicine Seminar; College Algebra; Anatomy
& Physiology I & II; Introduction to Nutrition; a
Communications elective; General electives; General
Psychology; Sociology; and Humanities. A total of 60 hours
of education.
Advanced Certicate Program:
Northern Maine also offers an Advanced Certicate
program, for those already possessing an Associate degree
or higher. The courses are the same as those for the
certicate program described below, excluding the English
and Math courses. Total hours is 16.
Certicate Programs:
Hennepin Technical College, Eden Prairie, MN offers an
advanced Technical Certicate as a Community Paramedic.
It requires a current license as an EMT-P and at least two
years of experience as a paramedic. The curriculum is 14
hours, covering the topics of Role Advocacy and Outreach;
Community Assessment; Care and Prevention Development
Strategies; and Community Paramedicine Clinicals.
Northern Maine also offers a certicate requiring 22
hours of education. It covers Health & Safety Compliance;
Community Paramedicine; English Composition; CP
Skills Lab; CP Clinical; Leadership in EMS; Community
Paramedicine Seminar; and College Algebra.
Certicate Programs – Online:
Nature Coast EMS offers an online Community Paramedic
certicate program focused on two things: skill
development and program design and implementation.
Recognizing that technical and soft skill sets are different

38
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Human Resources Policy and Procedure Manual
C h a p t e r 0 4
One nal consideration involving stang, verify your organizational chart, stang plan, and job descriptions are consistent
with your organization’s current Human Resources Policy and Procedures Manual. You may need to modify the Manual or
your documents to be sure you are in alignment with the organization.
If you need to develop one for your MIH-CP, there are many online resources. One resource is the sample Community
Development Corporation Policies and Procedures Manual developed by Local Initiatives Support Corporation to assist
community development corporations. You can nd the link to it in the references and resources at the end of this
Chapter.
for acute care, emergent care, and leadership, the
program addresses those skills necessary for a community
paramedic. It also guides you through the development of
a customized business plan for a MIH-CP Program.
Northern Maine is currently testing an on-line version of
their Community Paramedicine curriculums with the clinical
portion being completed locally. At this time, it is not
available, but likely will be offered in the near term.
When evaluating a training program, be sure to look for
one specic to the community paramedic role. Many
training programs are using the term “paramedicine” and
“paramedic” interchangeably. For instance, Metropolitan
Community College, Omaha, NE offers a certicate of
achievement in Paramedicine. However, when you read the
curriculum, you see it is preparing students to become a
paramedic and sit for the National Registry exam. It is not
focused on the specic community paramedicine skills.
Certication:
The International Board of Specialty Certication offers
a CP-C certication exam. It is not an educational
program, but a test designed to validate the competency
of paramedics providing services beyond the roles of
traditional emergency care and transportation.
Budget Note: Keep in mind that higher education levels
will usually impact the salary or wages, so consider this
when evaluating the salary in your budget.
NAEMT’s Mobile Integrated Healthcare and Community
Paramedicine (MIH-CP) 2nd National Survey asked the 129
MIH-CP programs about personnel training. And, nearly all
of them stated they required additional specialized training
as follows:
■ 87% Clinical training, such as medication administration
and chronic disease management
■ 73% Accessing community and social services resources
■ 69% Patient navigation
■ 69% Patient relationships/communications (ex:
motivational interviewing)
■ 58% Enhanced patient assessment
If your organization pays for continuing education credits
for your paramedics, be sure to include the expense in your
budget.
Budget Notes: If applicable, under Miscellaneous Expens-
es, include the cost of initial training and continuing edu-
cation training expenses in the budget in their respective
section. Put the meals and travel costs associated with
the training in their respective sections.
Budget Notes: Under Administration, include the cost of
the licensing fees.

39
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Logistics and Overhead Expenses
Multidisciplinary Advisory Committees
Identifying your stakeholders and partners for
launching a program is important in the early
stages of program design and the rst step in
beginning a relationship. These individuals may
be working in conjunction with you to provide
client services in the community. But that is not
the end. You should also seek to leverage their
talent, experience, and knowledge for continuous
improvement, quality control, growth, and
directional vision as part of a multidisciplinary
advisory committee. They will be your
community champions.
An advisory committee does just that – advises. It is
not a board of directors and should have no operational
authority or authority to mandate program changes.
However, the power the committee does have is the power
of “feet.” That is if they recommend changes, and, if those
changes do not happen, they can walk away as stakeholders
in your program. This can have a signicant impact on
your program – either for the good or the bad. That’s why
it is important to carefully establish the parameters of the
committee. You can call them By-Laws or Guidelines, but
essentially you are dening what you want the committee
to help you with and how to do it.
Have as many hands involved in the
program as possible. It is tough to
do it alone. Continually develop your
knowledge base. Match knowledge
skills with diverse multidisciplinary
skills of others.
John McNamara
Matej Kastelic/Shutterstock.com
C h a p t e r 0 4
There are many issues you need to think about to make
your program work. Here are some things to think about:
■ How are you getting your personnel to the clients? Or, are
they coming to you through a partnership arrangement of
some kind?
■ Will your staff wear uniforms?
■ What capital equipment and supplies are needed for
the staff person to do their job? Computers? Software?
Medical equipment?
■ What supplies/equipment, if any, are you giving to the
client? Blood pressure machines? Diabetic monitoring
systems?
■ What kind of space do you need? Home-based or oce-
based?
■ What are your space costs?
■ What communication system is needed? How are clients
contacting you? Are you using the non-emergency dispatch
system?
■ Other administrative overhead, such as oce materials,
supplies, internet, phones, utilities.
■ What changes are required in your insurance coverage?
■ Will there be legal fees to get started?
■ Marketing costs. Be sure to include such things as the cost
of materials, publications, copy costs, and logos on your
vehicles.
Budget Note: As you identify the necessary logistics
and overhead expenses enter them into the respective
budget lines.

40
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Reaching Your Target Market
An important question to consider is: How will you reach
the target market for your program; the populations most
likely to benet from your program? Regardless of the
way you set up your MIH-CP, you need to consider how to
attract clients. What gives your program client value? You
need to develop a Marketing Plan.
Your rst marketing consideration is to dene who you are
serving. Who is the target market for your service and what
are their demographics? You should have already done
this as part of your needs analysis, so transferring it to a
marketing plan should be fairly simple.
The next questions to ask relate to getting your program
message to those clients. How do you reach these clients?
Do you need to solicit the clients directly? Or, do you need
them to be referred to you by others, such as primary care
physicians, hospital discharge nurses, or your
own EMS staff? If you need referrals, then your
marketing efforts will not be directed to the client,
but to the people who do the referrals. This is an
important distinction as the marketing message is
different for each because their concerns, values,
and desired outcomes are different.
Pay to have professional marketing
materials developed. Don’t do it on
your own. It helps to open doors.
Wendy Crews
C h a p t e r 0 4
The items to consider when designing you Multidisciplinary
Advisory Committee are the following:
■ Mission of the Committee (verify it is consistent with the
program mission)
■ Goals of the Committee (verify they are consistent with the
program goals)
■ Number and selection process of committee advisors
■ Specic disciplines/professions?
■ Required qualications
■ Removal of an advisor
■ Selection of Chair / Co-chairs
■ Meeting frequency (should be on a set schedule)
■ Calling special meetings
■ Meeting notice requirements, if any
■ Quorum requirements, if any
■ What can come before the committee
■ Conict of Interest
■ Condentiality
The mission of the committee should describe the role
they play in your organization. Generally, they are used
to provide guidance on issues of quality, service offerings,
innovation, and growth. Be sure it is consistent with your
program’s mission.
Establish goals for the committee. What do you want them
to achieve – again, be sure they dovetail into your program
goals.
Identify the make-up of the committee. Establish the
number of advisors. It is often helpful to specically
identify “seats” by profession to maintain a specic mix
of advisors. Strive for diversity in medical disciplines
and practices, selections from various community-based
organizations, and if feasible, a public voice of the client.
Describe the qualications, if any. Who will select the
advisors? How do you remove an advisor?
Finally, create a structure for the meetings. Who is the
chair/co-chairs? How often will the committee meet?
If government based, is public notice required of the
meetings, and if so, what are the requirements for calling
and holding a meeting? Can there be special meetings
called? How? What items can come before the committee
meeting? Even though it’s advisory, do you want to require
a quorum? These functional issues need to be addressed so
everyone knows from the start what is expected of them,
how their advice will be used, and how information will be
discussed and shared.
Budget Note: If you anticipate expenses for the committee,
place those under “Other” in the Miscellaneous section.

41
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Once you’ve identied who you need to target your marketing
efforts to, then consider what the message will be for that
group. If you are marketing directly to the client, you need to
consider why these clients should use your service? What is
it about your service that makes it unique to any other in the
market? What value do you bring to them? Develop a solid
value proposition or reason a client should use your service.
For example, Our MIH-CP program brings healthcare to your
door. It eliminates the concerns of driving or needing to call
an ambulance when you need transportation for medical
care. If driving is a concern for an elderly person then they
see value in your service.
But, if you’ve targeted primary care physicians for the
marketing message to get the clients you want to serve, the
message will be different. You still need to ask: What is it
about your service that makes it unique to any other in the
market? What value do you bring to them? Your message
may be: Our MIH-CP program extends your compassionate,
competent care through our professional healthcare
providers to your special need patients (insert the needs
you’re targeting). This message speaks to a physician about
how to address patients with specic needs in a professional
manner that he or she is otherwise unable to provide. There
is value to them.
Now that you’ve identied the group to target for your
message, the next issue is how you are going to reach them?
What marketing materials do you need? What kind of print or
social media will work, if any? Do you need to do face to face
or oce visits? Do you need yers, brochures, business cards,
etc.? How can your stakeholders help you get the message
to the target group? As you develop this strategy, be sure to
include the cost of the marketing materials in your budget.
In Appendix E there are two simple one-page marketing
plan templates by Ivana Taylor from Small Business Trends.
Using the link in Appendix, you can access the marketing plan
templates and actually write your plan into the template.
She also provides mocked up sample plans you can use as a
guide.
Finally, an important consideration in marketing is how you
want to be branded in the community. In interviews with
the Florida MIH-CP programs brand visibility is sometimes an
issue. Some programs use unmarked vehicles because their
clients don’t want their neighbors to become alarmed if they
see an EMS logo on the vehicle parked outside their house.
Alternatively, other programs use their EMS logo vehicles. In
those communities seeing an EMS vehicle is not alarming, and
people are reassured that a trusted and respected provider
is caring for their neighbor. It is something you need to be
sensitive to as you develop your program to meet the needs
of the community you serve and the preferences of the client.
Budget Note: Once you have developed your marketing plan,
assign costs associated with the implementation of the plan,
such as printing, vehicle logos, marketing development and
maintenance contracts, and social media development. En-
ter the cost into the line for marketing/public relations.
Get out there – make contacts, shake
hands, tell your story, and provide
information.
Christine Long
City of Gainesville Florida Community Paramedicine
C h a p t e r 0 4

42
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Chapter 4 References and Resources
1. Ted Talk by Simon Sinek on developing your mission – your “Why” to inspire action: https://www.ted.com/
talks/simon_sinek_how_great_leaders_inspire_action
2. The NAEMT MIH-CP Toolkit provides sample SOPs and forms that are available at http://www.naemt.org/
initiatives/mih-cp/mih-cp-program-toolkit
3. Centers for Disease Prevention and Control’s fall prevention resource Preventing Falls: A Guide to
Implementing Effective Community-Based Fall Prevention Programs is available at
https://www.cdc.gov/homeandrecreationalsafety/falls/community_preventfalls.html
4. Sample Community Development Corporations Policies and Procedures Manual: https://community-wealth.
org/sites/clone.community-wealth.org/les/downloads/tool-lisc-procedure-manual.pdf
5. Another guide on writing a Policies and Procedure Manual is from Professor Michael Grin, How to Write a
Policy Manual. It is not a sample, but instead provides guidance and tips on the development of the manual.
http://templatezone.com/download-free-ebook/oce-policy-manual-reference-guide.pdf
6. NAEMT’s Mobile Integrated Healthcare and Community Paramedicine (MIH-CP) 2nd National Survey: http://
www.naemt.org/docs/default-source/2017-publication-docs/mih-cp-survey-2018-04-12-2018-web-links-1.
pdf?Status=Temp&sfvrsn=a741cb92_2
7. Another example job description is found in the NAEMT MIH-CP Program Toolkit at http://www.naemt.org/
initiatives/mih-cp/mih-cp-program-toolkit
8. MIH-CP Knowledge Center has many resources you can utilize in the development of your plan. There are
articles, research, case studies, legislation information, tools, policies, and survey information. http://www.
naemt.org/initiatives/mih-cp/mih-cp-knowledge-center
9. The National Highway Trac Safety Administration, Oce of EMS has resources on education, workforce,
research, data, preparedness, and advancing EMS systems.
https://www.ems.gov/index.html
10. South Carolina Oce of Rural Health, Blueprint for Community Paramedicine Programs, Especially for EMS
Agencies, Version 1: The Abbeville Experience is an overview and resource to see how others have developed
CP programs. https://nosorh.org/wp-content/uploads/2014/08/SC-Community-Paramedicine-Blueprint_V1-
Melinda-Merrill-and-Michele-Staneck.pdf
C h a p t e r 0 4

43
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Chapter 4 References and Resources
11. Community Paramedicine specic programs:
■ Hennepin Technical College Community Paramedic Certication program: https://www.hennepintech.edu/
program/awards/394
■ Northern Main Community College Community Paramedicine programs: http://www.nmcc.edu/wp-content/
uploads/CP-1718.pdf
■ St. Cloud Technical & Community College: https://sctcc.edu/degrees-programs/community-paramedic/community-
paramedic-certicate-13-credits T
■ Seminole State College of Florida: https://www.seminolestate.edu/catalog/program/HS-BS/paramedic2
■ Nature Coast EMS: https://www.naturecoastems.org/education.php
12. Metropolitan Community College Paramedicine programs – which are actually Paramedic training programs:
http://mccneb.smartcatalogiq.com/en/2016-2017/Course-Catalog/Programs-of-Study/Health-and-Public-
Services/Health/Paramedicine-PMPMC
13. Florida Administrative Code 64J-1.009 governing certication of Paramedics: https://www.rules.org/
gateway/RuleNo.asp?title=Emergency%20Medical%20Services&ID=64J-1.009
14. A couple of templates for a one-page marketing plan by Ivana Taylor from Small Business Trends can be
found in the Appendix You can nd links to others on the website: https://smallbiztrends.com/2008/06/one-
page-marketing-plan.html
15. Chronic Disease Management for the Community Paramedic at
https://www.emsworld.com/article/12240314/chronic-disease-management-for-the-community-paramedic
16. The Minnesota Department of Health offers an EMS toolkit with resources that help to address common
issues faced by rural EMS organizations:
■ The Recruitment and Retention section covers writing volunteer position descriptions, nding daytime volunteers,
and retaining members: http://www.health.state.mn.us/divs/orhpc/resources/ems/recruit.html
■ The Leadership and Management section provides links to podcasts and other resources: http://www.health.state.
mn.us/divs/orhpc/resources/ems/leader.html
17. International Board of Specialty Certication for Community Paramedics: https://www.ibscertications.org/
roles/community-paramedic
18. You may nd this link to the State Board of Education for Oregon’s resource called Developing a Local
Advisory Committee Resource Handbook helpful: http://www.oregon.gov/ode/learning-options/CTE/resources/
Documents/Developing%20a%20Local%20Advisory%20Committee%20Resource%20Handbook.pdf
C h a p t e r 0 4

44
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k C h a p t e r 0 5
CHAPTER 5
Developing Your Program Budget
Payroll, Operations, and Capital Expenses. There are
many subcategories under each section. You may not
have ALL of these expenses. They are there to simply
help you think through what is needed in your program.
You may have others to add as well.
Work through each expense category of the budget.
Initially, the numbers will be a “guess” – yes, a guess.
The gures you use are estimates based on the most
current knowledge you have at the time. The numbers
WILL change as you learn more and rene your
program. It is important to always re-evaluate your
budget gures when you make a change in any other
part of your plan.
First, the easier element, the expenses. Here are
some basic, brief denitions by Investopedia to help
you understand the budget. Expenses can be broken
down into recurring and nonrecurring. Recurring are
those expenses that are ones a company expects to
have on an ongoing basis as an ordinary cost of doing
business. Examples are fuel, equipment maintenance,
salaries, leases, utilities, and supplies. Nonrecurring
(or Capital expenses) are one-time or extraordinary
expenses. Examples are vehicles, non-disposable
equipment, buildings, and renovations to facilities.
In the Budget Template (Appendix B) you’ll nd
Expenses in yellow. The template is divided into
Expenses
Brevard County Florida Community Paramedicine
Putting numbers to a new MIH-CP is a challenge for most people. So, as you’ve been working through the development of
your MIH-CP plan you’ve also been building a foundation for your rst-year budget. Now, let’s concentrate on how to fully
develop your MIH-CP budget. We have provided a Budget Template in Appendix B to assist you.

45
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Revenue
Jirapong Manustrong/Shutterstock.com
For the Payroll section, as mentioned earlier, the actual expense is not just the salary or wage, but the matching taxes,
unemployment insurance, workers compensation, retirement and health benets paid by the organization. Talk to your
human resources person to determine a percentage of salary to use for these “extras” instead of breaking them down into
individual categories on the budget. For instance, if a person’s salary is $50,000, and the percentage for the “extras” is 30%,
then you would enter $50,000 on the salaries line and $15,000 on the Benets line.
If you anticipate overtime expenses, you’ll need to do the same – overtime wages + 30% for benets.
According to the Mobile Integrated Healthcare and Community Paramedicine 2nd National Survey, only 44% of the
national MIH-CP programs are reporting revenue generated by their programs. And, this is up from only 36% in 2014.
Also, 36% continue to receive grants, and 30% say they receive no payments. Of the 49 programs generating program
revenue, almost half of them made less than $50,000, only 24% made over $100,000. Revenue generation continues to be
a real issue for most MIH-CP programs.
This revenue issue poses the greatest challenge in developing the budget for most start-up programs. If you are fortunate
enough to be able to internally fund your program, then simply enter the amount of your total expenses into the “internal
sourced funds” budget line, and you have a balanced budget. Easy. For most, you’ll need to determine where your
revenue is coming from, and how much it will be.
C h a p t e r 0 5

46
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Grants
■ Identify exactly what you need the funding for - Equipment,
Training, Personnel, Operations, etc.
□ Your plan and budget will help you to identify what you
need to fund and how much you need.
□ Make sure your boss approves the plan and budget
for your grant proposal and that any partners already
involved in the project are on board with it. It is a waste
of your time to write a proposal if your boss or partners
are not on board with your plan.
■ Research grant opportunities which closely match your needs
□ It is a waste of your time to write a grant that is not in
alignment with your needs.
□ See the references and resource section at the end of
this Chapter for possible research sites.
■ Once a grant opportunity is identied, research as much
information as possible about it
□ What is the funding cycle?
○ Does it meet your project timeframe?
○ Do you have time to complete a strong proposal?
□ What are the eligibility requirements?
○ Is it only government/non-prots/for-prots?
○ Is only for rural or urban communities?
○ Is it only for serving specic demographics?
○ Can you partner with an eligible applicant to meet
the requirements?
□ What are the geographic limitations?
○ Is it limited to a certain state, county, town?
□ Are specic partnerships required?
○ Is it feasible to develop the necessary partnerships
in the required time frame?
□ Is the funding level appropriate?
○ It is a waste of your time to seek a very small grant
if it does not get you to the amount you need to
have a successful program. This is not to say that
you can’t use several smaller grants to fund a larger
ticket item or the overall project but be sure in the
end that you will have enough funding to complete
the project if you are awarded the grant.
○ Are matching funds required? Do we have, or can
get, those funds?
□ Who has received funding in the past?
○ Most funders will provide a list of past recipients.
This will give you a good indication of whether your
organization ts their funding prole.
□ What has been funded in the past?
○ Reviewing what has been funded will tell you a
couple of things – either they focus exclusively on
certain things – and you must be focused on the
same thing. OR because they have been funding
certain things for a long period, they are actually
looking for something that goes beyond their focus.
Be sure to ask yourself whether the current grant
details support their continued focus or whether
they are expanding beyond what they have funded
in the past.
□ Who will be reviewing the grant proposals?
○ Some grants will provide you information on who
will be handling the proposal review. If that is the
case, it is very helpful to understand their style
and focus: academic, data geeks, statistics, stories,
impact, etc.
■ Start getting the required support from any inuential partners,
government, or others which can help your grant application.
■ Read EVERYTHING several times – the details on the grant are
VERY important
□ Many, many grant proposals never make it to the
reviewer because of late submission, errors in required
formatting, failure to provide all information requested,
etc. Understanding and meeting every detailed
requirement in the grant is the only way to make it to the
reviewers.
■ Based on your research, revisit your plan to see where
adjustments can be made to more closely t the grant
requirements.
○ Don’t compromise the integrity of your program just
to get funding. Stay true to your mission.
○ If you do want to make changes to your plan, be
sure to engage your boss and your partners in the
conversation.
■ Call any contacts listed in the grant to help you clarify their
requirements.
■ Attend any conference calls or webinars hosted by the granting
organization.
□ This is where they will clarify what they are looking for in
projects and will usually respond to questions from the
audience.
■ Develop strong data to support your grant proposal.
□ Use data which supports THEIR priorities, not just yours.
□ Find comparison data to put your data into perspective.
To say the percentage of calls for falls in your community
is 30% doesn’t provide a context for the number. If you
use comparative data, such as the percentage of calls for
falls in the state is 20%, then the reader understands the
context and relevancy of the number.
■ Prepare a le to maintain your application documentation.
So, the big question on everyone’s mind: Where is the
money?
Before you seek any type of outside funding, especially grants, you must be prepared. Here is a list of specic questions
and things you need to do BEFORE you begin writing a grant for your program:
Here are some ideas for funding your program:
C h a p t e r 0 5

47
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Using grants are like the chickens in a breakfast –
they contributed (eggs), where funding the program
internally is a commitment, like the pig in a breakfast
(bacon). Commitment is a long-term focus.
Don Hughes
FUNDING SOURCES
Screenshot 2
Government Grants
When MIH-CP was a new concept in the industry, the
opportunities for grant funding was more abundant.
Monies were invested in pilot programs at the federal, state,
and local levels to learn more about the optimal design of
a program, the possible impacts a community paramedic
could have to improve the health of a community, and
alternative methods on how healthcare could be delivered.
As those years of research have now shown that MIH-CP
can have positive impacts on health and the delivery of
healthcare, fewer grants are available for pilot or new
programs, especially at the federal and state levels.
However, that does not mean federal grants don’t come
up on occasion. Most will be focused on testing a specic
concept within a community paramedicine program or a
health issue that a community paramedic could potentially
address. It’s less likely you’ll nd federal funding for a
start-up program unless your program has unique features
which address a specialized federal initiative.
You can go directly to a federal agency to search for
funding, such as FEMA’s Assistance to Fireghters Grant
Program at https://www.fema.gov/welcome-assistance-
reghters-grant-program, or the US. Department of
Homeland Security for active shooter and provider
protection equipment at https://search.dhs.gov/
search?query=grants+&op=Search&aliate=dhs.
You can also check for federal grants at the website, www.
Grants.gov. The opportunities listed change daily, regularly
checking it may help you stay on top of any quick due dates.
By putting in key search words, like “Paramedics” shown
in Screenshot 2, the current grant opportunities with that
word in them will appear. You can click on the Opportunity
number for greater details.
C h a p t e r 0 5

48
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Don’t rely on one funding source. Develop a diversified
funding model so that you can expand your programs
to meet the needs of your patient population.
Melissa McNally
Foundations
Foundations, endowments, and organizations with a philanthropic branch are another source of grant funding, or in some
cases in-kind donations. However, each will be focused on very specic areas of interest to them. To help you nd these
opportunities, The Grantsmanship Center is one online site which may be benecial. While not all their information can be
accessed without a paid subscription, there is some free information. For example, this link will take you to the Top Giving
Foundations in Florida: https://www.tgci.com/funding-sources/FL/top. By clicking on the name of a foundation in the list,
you will nd contact information and geographic focus. It will also provide a link to the foundation’s website, where you
can do additional research to determine whether their giving focus is in alignment with the focus of your MIH-CP.
Associations
Various re and EMS associations will occasionally offer grant funding to support new initiatives, training, or capital
purchases which could support the start-up of an MIH-CP program. But in reality, they are usually more focused on being
a resource for locating new grant opportunities. For instance, and as displayed in Screenshot 3, FireRescue1 sponsors a
page on their website called FireGrantsHelp. This resource may assist in locating grants for re departments, volunteer,
and reghter grant assistance: www.regrantshelp.com.
State grants for start-up programs are not as abundant as
they used to be. State matching grants are offered through
the Emergency Medical Services Trust Fund at a 75/25
match or 90/10 match for rural service providers. Under FS
401.113 the grant funds are to be used to conduct research,
increasing existing levels of emergency medical services,
evaluation, community education, injury-prevention
programs, and training in CPR and other lifesaving rst aid
techniques. Rural providers may also use the monies for
improvement, expansion, or continuation of services.
However, this grant has experienced a steady decline in the
availability of funding through the Trust Fund.
Check with the Florida Department of Health, Emergency
Medical Service Section at 850-245-4440 and the Oce
of Rural Health at 850-245-4009 for current opportunities
or look at: http://www.oridahealth.gov/%5C/provider-
and-partner-resources/ems-grants/index.html. Again, like
federal grants, they may be focused on testing a specic
concept within a community paramedicine program or a
health issue that a community paramedic could potentially
address.
Many MIH-CP have been started with grant funding from
a local source. The Emergency Medical Services Trust
Fund also provides monies to the counties for emergency
services. When starting your program, work with your
community and local government to see what may be
available to help address a community health need.
C h a p t e r 0 5

49
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Screenshot 3
Screenshot 4
If you click on the Lowe’s link in Screenshot 3, you’ll nd additional information. Screenshot 4 shows you what you’ll nd:
As you can see, it gives you enough baseline information to see if you may be eligible for the grant. However, if you
want more information or assistance with the grant, it is only available to members subscribing to FireRescue 1 services.
Alternatively, you could go directly to the Lowe’s page and do a detailed analysis of the opportunity.
C h a p t e r 0 5

Insurance Partners Florida Model National Model
Set up
Organization started and designed based on
the partnership
Collaboration between the City of Pittsburgh
and its bordering 36 municipalities. Started to
address the nancial burdens certain patients
were having on EMS agencies. Established a
countywide resource team – no single EMS
agency runs the program.
Services
Chronic care; transitional care; advanced
illness management, health risk assessments;
and unplanned urgent/emergent care
Chronic disease management for diabetes,
asthma, and chronic heart disease
Target Market
Insured patients with Medicare Advantage or
Affordable Marketplace Healthcare
Referrals from EMS agencies, hospitals,
University of Pittsburgh Medical Center, and
Highmark Blue Cross Blue Shield
Insurance Partners Florida Blue and Aetna
Blue Cross Blue Shield and one other leading
health insurance provider
Funding
Capital funding upfront monies from insurance
provider in the Medicare Advantage population.
Marketplace Healthcare was primarily a fee
for service billing. Additional fee for service
models were added to Medicare population as
the program grew.
Funding from health insurance providers
50
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Some partners are willing to invest in a MIH-CP program
because of a strategic advantage it will create, or nancial
savings it can generate for them. We’ve all heard about
hospitals being charged signicant nes for hospital
readmissions. And a few Florida MIH-CP have partnered
successfully with hospitals to reduce readmission rates.
Most of the Florida MIH-CP we interviewed have had little
luck getting hospitals to invest signicantly in an MIH-CP
despite the programs ability to help reduce readmission
rates and subsequent hospital penalties.
However, insurance companies have been investing in
and testing the MIH-CP model to determine if the model
improves their members’ health and reduces the overall
cost of providing care. Table 9 presents a brief summary
of some of the characteristics of a Florida MIH-CP
program, Evolution Health, and the CONNECT Community
Paramedic program, a national model, who created funding
partnerships with insurance companies.
According to Dan Swayze, Vice President and COO of the
Center for Western Medicine of Western Pennsylvania,
Inc. and project manager for the CONNECT Community
Paramedic program, rural EMS agencies are often too
small to work individually with insurance companies. They
are usually looking for geographic markets with a higher
concentration of their members.
Discussions have been ongoing with the Florida Association
of Health Plans to engage and partner with the association
and their members on MIH-CP programs across the state.
Finally, keep in mind that some partner funding can be in-
kind donations. Even if your partners cannot provide cash
funding, they may be able to provide equipment, supplies,
and other items helping to offset your cash outlays.
Partner Funding
Table 9: Characteristics of MIH-CP and Insurer Partnerships
C h a p t e r 0 5

51
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
SeventyFour/Shutterstock.com
Client Funding
Another source of funding is revenue from the patients or
clients receiving the care. There is a new MIH-CP in Florida
who recently launched their program using only patient pay
as their ongoing revenue source. They have designed a model
with enough client value that patients are willing to pay for
the service without using third-party payers. Unfortunately,
generating sucient revenue to support your program is
unique, but something you should also consider when you
develop your program.
Medicare/Medicaid Reimbursement
Unfortunately, Medicare and Medicaid programs do not
reimburse for community paramedics in the State of Florida
at this time. They will reimburse for services which include
treatment if the patient is transported to a medical receiving
facility. The patient must be transported. The reason for
this is Medicare and Medicaid only reimburse for the actual
transportation of a client by EMS/Paramedics/EMT’s.
Some MIH-CP Programs will try to get around this
reimbursement issue by using other types of medical providers.
If this is something you want to consider, we strongly suggest
you work with an attorney with expertise in this area to
make sure you are in compliance. The penalties for violating
Medicare/Medicaid laws are signicant and not to be taken
lightly.
Budget Narrative
Depending on the complexity of your budget, you may want to
include a budget narrative in your plan. The narrative simply
explains to the reader anything you want them to know about
the budget. For example, you may want to explain how you
calculated a gure (i.e., employee benets), or variances from
previous year gures, or if it is a 3-year budget, the differences
in gures between each year. The narrative can also be helpful
for you in the event you want to make changes or to analyze
year-end performance.
Appendix A is an outline for a complete business plan.
C h a p t e r 0 5

52
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Chapter 5 References and Resources
1. Investopedia, https://www.investopedia.com/ask/answers/072815/what-difference-between-recurring-and-
nonrecurring-general-and-administrative-expenses.asp
2. Community Tool Box: Writing a Grant Application for Funding: https://ctb.ku.edu/en/writing-grant-application
3. Another grant resource is Grant Station. It is a member-based program: https://grantstation.com
4. NEMSIS and EMSTAR are good resources for comparison data to support grant proposals: https://nemsis.org/
and http://www.emstar.org/
5. Medicare Benet Policy Manual, Chapter 10 - Ambulance: https://www.cms.gov/Regulations-and-Guidance/
Guidance/Manuals/downloads/bp102c10.pdf
6. Medicare Claims Processing Manual, Chapter 15 - Ambulance: https://www.cms.gov/Regulations-and-
Guidance/Guidance/Manuals/Downloads/clm104c15.pdf
7. The American Ambulance Association has a strong advocacy program for championing changes to the
Medicare and Medicaid laws. You can follow their efforts and changes in the laws at this site: https://
ambulance.org/advocacy/.
8. Even though you may not be able to get Medicare/Medicaid reimbursement for MIH-CP programs, there is a
current program through the Agency for Health Care Administration (AHCA) to seek additional reimbursement
for Medicaid transports: Public Emergency Medical Transportation (PEMT) Supplemental Reimbursement
Program. There are very specic qualication requirements, such as you must be an emergency medical
transport provider, enrolled as a Medicaid provider, and owned or operated by an eligible governmental entity.
The reimbursement does not cover recipients enrolled in a Florida Medicaid Managed Care Plan, non-fee
service transports, and non-transports. Utilizing this program might be a way to infuse new money into your
EMS organization to internally support a MIH-CP program. The 2 links below provide additional information and
access to Excel spreadsheets for the PEMT:
■ Agency for Health Care Administration: http://ahca.myorida.com/medicaid/Finance/nance/LIP-DSH/PEMT/index.
shtml
■ Florida Fire Chiefs Association: https://www.ffca.org/pemt-public-emergency-medical-transportation-supplemental-
reimbursement-program
9. The Minnesota Department of Health offers an EMS toolkit with resources that help to address common
issues faced by rural EMS organizations:
■ The Funding and Finances tools include nding grants, writing grant proposals, fundraising ideas, and a very
detailed budget spreadsheet: http://www.health.state.mn.us/divs/orhpc/resources/ems/funding.html
10. Florida Association of Health Plans, Inc. http://www.fahp.net/
11. NAEMT’s Mobile Integrated Healthcare and Community Paramedicine (MIH-CP) 2nd National Survey: http://
www.naemt.org/docs/default-source/2017-publication-docs/mih-cp-survey-2018-04-12-2018-web-links-1.
pdf?Status=Temp&sfvrsn=a741cb92_2
12. Article in JEMS magazine, January 17, 2015 on the CONNECT Community Paramedicine program: How
Pittsburgh’s Community Paramedic Program Links Patients to the Correct Care by Dan Swayze, Dr.PH, MBA,
MEMS. http://www.jems.com/articles/print/volume-40/issue-1/features/how-pittsburgh-s-community-
paramedic-pro.html
C h a p t e r 0 5

53
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k C h a p t e r 0 6
CHAPTER 6
What Difference Did You Make?
This Chapter discusses techniques for assessing whether your program is making a difference in the lives of your patients, in the
population you serve and in your community.
It’s important to know if your program is making a
difference. It’s important to you – you want to know
if you’re successful or not! It’s also important to your
clients, stakeholders, and funders. Whether or not you
are making a difference is where the rubber hits the
road.
After you have identied needs, engaged stakeholders,
decided on an intervention, the next step is to decide
how you will measure the success of your program.
How did it make a difference to the people you
served? Whether or not your program was a success
depends on how well you met your goals. Performance
measures operationalize your goals allowing you to
assess your performance. Sharing the results of your
assessments is one way to share your success story with
internal and external stakeholders and to satisfy the
requirements of grants and contracts for service.
What difference did you make?
Look at realistic metrics based your
population and make sure it serves the
mission of your program. Utilize data
to bridge information gaps, evolve the
practice of patient care, and improve
patient outcomes.
Melissa McCarthy
City of Gainesville Florida Community Paramedicine

Patient experience
74%
Patient healthcare
service utilization post
MIH-CP enrollment
67%
Patient healthcare service
utilization during MIH-CP
enrollment
83%
Patient health status
72%
Income Data
Expenditure data
Other
20%
30%
7%
Patient pre-MIH-CP
enrollment healthcare
service utilization
(911, ED, hospital
admissions/readmissions)
76%
Patient demographics
92%
54
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k C h a p t e r 0 6
Four things to remember: It is much easier to dene
your measures up-front, so you can capture the
information required as you operate your program. It
is much harder, if not impossible, to retrot or force
your data into a performance measure later. Second,
if you are funded by a contract or grant, your funding
agency will likely require performance measures. Third,
you should measure what’s important. Performance
measures must be relevant and responsive to the
health needs you are meeting and the evidence-based
intervention you are providing. Finally, use your
performance measure data as grist for your quality
management program. Engage staff and stakeholders
in a plan, do, check, and act improvement cycle if you
nd areas for improvement.
Performance measures ow from your mission,
strategies, and objectives and are important to
determine the difference you make to the people you
serve. Developing the mission, strategies, objectives,
and performance measures sequentially allows you
to see how they t together. Taken collectively your
mission, strategies, objectives, and performance
measures are SMART:
■ S for Specic
■ M for Measurable
■ A for Achievable
■ R for Relevant
■ T for Time-bound
Performance Measures
Data Collection
Data collection and analysis is the lifeblood of performance measures. Without establishing a strong data collection and
analysis process the accuracy and reliability of your outcomes and the overall value of your program can be questionable.
Table 10 describes the types of data collected by the 129 MIH-CP programs surveyed as part of the NAEMT’s Mobile
Integrated Healthcare and Community Paramedicine (MIH-CP) 2nd National Survey. Keep in mind these collection
points are based on what their goals and what they have determined is important to measure. What you need to
collect will depend on how your program design.
Table 10: Data Collected BY MIH-CP Programs
What Data is
Collected?

55
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
The survey also asked respondents what methods they
used to document client interactions. About half (47%)
used EMS electronic patient care reports (ePCR) systems,
39% used shared electronic patient records systems
(like with a hospital or primary care provider), 25% use
commercially available MIH-CP specic systems, 21%
use locally developed electronic record systems (word
processing, spreadsheets), and 13% use pen/paper
method. You will need to evaluate your resources, access
to systems, what data you want to capture, and staff
capabilities to determine the methods most effective for
your program.
Another question is with whom should the data be shared?
First, your staff and then your stakeholders. A best
practice identied among respondents to NAEMT’s survey
is the bi-directional sharing of data between the MIH-CP
Program and its stakeholders. Two-thirds of the MIH-CP’s
surveyed reported bi-directional sharing of patient health
information. This bi-directional data sharing is an integral
part of a successful program.
Several tools and examples of performance measures
are available. They run the gamut from simple and
easy to use to complex and resource intensive. A
brief description of a few is provided, and you can nd
additional information on them in the resources section
at the end of this Chapter. An important consideration is
that all performance measures must be relevant to your
organization and your community, and logically ow from
the intervention your program is implementing.
The Community Paramedicine Evaluation Tool (CPET),
published in 2012 by the federal Department of Health
and Human Services, Health Resources and Services
Administration, Oce of Rural Health Policy, provides a
comprehensive program evaluation tool. It is designed
for programs to use to evaluate an existing program or for
programs who are considering starting a MIH-CP program.
The CPET is organized around three core functions of
assessment, policy development, and assurance under
which benchmarks and indicators are described. Each
benchmark (performance measure) is scored on a scale
from 1 to 5, with 5 representing a “perfect score.” Scoring
a ve is ideal and found in best practices. A link to the
CPET is found at the end of this Chapter in references and
resources.
As previously noted, the development and operation of
a MIH-CP program is a process, a marathon not a sprint,
and not all programs will reach a score of 5 for each
benchmark. Using the tool in your program’s continuous
quality improvement is a good start. If you notice a less
than adequate response to a benchmark, start a plan,
do, check, and act quality improvement cycle. Engage
your stakeholders and advisory group to decide which
benchmarks are appropriate to your program, measure
them, and then strive to reach a score of 5.
Finally, take the time to create and document your database and data collection variables and processes. Set standards,
monitor trends, and make program changes if appropriate. Become a data-driven organization.
Measuring Performance
Community Paramedicine Evaluation Tool
You don’t need to go for the 100%
solution, even a 5 – 10% improvement
means the client is better than they were
before.
Lauren Young
C h a p t e r 0 6

56
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
NAEMT MIH-CP Program Toolkit
The NAEMT MIH-CP Program Toolkit contains sample
performance measures that represent the consensus
of a 2015 expert group that had input from over
75 EMS and healthcare associations. The intent of
the performance measures is to assist programs in
documenting their value to their clients, community,
insurance companies, public payors, foundations, and
other payors like federal, state, and local grantors.
The development of the performance measures was
guided by a Steering Committee that included Matt
Zavadsky of MedStar Mobile HealthCare, Brenda
Staffan of REMSA, Dan Swayze of the Center for
Emergency Medicine of Western Pennsylvania, Brian
LaCroix of Allina Health EMS, Gary Wingrove of Mayo
Clinical Medical Transport and Dr. Brent Myers,
former medical director of Wake County EMS.
As presented in the NAEMT MIH-CP Program Toolkit’s
outcome measures, the measures are organized into
two domains each with multiple subdomains. The
two domains and selected subdomains include the
following:
1. Structure/Program Design Measures
a. Executive Level Commitment
b. Needs Assessment/Gap Analysis
c. Resource Identication
d. Stakeholder Engagement
2. MIH-CP Program Measures
a. Quality of Care & Patient Safety Metrics
b. Experience of Care Metrics
c. Utilization Metrics
d. Cost of Care Metrics – Expenditure Savings
e. Balancing Metrics
More information, as well as a description of how
the MIH-CP Program Toolkit outcome measures
were developed, may be found at http://www.naemt.
org/initiatives/mih-cp/mih-cp-program-toolkit.
When you reach the site, look for the following
headings: Assessing the Value and Outcomes of
EMS-Based Mobile Integrated Healthcare Programs,
Measurement Strategy Overview, MIH Measures
Workbook and MIH Measures Workbook Example.
Revisiting the NAEMT’s MIH-CP Program Toolkit’s outcome
measures, Matt Zavadsky categorized these measures as
falling into three basic groups. These are the program
structure, process, and outcomes. These three categories
align with the classical work of Donabedian who theorized
that quality of care might be assessed by examining the
structure, process, and outcomes of care. Some things to
consider in assessing quality in each of these categories, but
by no means exhaustive, are the following:
1. Program Structure – How is the program organized?
Are sucient resources allocated to meet the program’s
goals? Are staff in place to carry out the program? Is the
necessary equipment available and in working condition?
2. Program Processes – These are related to how the
program works and how you carry out your best practice
or evidence-based intervention. Standard operating
procedures are key.
3. Outcomes – These are described in terms of the
difference you made in the lives of the people in your
program. Did the client get their blood pressure under
control? Did they report an improvement in their quality
of life or self-perceived health status? Was there an
improvement in the client’s instrumental activities of
daily life? Sometimes called an intermediate outcome,
did the client’s risk for a condition decrease, for example,
did they quit smoking?
City of Gainesville Florida Community Paramedicine
C h a p t e r 0 6

57
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
INSTITUTE FOR HEALTHCARE IMPROVEMENT, TRIPLE AIM INITIATIVE
Another taxonomy for categorizing quality domains is dened by the Institute for Healthcare Improvement (IHI) in their
Triple Aim Initiative. The IHI denes three domains of quality that collectively are referred to as the Triple Aim; these are
the following:
1. Population Health
2. Patient Experience
3. Per Capita Cost
1. Population Health
There are several options for assessing your program’s impact on the health of the population you serve. The interviews
conducted with 11 Florida MIHP Programs revealed that most programs who assessed the impact of their programs on the
health of a population used self- assessed health status, health-related quality of life metrics, and limitations of activity.
Other Population health measures may be focused on your target population’s general health and wellbeing. Equally
as important, these measures may be specic to your target population’s evidence-based intervention. The following
narrative presents a description of the different tools to assess population health.
A. Self-Assessed Health Status
According to the federal Centers for Disease Control and Prevention (CDC), self-assessed health status is a validated
and useful measure of how a person perceives their health. Respondents are asked to rate their health as excellent,
very good, good, fair, or poor. It is assessed with a single question - Would you say your general is excellent, very
good, good, fair, or poor?” Self-Assessed Health Status is assessed upon entry into and discharge from your MIH-CP
program.
This measure is part of the National Health Interview (NHI), a large sample survey of the U.S. population. It is useful if
you’d like to compare your program’s clients to the general U.S. population. In the resources section at the end of this
Chapter, there is a CDC link for additional information.
B. Health-Related Quality of Life
CDC describes Health-Related Quality of Life as a function of three modules of questions as follows:
1. Healthy Days Core Module (4 questions)
a. Would you say that in general, your health is excellent, very good, good, fair, or poor?
b. Now thinking about your physical health, which includes physical illness and injury, for how many days
during the past 30 days was your physical health, not good?
c. Now thinking about your mental health, which includes stress, depression, and problems with emotions,
for how many days during the past 30 days was your mental health not good?
d. During the past 30 days, for about how many days did poor physical or mental health keep you from
doing your usual activities, such as self-care, work, or recreation?
2. Activity Limitations Module (5 questions)
a. Are you limited in any way in any activities because of any impairment or health problem?
b. What is the major impairment or health problem that limits your activities?
c. For how long have your activities been limited because of your major impairment or health problem?
d. Because of any impairment or health problem, do you need the help of other persons with your
personal care needs, such as eating, bathing, dressing, or getting around the house?
e. Because of any impairment or health problem, do you need the help of other persons in handling your
routine needs, such as everyday household chores, doing necessary business, shopping, or getting around
for other purposes?
C h a p t e r 0 6

58
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
3. Healthy Days Symptoms Module (5 questions)
a. During the past 30 days, for about how many days did pain make it hard for you to do your usual
activities, such as self-care, work, or recreation?
b. During the past 30 days, for about how many days have you felt sad, blue, or depressed?
c. During the past 30 days, for how many days have you felt worried, tense, or anxious?
d. During the past 30 days, for how many days have you felt you did not get enough rest or sleep?
e. During the past 30 days, for about how many days have you felt very healthy and full of energy?
Health-related quality of life is assessed upon entry into and discharge from your MIH-CP program. The CDC provides a
wealth of information about Health-Related Quality of Life measures at https://www.cdc.gov/hrqol/hrqol14_measure.htm
C. Limitation of Activity
Whether a person can carry out usual day-to-day activities is the focus of limitation of activity measures. Part of
CDC’s NHI, these measures ask respondents about their limitations and, as seen above, is considered a quality of life
measure. These surveys drill down into the type and degree of limitations an individual is experiencing. Limitations
of activity would be assessed upon entry into and discharge from your MIH-CP program.
Limitation of activity is assessed by asking people about their limitations in:
• Activities of daily living (such as bathing/showering, dressing, eating, getting in and out of bed, walking, using the
toilet)
• Instrumental activities of daily living (such as using the telephone, doing light housework, doing heavy
housework, preparing meals, shopping for personal items, managing money)
• Play, school, or work
• Remembering
• Any other activity that they cannot do because of limitations caused by physical, mental, or emotional problems
Additional information is available by clicking on the CDC link in the references resources listed at the end of this Chapter.
2. Patient/Client Experience
Assessing your client’s experience is commonly accomplished by administering a client satisfaction survey. There are
standard questions from various sources that you might use to construct a patient satisfaction survey. Typically, these
surveys include the following types of questions that are ranked on a Likert-like scale from 1 – 5 with more points
awarded for a positive patient experience. Client satisfaction would be assessed upon entry into and discharge from your
MIH-CP program.
Potential categories of questions relate to access to care, provider interaction and rapport, ability to make an
appointment or been seen, if you get a prompt return of phone calls, whether the provider listens and takes the time
to understand you, whether the provider explains your care and answers your questions, and if the client thinks the
provider gives advice and treatment. A sample client satisfaction survey is included in Appendix F.
Other areas that impact the client’s experience are related to the organization’s provision of safe, effective, timely,
ecient, equitable, and patient-centered care. For more information about these six dimensions of healthcare, see the
Institute Medicine’s report titled Crossing the Quality Chasm: A New Health System for the 21st Century. This report was
published in 2011 by the Institute of Medicine, National Academies Press; despite its age, its contents are enduring.
C h a p t e r 0 6

Number
Number of ambulance transports by enrolled patients 12 months post-graduation 1, 750
Number of ambulance transports by enrolled patients 12 months pre-enrollment 3,700
Average payment per transport $421
Expenditure per CP patient contact $ 75
Number of CP patient contacts for enrolled patients 4,750
59
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
3. Per Capita Cost – Demonstrate Cost Saving/Cost Avoidance
The need to demonstrate the value of an MIH-CP is becoming increasingly more important. Funders, insurers,
stakeholders, and other partners want to know the cost saving associated with your program. The NAEMTs MIH-CP
Program Toolkit included outcome measures that might be used to demonstrate the cost savings associated with your
MIH-CP program. These are the following:
1. Ambulance Transport Saving
2. Hospital Emergency Department Visits
3. All-cause Hospital Admissions
4. Hospitalization Average Length of Stay
The following example on Ambulance Transport Savings displayed in Table 11 was taken from the NAEMTs MIH-CP
Program Toolkit. The variables of interest are the number of ambulance transports by enrolled patients 12 months
pre-graduation and the number of ambulance transports by enrolled patients 12 months post-graduation. Two
measurements are used, one pre-intervention and the other post-intervention. The pre-intervention group is dened
as enrolled patients 12 months pre-enrollment, and the post-intervention group is the number of enrolled patients 12
months post-graduation.
Using the data in Table 11, the following calculations are completed:
1. the cost associated with the number of ambulance transports by enrolled patients 12 months post-
graduation is $736,750 (1,750 X $421)
2. the cost associated with the number of ambulance transports by enrolled patients 12 months pre-
graduation is $1,557,700 (3,700 X $421)
3. the cost of CP patient contacts for enrolled patients is $356,250 (4,750 X$75)
Making a case for the MIH-CP Program, one would say that based on a pre and post-enrollment assessment of the
frequency and cost of ambulance transport among enrolled patients, there was a cost savings of $1,557,700. If one
considers the cost of CP patient contacts, the savings is $1,201,450.
Table 11: Ambulance Transport Savings
The goal is to reduce expenditures for unplanned ambulance transports to an ED pre and post-enrollment or per event.
C h a p t e r 0 6

60
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Intervention-specic performance measures are used
to assess the impact your program (intervention) has
on the clients you serve. If you are implementing
an evidence-based practice, other programs have
demonstrated the ability of the intervention to have
the desired effect. If an evidence-based practice is not
available or is unacceptable to your clients, consider a
best-practice.
If your community is experiencing the effects of
tobacco use that include high morbidity and mortality
due to tobacco-related cancers and chronic lung
disease and your planned program/intervention is a
tobacco cessation program, you could structure your
performance measure as follows:
Goal: Reduce illness, disability, and death related to
tobacco use and secondhand smoke exposure.
Objective: By the end of the rst year of operation,
50% of clients who were screened positive for tobacco
use received tobacco cessation counseling.
Performance Measure: Percentage of clients who
are screened positive for tobacco use and who receive
tobacco cessation counseling.
Numerator: The numerator would be the number of
clients who were both screened for tobacco use and
found to use tobacco who were offered a cessation
intervention.
Denominator: The denominator is all clients who were
screened and are positive for tobacco use.
Note: The tobacco related goal is consistent with the
CDC’s Healthy People 2020 goal. Smoking rates are a
statistic the State Health Department tracks and the
focus of county health departments’ efforts making
this a good area for collaboration. Using the format
presented above will help you hone in on and opera-
tionalize your goal.
So far, we’ve talked about measuring performance
using a quantitative or numbers approach. However, if
you restrict your approach to just numbers, you’ll miss
some valuable information and insights.
Numbers alone cannot capture the impact that you
have on the clients you serve. If you want to know
the difference you make in the lives of the people
you care for, ask them. Clients and their caregivers
are treasure troves of information. Focus groups or
personal interviews, known as qualitative techniques,
are useful to gain an in-depth look at the impact of your
program. You may know that 60% of your clients with
diabetes have elevated hemoglobin A1Cs. But, do you
know why? That information is only available from your
clients.
Qualitative techniques may involve collecting data from
stakeholders (local providers, county commissioners,
insurers, etc.). This data can give you insights into what
these groups value. If your stakeholders gain a better
understanding of the value of your program, it may lead
to new sources of funding.
Don’t overlook the power of anecdotal information.
When you hear a personal story about the impact
and success of your program, capture and share it.
Share it with staff, your clients, and your stakeholders.
Qualitative approaches are essential to understanding
the need for and the impact of your program especially
your client’s feelings and the value they place on your
services. Stories are powerful; they put faces on the
numbers providing context and meaning. Use them to
breathe life into the numbers.
Intervention-Specic Performance Measures
It’s Not All Numbers
GaudiLab/Shutterstock.com
C h a p t e r 0 6

61
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Chapter 6 References and Resources
1. Oce of Financial Management, State of Washington. Performance Measure Guide found at https://ofm.
wa.gov/sites/default/les/public/legacy/budget/instructions/other/2009performancemeasureguide.pdf
2. Steve Jacob, “EMS Loyalty Program” Slashes Emergency Room Trips, Saves Millions, D Health Daily, 2/12/2014.
This article provides insight into the savings MedStar has seen with their CP program. http://healthcare.
dmagazine.com/2014/02/12/ems-loyalty-program-slashes-emergency-room-trips-saves-millions/
3. NAEMT’s Mobile Integrated Healthcare and Community Paramedicine (MIH-CP) 2nd National Survey:
http://www.naemt.org/docs/default-source/2017-publication-docs/mih-cp-survey-2018-04-12-2018-web-links-1.
pdf?Status=Temp&sfvrsn=a741cb92_2
4. NAEMT MIH-CP Program Toolkit. Available at
http://naemt.org/initiatives/mih-cp/mih-cp-program-toolkit
5. CDC, Self-assessed Health Status
https://www.healthypeople.gov/2020/about/foundation-health-measures/General-Health-Status#selfAssessed
6. Crossing the Quality Chasm: A New Health System for the 21st Century. Committee on Quality of Health
Care in America, Institute of Medicine. Washington, DC, USA: National Academies Press; 2001. Available at
http://www.ihi.org/resources/Pages/Publications/
CrossingtheQualityChasmANewHealthSystemforthe21stCentury.aspx
7. The CDC provides a wealth of information about Health-Related Quality of Life measures at
https://www.cdc.gov/hrqol/hrqol14_measure.htm
8. To learn more about Donabedian see the article titled Donabedian’s Lasting Framework for Health Care
Quality available at
https://sph.umich.edu/glc/news/pdf/Donabedian NEJM 2016.pdf
9. A Guide to Measuring the Triple Aim: Population Health, Experience of Care, and Per Capita Cost. Available at
http://www.ihi.org/resources/Pages/IHIWhitePapers/AGuidetoMeasuringTripleAim.aspx
10. A discussion of evidence-based practices and how they differ from best practices may be found at
http://www.communitygrantsnow.com/2011/08/30/evidence-based-practices-vs-best-practices/
C h a p t e r 0 6

62
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
CHAPTER 7
Sustaining Your Program
grant funds to operate your program beyond one
or two years is unlikely. In Chapter 5 we discussed
different funding sources. You should be continually
evaluating alternative funding sources, models and
partners to stabilize and diversify your ongoing revenue
stream.
You’ll notice the Budget template has two years. For
sustainability, it’s helpful to think about your revenue
and expenses beyond the rst year. Please keep in
mind, while grants can be very helpful to get started,
you should not rely solely on funding your program
with grants. The likelihood of continuing to receive
Funding
Make sure you have financial
sustainability because that’s the main
reason programs go away.
Matt Zavadsky
Sustaining a community paramedicine program is the most dicult part. Many organizations have shown great results
from their MIH-CP but have been unable to sustain the program over time for various reasons.
Of the 129 programs responding to the NAEMT’s survey, the majority (40%) reported they had been in operation for
three or more years. Of the remaining respondents, their time of operation, 22% reported 2-3 years, 23% reported 1-2
years, and 15% reported being in operation for 1 year or less.
Here are some of the sustainability issues you should consider as you develop and operate your MIH-CP program.
Manatee County Florida Community Paramedicine
C h a p t e r 0 7

63
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Changes in Medicare/Medicaid Regulations
At some point, changes in the Medicare and Medicaid regulations will enable MIH-CP Programs to bill for
and be reimbursed for services other than emergency transport. When it does happen, this will signicantly
impact the ability of MIH-CP programs to be nancially sustainable. You can stay informed on this topic
through the Florida Ambulance Association or American Ambulance Association.
Another sustainable issue is stang. As
previously mentioned, the emergency
medical services industry across the country
is struggling with a paramedic shortage, and
this shortage affects an agency’s ability to
recruit staff for their MIH-CP. Staff turnover
in an emerging MIH-CP program can be very
detrimental to the consistent and effective
operation of the program. Something to
consider is whether you will staff your program
with full-time or part-time staff. Depending
on the need in your community a part-time
position may be more appropriate. Finally,
selecting the right candidates and continually
supporting their professional growth in
conjunction with program growth is crucial.
As your program matures, consider developing
a succession plan for sustainability at all levels
of the program.
Some MIH-CP programs will not be free-
standing organizations but will be a component
or division of a larger entity or service. This
usually means others may have some level of
control over the program. If this is the case,
you must be completely transparent, provide
timely and accurate data, and become the best
storyteller. With good information and stories,
they can make well informed and educated
decisions, and maybe even become a strong
advocate for your program.
Stang
Internal Support
Manatee County Florida Community Paramedicine
C h a p t e r 0 7
Make sure the individuals who make
decisions about the program know and
understand the benefits of the program.
You must continually be selling it.
Christine Long

64
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
provide a balanced voice and diversity of thought on
continuous program improvement and growth. It
enables ongoing input into the design, processes, and
results of the program.
get testimonials, have them speak at hearings about
your program, or develop marketing materials using
personal stories. Be creative in how you can engage
them in your program.
in your community. Let them know what great things
you are doing. Share client success stories, impressive
data, personal examples of your program’s work, and
educational and volunteer opportunities. This is also
an ideal way to leverage the client support mentioned
above.
If you did not use a local alliance in the development
of your program, one of the best ways to sustain your
partners and supporters is to establish one. A list
of suggested members is on page 30. Stakeholders
Clients can be your strongest voice of sustainable
support for your program. Make sure you measure
patient satisfaction and, if very positive, leverage
it within your organization, your partners, and the
community. Consider using them as volunteers,
One of the most important aspects of program
sustainability is community support. Your reputation
in the community will have either a negative or
positive impact on all aspects of your program.
Therefore, manage communications within your
community. Establish a media plan and campaign to
let the public know how you’re are making an impact
Partnership Support
Client Support
Community Support
C h a p t e r 0 7
Rural providers who wish to work with insurance
companies need to work collaboratively, even on a
regional basis, rather than try to work to carve out their
program for just the communities they traditionally
serve. If they can’t build a regional program or want to
maintain their independence, community paramedic
programs starting within rural EMS providers are
more likely to be sustainable by partnering with local
providers like nursing homes, medical practices or
health departments to target a market opportunity that
better matches their size.
Daniel Swayze

65
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Chapter 7 References and Resources
1. Florida Ambulance Association: http://www.the-faa.org/
2. American Ambulance Association: https://ambulance.org/
3. NAEMT publication: Top 10 MIH or community paramedicine
program funding sources. Available at http://www.naemt.org/initiatives/mih-cp/mih-cp-program-toolkit
4. To address the sustainable staff issue, one of the challenges is fatigue. Here is a recent article from the
National Association of State EMS Ocers on the topic: https://www.nasemso.org/Projects/Fatigue-in-EMS/
index.asp
5. The Minnesota Department of Health offers an EMS toolkit with resources that help to address common
issues faced by rural EMS organizations:
• Recruitment and Retention: http://www.health.state.mn.us/divs/orhpc/resources/ems/recruit.html
C h a p t e r 0 7

66
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k C h a p t e r 0 8
CHAPTER 8
Tying It All Together
When you write yours, you may not want to include
detail about the steps you took unless it helps the
reader understand the analysis you used to come to a
conclusion.
This case study provides an example of how to put
together your MIH-CP Program Business Plan. The
entity and community statistics/data are ctitious.
For learning purposes, this plan explains the steps
they took to come to some of the conclusions.
Case Study - Sunshine County Emergency Medical Services
Expect to spend signicant time developing your MIH-CP program. To give you a realistic idea of development and
launch time frames, according to the NAEMT’s Mobile Integrated Healthcare and Community Paramedicine (MIH-
CP) 2nd National Survey, MIH-CP programs across the country spent six months to 2 years from planning to actual
implementation. Be patient and set it up right. You’ll denitely benet in the long run.
Use the format as a guide in the development of your Plan. A template Plan outline is included in Appendix A. Again,
you need to develop and customize a Plan to t your community’s needs.
NicoElNino/Shutterstock.com

67
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
MIH-CP BUSINESS PLAN FOR SUNSHINE COUNTY EMS
1. Introduction to Sunshine County Emergency Medical Services (Sunshine EMS)
Sunshine County Emergency Medical Services (Sunshine EMS) is a government entity that covers the entire county of
Sunshine, Florida. The EMS service operates 2 ambulances during the day and 1 at night. Their staff consists of 2 full time
and 1 part time Paramedics and 2 full time and 1 part time EMT’s. In addition, they have 2 volunteer Paramedics and 3
volunteer EMT’s.
They run approximately 2,500 calls per year. Of which, 35% of the 9-1-1 calls are by residents 65 years of age and older for
fall-related injuries.
Dr. Bea Good is the medical director for the EMS service.
Population Statistics:
Located in central Florida, rural Sunshine County has a population of 96,698 residents. Critical indicators of access to
healthcare are poverty, employment, insurance status, and education. The following is a summary of these indicators for
Sunshine County:
• 37% of the county’s residents are below 200% of the poverty level.
• 38.6% of families with related children under the age of 5 are living under the poverty level (this gure is over
56% higher than the state rate of 16.8%).
• 42.5% of families with a female head of household with children are living under the poverty level.
• The current unemployment rate of 15% (1st quarter 2018) is 45.6% higher than the state of Florida at 10.3%. The
highest areas of unemployment are in the towns of Orange, Lemon, and Lime.
• As many as 21,274 residents under the age of 65 are uninsured. This equates to 22% percent of that population
segment.
• The Hispanic population has the highest uninsured rate in the county at 41.9% for 2017. This is signicantly
higher than the rate of uninsured for the county and 27% higher than the state level.
• Between 2014-2017 only 16.6% of residents aged 25 years of age and older had a bachelor’s degree, signicantly
lower than the state rate of 26.4%.
• 32% of the population are 65 years of age and older compared to approximately 18% statewide.
• The Median Household income is $39,100, which is signicantly lower than the state level of $46,956.
C h a p t e r 0 8

68
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
2. The Needs Assessment
After reviewing the county statistical data and the Sunshine EMS internal call and run report data, they have
identied the rate of falls among residents 65 years of age and older (35% of all calls) as a potential problem/need
that could be addressed by an MIH-CP program.
They searched for additional information on falls through the Florida Department of Health. This agency conducts
a Behavioral Risk Factor Survey that asks respondents to report if they had fallen in the three months before the
interview. The results of the survey indicate that individuals 65 years of age and older in Sunshine County reporting
a fall in the past three months was 8.32% compared to only 5.7% for Florida residents. Additionally, in 2016 the age-
adjusted death rate due to unintentional injuries for individuals 65 and older was 16 per 100,000 in Sunshine County
compared to 9.4 for the Florida population.
They also searched for information on falls in Florida CHARTS. The crude death rate due to unintentional falls among
the Sunshine County population 65 years of age and older is 90.13 per 100,000 compared to the Florida rate of 62.8.
The rate of falls among Sunshine County’s residents 65 years of age and older is 6.5% compared to a rate of 5.1% for
the comparable Florida population.
Community Make-Up:
• Mercy is the only hospital in the county. It has an emergency room.
• They have 2 primary care doctor oces, with a total of 4 doctors.
• There are no urgent care clinics.
• Sunnyside and Rosary are the 2 nursing homes.
• They have a hospice center aliated with the Rosary nursing home.
• There are 2 pharmacies, one aliated with a large chain, and a locally operated one.
• There are no home health services or mental health facilities in the county.
• There is a Florida public health department oce and a social services oce.
• They have 2 high schools and a satellite oce for a local community college. The satellite oce focuses
primarily on general studies, but the college does offer CNA, certications and degrees on the main campus.
• They have several civic/veteran’s organizations: Lions Club, VFW, and Kiwanis.
• There is a Senior Center which has meeting space, a game room, and provides inexpensive lunches Monday –
Friday.
• Together, the Non-Denominational, Baptist, Catholic, and Lutheran churches in the county operate a food pantry
on Thursday mornings.
• There is no dedicated transportation system in the county, but there is a taxi service.
• They have a re department and a law enforcement agency covering the county.
C h a p t e r 0 8

Sunshine County Florida U.S. Benchmark
Length of Life Ranked 60th
Premature Death 10,012 6,893 5,200
Poor Physical Health Days 4.4 3.7 2.5
Poor Mental Health Days 4.6 3.8 2.3
Health Behaviors Ranked 35th
Adult Obesity 27% 26% 25%
Adult Smoking 24% 18% 14%
Physical Inactivity 26% 23% 20%
Injury Deaths 109 69 50
Social & Economic Factors Ranked 46th
Children in Poverty 29% 25% 13%
High Power/Low Interest
Mercy Hospital
State Government Representative
High Power/High Interest
Local Government Representative
Third Party Payors
Public Health Department
Primary Care Doctor Oces
Low Power/Low Interest
Educational Institutions
Vendors
Low Power/High Interest
Sunnyside and Rosary Nursing Homes
Rosary Hospice
Senior Center
Fire/Law Enforcement Agencies
Social Service Agency
Both Pharmacies
Civic /Veteran’s Organizations
All Churches
Taxi Service
69
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
The Robert Wood Johnson Foundation provides county health ranking information. http://www.countyhealthrankings.org
They researched how Sunshine County ranks and discovered this:
Upon completion of the needs assessment, Sunshine EMS identied the problem of falls among Sunshine County residents
65 years of age and older as the focus of their MIH-CP program.
They decided to initially invite those in the High Power/Low Interest, High Power/High Interest, and Low Power/High Interest
categories to attend a presentation on their proposed MIH-CP program.
Sunshine County Health Rankings Compared to Florida and U.S. Benchmarks
3. Stakeholders
The next step was to identify the potential stakeholders they want to invite to participate in the development of their
program. Using the Power verses Interest Grid, they categorized the various community organizations/individuals to come
up with a list of potential stakeholders.
C h a p t e r 0 8

70
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
4. Program Plan
After meeting with the potential stakeholders, Sunshine EMS developed the following:
Vision: Sunshine County will be free of all preventable illness and injury.
Mission: Our mission is to eliminate injuries and deaths to individuals 65 years of age and older from falls in Sunshine
County.
Goal: Reduce illness, disability, and death related in home falls among individuals 65 years of age and older.
Strategies:
Strategy A. Raise awareness
Develop partners to get home assessment information to the target market
Offer workshops on home assessments
Strategy B: Referral System
Set up a referral system with community partners
Strategy C. Education
CDC Check for Safety Tool
Strategy D. Programming to prevent falls
Matter of Balance classes
Tai Chi classes
Yoga classes
Strategy E. Home Assessments and Remediation
Develop partners to assist with remediation efforts
Strategy F. Medication Reconciliation
Develop partners to assist in reconciling conicting medications
Matej Kastelic/Shutterstock.com
C h a p t e r 0 8

71
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Objectives and Performance Measures
The following presents two key objectives for Strategy E and the associated performance measures:
Objective 1.1: To increase the number of client homes with individuals 65 years of age and older who have completed an
at-home risk assessment from 30% to 50% within the rst year.
• Performance Measure: The number of client homes with individuals 65 years of age and older who have
completed an at-home risk assessment from 30% to 50% within the rst year.
• Numerator: The number of at-home fall risk assessments that are completed in client homes with individuals 65
years of age and older.
• Denominator: The denominator is the number of client homes with individuals 65 years of age and older.
• Baseline: In the calendar year 2017, 30% of client homes with individuals 65 years of age and older had a
completed at-home fall risk assessment.
Objective 1.2: To reduce the number of fall related 9-1-1 calls by residents 65 years of age and older from 35% to 20%
within 1 year.
• Performance Measure: The number of fall related 9-1-1 calls by residents 65 years of age and older.
• Numerator: The number of fall related 9-1-1 calls by residents 65 years of age and older.
• Denominator: The denominator is the total number of 9-1-1 calls.
• Baseline: In the calendar year 2017, the number of fall related 9-1-1 calls by residents 65 years of age and older
was 35%.
5. Alignment/Conict Evaluation:
After developing the program’s vision, mission,
goals, and strategies Sunshine EMS evaluated them
in the context of the organization’s vision, mission,
and goals for alignment. They are consistent with
the organization’s mission of providing the highest
quality of care to the citizens of Sunshine County.
The program aligns with the EMSSP, Strategic
Priority 5 by increasing the number of MIH-CP
programs in Florida and by increasing the number
of programs providing fall prevention programs in
Florida.
Also, they contacted each of the community
organizations who work with the 65 years of age
and older target market to verify the goals did not
conict or duplicate their efforts. Finding none,
they proceeded with the identied goals.
C h a p t e r 0 8
zkes/Shutterstock.com

72
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
6. Implementation Plan:
Sunshine EMS’s MIH-CP program will target the 65 years of age and older population, who has the highest rate of falls in
the county. Falls by the elderly has devastating effects on their length and quality of life, as well as burdening the county’s
emergency response system. Addressing this issue will have a positive impact on many lives and ease the use of the 9-1-1
system by this age group.
Standard Operating Procedures (SOP’s)
Dr. Bea Good has enthusiastically agreed to provide medical direction for the program. She will not charge any additional
fees for her services.
She has agreed to develop Standard Operating Procedures for the program, including general physical assessments, home
safety assessments, medication reviews and reconciliations, emergency situations, and MIH-CP enrollment and discharge
protocols. In addition, she will create a patient consent form which complies with the Health Insurance Portability and
Accountability Act for the clients and develop a quality assurance program for the protocols and program operation.
Operating Plan:
Launch Date: The MIH-CP launch date is planned for March 1, 2019.
Service Offerings:
Services will be provided to all Sunshine County residents 65 years of age or older, and shall include:
• Educational programs on fall prevention
• Programming to prevent falls
• Home assessments and remediation efforts
• Medication reconciliation
• Home health checks
• Patient navigation/advocacy
The evidence-based practices included in the program are found in the U.S. Department of Health and Human Services,
Centers for Disease Control and Prevention’s publication, Preventing Falls: A Guide to Implementing Effective Community-
Based Fall Prevention Programs.
Stang:
The MIH-CP program will have one paramedic wholly dedicated to the delivery of MIH-CP services; this includes all
administrative tasks associated with the job. The salary will be $42,000, plus benets. After consulting with the accountant
that handles payroll, the percentage of benets for this position is 22% of salary.
C h a p t e r 0 8

President/CEO of Sunshine EMS
Earl Daring
Multidisciplinary Advisory Committee
To be determined
Medical Director
Dr. Bea Good
MIH-CP
Manager/Community Paramedic
To be hired
73
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Operations:
• It will operate Monday – Friday from 8am to 5pm.
• One small used SUV will be purchased to utilize
for the program – not to exceed $15,000.
Graphics will need to be ordered and placed on
vehicle at a cost of $500.
• Insurance on the additional vehicle and
malpractice will be $1,800/year.
• No additional space will be necessary. Will
use current oce administrative support and
supplies. A new cell phone and laptop computer
will be purchased, including all Microsoft
software.
• Uniform allocation of $500 for a new employee,
and $100/year thereafter for replacement.
• Some additional medical supplies and minor
equipment will be required to stock the vehicle at
a cost of $2,000.
• Mercy Hospital, a primary care doctor, and Rosary
Nursing / Hospice have agreed to provide funding
to support ½ the annual salary of the CP and will
provide referrals to the program.
• The local pharmacist has agreed to work with
the CP and medical director on medication
reconciliation as needed and provide referrals to
the program.
• The local public health department will work in
conjunction with the CP on vaccinations, and sign
a Memorandum of Agreement.
• The Senior Center has offered space to hold
educational sessions at no cost.
• The taxi service has offered to provide discounted
rides to medical appointments for the population.
Organization Chart:
Multidisciplinary Advisory Committee:
A multidisciplinary advisory committee will be established. It will consist of a primary care physician, a hospital l
representative, a social services representative, a nursing home or hospice representative, a pharmacy representative, a
public health representative, a member of either the re or law enforcement community, and at least one lay person from
the community.
The function of the committee shall be to provide guidance on the quality of the services, the service offerings, and growth
opportunities.
Marketing/Public Relations:
The target market for our program are individuals 65 years of age and older. Our marketing approach will be two-fold.
First, direct marketing to the target population. We want people to be proactive in preventing falls.
Second, marketing to groups who work closely with the target population as a source of referrals.
A full marketing plan will be developed to implement each marketing approach. It is estimated to cost $10,000 to develop
the plan and materials to implement it.
C h a p t e r 0 8

Area of Focus Key Action Steps
Person
Responsible
Date of
Completion
Comments
A. Focus Area: Personnel and Procedures for the MIH-CP Program
A.1. Hire Community Paramedic Develop a job description Earl Daring CEO Jan. 31st 2019
Must be a licensed
Florida paramedic
Complete new employee
orientation
Earl Daring CEO Feb. 28th 2019
A.2. Establish Procedures and
Forms for Program
Develop SOP’s for the new
service offerings
Dr. Bea Good Feb. 28th 2019
Will be evaluated by
the MIH-CP Manager
after hiring
Develop quality control
measures for program
Dr. Bea Good Feb. 28th 2019
Develop HIPAA compliant
patient consent forms
Dr. Bea Good Feb. 28th 2019
A.3. Integration of Program
Evaluate the organization’s
current policy and procedures
manual for program
compliance or modications
needed
MIH-CP Manager Feb. 1st 2019
Evaluate current EMS data and
billing software systems for
use with the program
MIH-CP Manager Feb. 1st 2019
Revise the Medical Director’s
contract to include the
additional responsibilities
Earl Daring CEO Feb. 1st 2019
B. Focus Area: Multidisciplinary Advisory Committee
B.1. Establish a Multidisciplinary
Advisory Committee
Develop By-laws or Guidelines
for an Advisory Committee
MIH-CP Manager Jan. 15th 2019
Be sure to include the
meeting structure
Recruit Advisory Committee
members
MIH-CP Manager Jan. 31st 2019
Hold the rst meeting MIH-CP Manager Feb. 15th 2019
B.2. Advisory Committee
Recruitment
Develop a plan for building
new advisory members
MIH-CP Manager March 31st 2019
B.2. Maintain Advisory
Committee
Develop a system for
continuous communication
with your Advisory Committee
MIH-CP Manager Ongoing
C. Focus Area: Marketing
C.1. Marketing to Target Market
Develop a market plan for
reaching the 65 years of age
and over target market
MIH-CP Manager Nov. 15th 2018
Include timelines
& materials to be
developed
Hire a marketing company
to develop materials for the
target market
MIH-CP Manager Dec. 1st 2018
C.2. Marketing to Partners
Develop a market plan for
partners regarding reaching
the 65 years of age and over
target market
MIH-CP Manager Dec. 1st 2018
Hire a marketing company
to develop materials for the
target market
MIH-CP Manager Dec. 1st 2018
C.3. Public Relations Events
Plan a Grand Opening
community event
MIH-CP Manager March 1st 2019 Date of launch
74
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Implementation Work Plan:
C h a p t e r 0 8

Community Paramedic Program Budget Template
Categories Year 1 Year 2
Revenue
Internal Sourced Funds $ 46,000 $ 67,914
Patient/Client Payments $ - $ -
Grant/Foundation Funding $ 40,620 $ -
Partner Funding $ 25,620 $ 26,388
Total Revenue $ 112,540 $ 94,302
Expenses
Payroll Expenses
Salaries of Leader & Staff $ 42,000 $ 43,260
Percentage of Salaries for Benets $ 9,240 $ 9,517
Overtime $ - $ -
Percentage of Overtime for Benets $ - $ -
Total Payroll Expenses $ 51,240 $ 52,777
Operations Expenses
Administration
Dues & Subscriptions $ - $ -
Insurance (Facilities, Vehicles, Directors and
Ocers, Liability, Malpractice)
$ 1,800 $ 1,980
Legal Fees $ - $ -
License Fees of Staff $ - $ -
Marketing/Public Relations $ 10,000 $ 3,000
Medical Direction Contact Fees $ - $ -
Oce Supplies & Postage $ - $ -
Telephone/Internet $ - $ -
Utilities $ - $ -
Total Administration Expenses $ 11,800 $ 5,025
Facilities
Building Repairs/Maintenance $ - $ -
Communications Equipment $ 1,000 $ -
Computer Equipment $ 2,000 $ -
Lease Payments $ - $ -
Total Facilities Expenses $ 3,000 $ -
Vehicles
Fuel $ 27,000 $ 30,600
Repairs & Maintenance $ 2,000 $ 3,000
Lease Payments $ - $ -
Maintenance Contracts $ - $ -
Total Vehicle Expenses $ 29,000 $ 33,600
Miscellaneous Expenses
Meals $ - $ 200
Medical Equipment (disposable) $ 300 $ 300
Supplies (Operational) $ 500 $ 500
Supplies (Patient/Client) $ - $ -
Training (Initial) $ - $ -
Training (Continuing) $ - $ 1,500
Transportation Expenses $ - $ -
Travel $ - $ 500
Uniforms $ 500 $ 100
Other
Other
Other
Total Miscellaneous Expenses $ 1,300 $ 2,900
Total Operating Expenses $ 45,100 $ 41,525
Capital Expenses
Capital Purchases (Vehicles) $ 15,000 $ -
Renovations/Construction $ - $ -
Medical Equipment (non-disposable) $ 1,200 $ -
Other $ - $ -
Other $ - $ -
Total Capital Expenses $ 16,200 $ -
Total Expenses $ 112,540 $ 94,302
Total Revenue After Expenses $ - $ (0)
Budget:
75
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k C h a p t e r 0 8

76
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Budget Narrative:
Revenue Year 1
Internal sourced funds come from an infusion of monies by participation in the Public Emergency Medical Transportation
Supplemental Reimbursement Program for Medicaid ($28,289) and government funds ($18,011).
Grant funding from the American Health Care Association for purchase of the vehicle and ½ cost of 1st year CP salary/
benets.
Partners have committed to provide the other ½ cost of CP salary.
Expenses Year 1
Benets are 20% of salary.
Marketing includes professional design, printing cost of materials, grant opening event and other public relations events,
and vehicle graphics.
Fuel is calculated at 15,000 miles/month at 20 miles/gallon at $3/gallon
Revenue Year 2
Internal sourced funds come from an infusion of monies by participation in the Public Emergency Medical Transportation
Supplemental Reimbursement Program for Medicaid ($29,822) and government funds ($38,092).
Partners have committed to provide ½ cost of CP salary/benets.
Expenses Year 2
Salary increase 3% cost of living.
Benets are 20% of salary.
Insurance increase 10%.
License renewal for CP.
Marketing includes materials and public events.
Fuel is calculated at 17,000 miles/month at 20 miles/gallon at $3/gallon
Meals are for conferences for recertication.
Training (Continuous) is for conferences for recertication (every 2 years).
Travel includes hotel costs for recertication.
C h a p t e r 0 8

77
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
MEMORANDUM OF AGREEMENT (MOA)
Sunshine County Emergency Medical Services as the primary EMS provider for Sunshine County (EMS Provider) and Dr.
Bea Good, Medical Director for the EMS Provider (Medical Director) enter into this Memorandum of Agreement with the
Department of Health, Sunshine County (County Health Department) to encourage more effective utilization of the skills
of emergency medical technicians and paramedics by enabling them to perform, in partnership with local county health
departments, specic additional healthcare tasks that are consistent with the public health and welfare.
Notwithstanding any other provision of law to the contrary, the parties agree as follows:
1. EMS Provider paramedics or emergency medical technicians may perform health promotion and wellness activities
and blood pressure screenings in a nonemergency environment, within the scope of their training, and under the
direction of the medical director. “Health promotion and wellness” means the provision of public health programs
pertaining to the prevention of illness and injury.
2. EMS Provider paramedics may administer immunizations in a nonemergency environment, within the scope of their
training, and under the direction of the Medical Director. Appendix A, attached to this agreement, describes the
established protocols, policies, and procedures under which the paramedic will operate.
a. Medical Director will verify and document that a paramedic has the sucient training and experience
to administer immunizations. EMS Provider will maintain the training and experience verication and
documentation on the most current forms provided by the County Health Department and will make the
documentation available to the County Health Department upon request.
3. This agreement will replace any earlier documents or oral agreements between the parties as it pertains to these
specic provisions.
4. Either party must notify the other party of any necessary changes or modications to the agreement to keep the
agreement current, such as changes in the County Health Department training and experience documentation forms,
a change in the Medical Director, or modications to the protocols, policies, and procedures described in Appendix A.
5. This agreement will be effective from the date of the signature by all parties and remain in effect until one party
provides 30 days written notice to others that they desire the agreement to be cancelled.
The terms of this Memorandum of Agreement are understood and agreed upon by the EMS Provider, the Medical Director,
and the County Health Department.
EMS Provider:
_________________________________________________________________________________ Date: _______________
Earl Daring, CEO
Sunshine County EMS
Medical Director:
_________________________________________________________________________________ Date: _______________
Dr. Bea Good, Medical Director
County Health Department:
_________________________________________________________________________________ Date: _______________
Department of Health, Sunshine County
Title: _______________________________________
C h a p t e r 0 8

78
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
TEMPLATE OUTLINE FOR BUSINESS PLAN
1. Introduction
Organization
Population Statistics
Community Make-up
2. Needs Assessment
3. Stakeholders
4. Program Plan
Vision
Mission
Goals
Strategies
Objectives
Performance Measures
5. Alignment/Conict Evaluation
6. Implementation Plan
Standard Operating Procedures
Operating Plan
Launch Date
Service Offerings
Stang
Operations
Organization Chart
Multidisciplinary Advisory Committee
Marketing/Public Relations
Implementation Guide
7. Budget
Budget Narrative
Appendix A
a p p e n d i x

Community Paramedic Program Budget Template
Categories Year 1 Year 2
Revenue
Internal Sourced Funds
Patient/Client Payments
Grant/Foundation Funding
Partner Funding
Total Revenue
Expenses
Payroll Expenses
Salaries of Leader & Staff
Percentage of Salaries for Benets
Overtime
Percentage of Overtime for Benets
Total Payroll Expenses
Operations Expenses
Administration
Dues & Subscriptions
Insurance (Facilities, Vehicles, Directors and
Ocers, Liability, Malpractice)
Legal Fees
License Fees of Staff
Marketing/Public Relations
Medical Direction Contact Fees
Oce Supplies & Postage
Telephone/Internet
Utilities
Total Administration Expenses
Facilities
Building Repairs/Maintenance
Communications Equipment
Computer Equipment
Lease Payments
Total Facilities Expenses
Vehicles
Fuel
Repairs & Maintenance
Lease Payments
Maintenance Contracts
Total Vehicle Expenses
Miscellaneous Expenses
Meals
Medical Equipment (disposable)
Supplies (Operational)
Supplies (Patient/Client)
Training (Initial)
Training (Continuing)
Transportation Expenses
Travel
Uniforms
Other
Other
Other
Total Miscellaneous Expenses
Total Operating Expenses
Capital Expenses
Capital Purchases (Vehicles)
Renovations/Construction
Medical Equipment (non-disposable)
Other
Other
Total Capital Expenses
Total Expenses
Total Revenue After Expenses
79
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Appendix B
a p p e n d i x

80
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Appendix C
__________________________ EMS as the primary EMS provider for ________________, County, (EMS Provider) and ___________________
Medical Director for the EMS Provider (Medical Director) enter into this Memorandum of Agreement with the Department
of Health, ____________________ County (County Health Department) to encourage more effective utilization of the skills of
emergency medical technicians and paramedics by enabling them to perform, in partnership with local county health
departments, specic additional healthcare tasks that are consistent with the public health and welfare.
Notwithstanding any other provision of law to the contrary, the parties agree as follows:
1. EMS Provider paramedics or emergency medical technicians may perform health promotion and wellness activities
and blood pressure screenings in a nonemergency environment, within the scope of their training, and under the
direction of the medical director. “Health promotion and wellness” means the provision of public health programs
pertaining to the prevention of illness and injury.
2. EMS Provider paramedics may administer immunizations in a nonemergency environment, within the scope of their
training, and under the direction of the Medical Director. Appendix A, attached to this agreement, describes the
established protocols, policies, and procedures under which the paramedic will operate.
a. Medical Director will verify and document that a paramedic has the sucient training and experience
to administer immunizations. EMS Provider will maintain the training and experience verication and
documentation on the most current forms provided by the County Health Department and will make the
documentation available to the County Health Department upon request.
3. This agreement will replace any earlier documents or oral agreements between the parties as it pertains to these
specic provisions.
4. Either party must notify the other party of any necessary changes or modications to the agreement to keep the
agreement current, such as changes in the County Health Department training and experience documentation forms,
a change in the Medical Director, or modications to the protocols, policies, and procedures described in Appendix A.
5. This agreement will be effective from the date of the signature by all parties and remain in effect until one party
provides 30 days written notice to others that they desire the agreement to be cancelled.
The terms of this Memorandum of Agreement are understood and agreed upon by the EMS Provider, the Medical Director,
and the County Health Department.
EMS Provider:
__________________________________________________________________________EMS Date:_______/_______/________
Title: _______________________________________
Medical Director:
__________________________________________________________________________EMS Date:_______/_______/________
_____________________________________________, Medical Director
County Health Department:
__________________________________________________________________________EMS Date:_______/_______/________
Department of Health, _______________________________________ County
Title: _______________________________________
TEMPLATE MEMORANDUM OF AGREEMENT (MOA)
a p p e n d i x

President/CEO of Organization
Program Advisory Committee
Program Director
Medical Director(s)
Community Paramedic(s)
Program Analyst
81
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Appendix D
TEMPLATE ORGANIZATIONAL CHART
a p p e n d i x

“THEME”
Category Strategy
Target Market
Positioning Statement
Offering to customers
Price Strategy
Distribution
Sales Strategy
Service Strategy
Promotion Strategy
Marketing Research
Any other component of your marketing plan
Marketing Theme:
Category Strategy
My reason for existence:
What sets my business apart from the rest:
My ideal customer is: 1.
What’s most important to my ideal customer when they are
buying what I’m selling:
1.
What I want to accomplish this year: •
The top 3 things that are going to get me there: 1.
How much will each program contribute to my revenue/
protability:
1.
What will trigger my ideal customer to think of me: •
Programs I am running to reach my goal:
How much money will I need to get it done? 1.
82
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Appendix E
TEMPLATES MARKETING PLAN
These are 2 templates for a one-page marketing plan by Ivana Taylor from Small Business Trends. You can access
these templates to actually write your plan at: https://smallbiztrends.com/2008/06/one-page-marketing-plan.html.
This rst template follows the more traditional marketing plan outline.
But, sometimes it’s better to be less formal and approach marketing from a different viewpoint. This second template
is more focused on identifying and developing emotional triggers of the client.
a p p e n d i x

Please circle how well you think we are doing in the following areas:
GREAT
5
GOOD
4
OK
3
FAIR
2
POOR
1
Ease of getting care:
Ability to be seen
5 4 3 2 1
Prompt return on calls
5 4 3 2 1
Staff:
Provider:
Listens to you
5 4 3 2 1
Takes enough time with you
5 4 3 2 1
Explains what you want to know
5 4 3 2 1
Gives you good advice and treatment
5 4 3 2 1
Other Staff
Friendly and helpful to you
5 4 3 2 1
Answers your questions
5 4 3 2 1
All Others:
Friendly and helpful to you
5 4 3 2 1
Answers your questions
5 4 3 2 1
Payment:
What you pay
5 4 3 2 1
Explanation of charges
5 4 3 2 1
Condentiality:
Keeping my personal information private
5 4 3 2 1
The likelihood of referring your friends and relatives to us:
5 4 3 2 1
83
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Appendix F
TEMPLATE PATIENT/CLIENT SATISFACTION SURVEY
[Your MIH-CP Name Here]
We would like to know how you feel about the services we provide so we can make sure we are meeting your needs.
Your responses are directly responsible for improving these services. All responses will be kept condential and
anonymous. Thank you for your time.
What do you like best about our service? ___________________________________________________________________________________
_______________________________________________________________________________________________________________________________
_______________________________________________________________________________________________________________________________
What do you like least about our service? __________________________________________________________________________________
________________________________________________________________________________________________________________________________
_______________________________________________________________________________________________________________________________
Suggestions for improvement? ________________________________________________________________________________________
__________________________________________________________________________________________________________________________
_______________________________________________________________________________________________________________________________
Thank you for completing our survey
a p p e n d i x
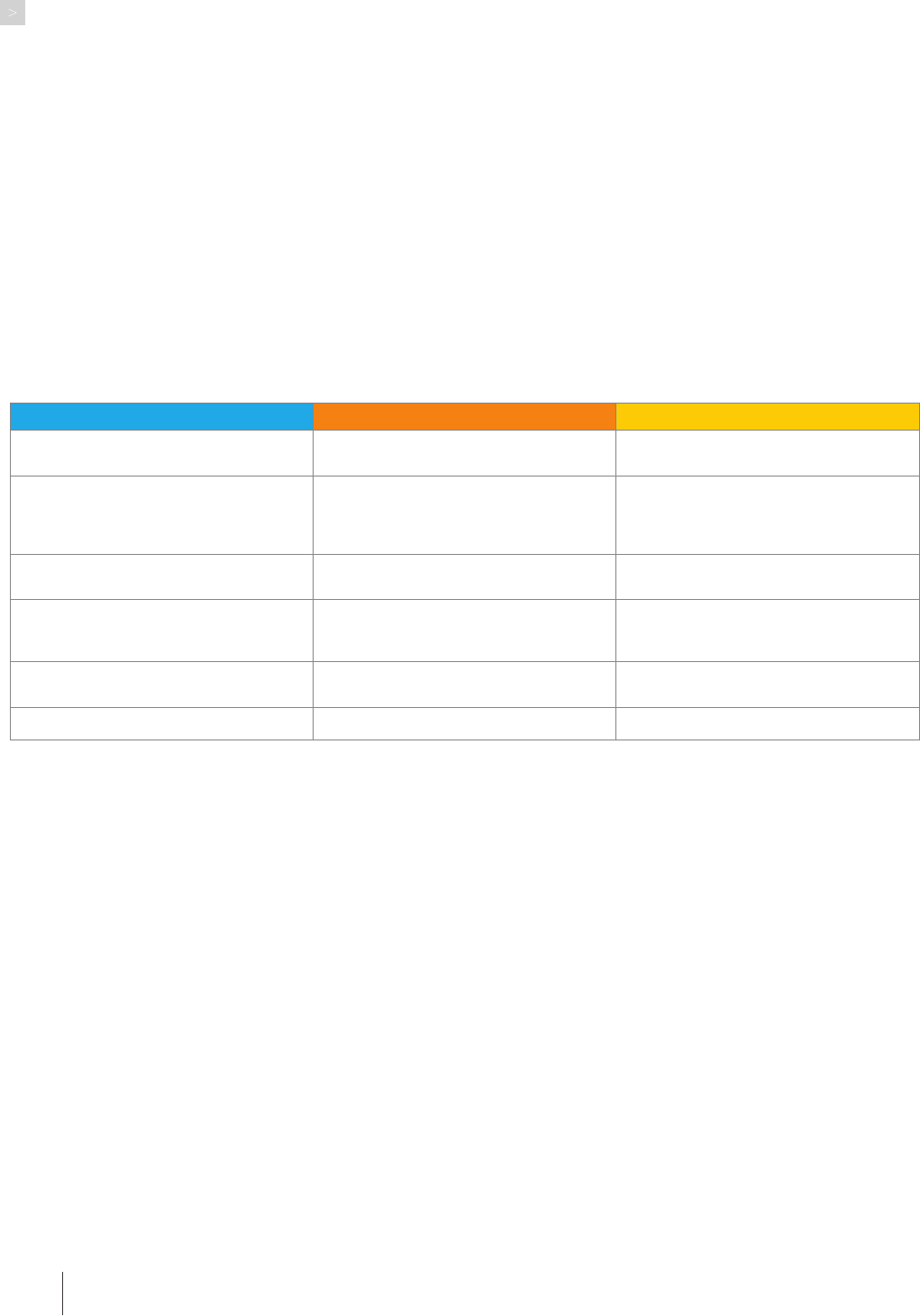
Tasks Conditions Standards
Provide comprehensive health, wellness,
and safety assessments
Caseload not more than 30 clients,
supervisor is available
95% of assessments are comprehensive
and complete
Prepare comprehensive, individualized
client care plans
Caseload not more than 30 clients,
supervisor is available for dicult
cases
Within 1 week of rst visit 95% of clients
will have a comprehensive individualized
care plan acceptable to the client and the
Medical Director
Implement and monitor client care plan
Caseload not more than 30 clients,
supervisor is available for dicult case
95% of care plans are up-to-date within 2
days
Evaluate client care plan and modify if
necessary
Caseload not more than 30 clients,
supervisor is available for dicult case
95% of client care plans evaluated and
if milestones not achieved, discuss
documentation with supervisor
Effectively communicates complex
information
Communication is routinely effective
Ensure client satisfaction Meet or exceeds 95% client satisfaction
84
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Appendix G
TEMPLATE PERFORMANCE BASED JOB DESCRIPTION
Community Paramedic Performance Based Job Description
Agency: _______________________________________
Job title: _______________________________________
Location: _____________________________________
Division/Department: ________________________
Supervised by: ________________________________
Performance-Oriented Job Description
Community Paramedic
Required Competencies
■ Ability to communicate complex information effectively
both verbally and in writing to patients, families, staff, and
providers
■ Ability to function effectively as a team member, or leader
in one’s activities
■ Knowledge of the profession’s scope of practice including
its limitations
■ Knowledge of health promotion, disease prevention,
preventive services, and chronic diseases including physical,
behavioral, social, and nancial considerations
■ Ability to conduct a comprehensive health assessment,
develop a care/intervention plan, implement the care/
intervention, and evaluate the intervention adjusting as
necessary
■ Knowledge of community resources to assist patients in
meeting their needs
■ Knowledge of computer, smartphone, tablet applications
relevant to the eld
■ Demonstration of a commitment to continuing education
and professional development
Minimum Qualications
■ Candidates must be licensed in the State of _______ as a
Paramedic with a minimum of three years’ experience.
■ Completion of a Community Paramedic education program
as required by the agency.
■ Maintain an Advanced Cardiac Life Support, CPR
certication, extrication, EVOC or equivalent, and an
insurable Driver’s License required.
■ Successful completion of ICS 100, ICS 200, ICS 700.
■ Trained, experienced, and otherwise qualied to drive
emergency response ambulances and QRV’s, maintain the
appropriate class of driver’s license.
a p p e n d i x

85
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Appendix H
SAMPLE MOBILE INTEGRATED HEALTHCARE PROVIDER REFERRAL ENTRY INTO CARE
Person Making Referral:____________________________________________________________________________ Date:____/____/__________
Agency:____________________________________________________________________________________ Phone: (_____)-_______-_____________
E-Mail:__________________________________________________________________________________________ Fax: (_____)-_______-_____________
Aliation to patient: Paramedic Provider Physician Case worker NCEMS Billing
Hospice Family Member Home Health Provider Other:______________________
__________________________________________________________________________________________________________________________________
Patient Name:_______________________________________________________________________ DOB:____/_____/_____ M F
Patient’s Full Address:__________________________________________________________________________________________________________
City:__________________________________________________________________________________ State:_________ Zip:___________________
Phone: (_________)-_________-_________ RUN # (If applicable):_______________________
Primary Medical Condition:____________________________________________________________________________________________________
Expected Discharge Date (If Applicable): _____________________________________________________________________________________
Reason for Referral: ___________________________________________________________________________________________________________
__________________________________________________________________________________________________________________________________
__________________________________________________________________________________________________________________________________
__________________________________________________________________________________________________________________________________
If possible, please include the most recent:
History and Physical
Home Medication list
Discharge instructions
12 Month Visit History with date, diagnosis, and admit status
Please send to _____________________________________________________________________ via_______________________________________
a p p e n d i x

86
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Appendix I
SAMPLE MOBILE INTEGRATED HEALTHCARE PROVIDER INITIAL CONTACT FORM
a p p e n d i x
Sample Mobile Integrated Healthcare Provider Initial Contact Form
MIHP Provider:_________________________________________________________________________________ Date:_______/_______/________
Patient’s Name:__________________________________________________________________ DOB:_______/_______/________ M F
Full Address:___________________________________________________________________________________________________________________
City:____________________________________________________________________________________________ State:___________ Zip:__________________
Phone: (_________)-____________-_____________ SS#:____________-____________-______________
Primary Care Physician:________________________________________________________________________________________________________
Specialty Physicians: ___________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________________________________
PT and other medical personnel: ______________________________________________________________________________________________
_____________________________________________________________________________________________________________________________
Number of calls prior to: _________ Insurance: ______________________________________________________________________________
Referred by:_______________________________________________________ Agency:___________________________________________________________
Prevention category: __________________________________________________________________________________________________________
Allergies:________________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________________________________
________________________________________________________________________________________________________________________________
Full Past Medical history: ____________________________________________________________________________________________________
_________________________________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________________________________
I,______________________________ agree to become client of XXX EMS, Mobile Integrated Healthcare – Community Paramedicine
Program. I understand that the goal of the program is to improve my health status and facilitate continuity of care with
my health care providers.
Client Signature:_______________________________________________________Date:_______/_______/________
MIHP Signature:________________________________________________________Date:_______/_______/________

87
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Appendix J
EXAMPLE PALM BEACH COUNTY MIH PILOT PROGRAM
Mobile Integrated Health
High Frequency EMS Caller Pilot Program
Objective: A pilot program designed to improve patient life quality, health status, and reduce reliance on EMS by those
who demonstrate high frequency use of 911.
Goals: The goals of the pilot program are to reduce the use of 911 by enrolled participants, reduce the amount of ER
transports needed for enrolled participants, reduce hospital admissions of enrolled participants, and increase access
to resources and medical care services that can most appropriately meet the needs of the patient.
Study Length: The study will start on March 1, 2018 and last for a period of 12 months.
Enrollment Criteria: 10 or more 911 calls in one month or 3 or more times in a two-week period and patient
agreement to participate.
Exclusionary Criteria: Primary diagnosis of psychiatric disability, advanced cognitive impairment/dementia, or
addiction disorder.
Study Design:
1. Patients will be identied by set criteria involving total of 911 use, circumstances of 911 calls, and location.
2. A minimum of 100 patients to be enrolled in the 12-month pilot program.
3. Patients will sign informed consent at their rst face to face visit.
4. MIH Team that will visit patients will consist of Social Workers, Paramedics, and other qualied professionals as
identied by the MIH Coordinator.
5. Data will be collected to show the number of 911 calls pre-MIH intervention and post-MIH intervention for each
enrollee as well as life quality indicators pre-MIH intervention and post-MIH intervention.
6. Data will be analyzed to show what impact the program had on patient’s life quality, health status, functioning,
and use of 911. Healthcare cost savings from reduced ER visits and hospital admissions will also be explored.
Projections:
1. Enrollment of at least 100 high frequency EMS callers who meet pilot program criteria over a 12-month period.
2. Improve enrollee perception of life quality and overall health by 50% after MIH intervention.
3. Reduce 911 use by enrollees by 60% within the 12-month pilot program.
4. Reduce ER visits by enrollees by 60% within the 12-month pilot program.
5. Reduce hospital admission of enrollees by 60% within the 12-month pilot program.
a p p e n d i x

88
F l o r i d a M o b i l e i n t e g r a t e d H e a l t H c a r e - c o M M u n i t y Pa r a M e d i c i n e P r o g r a M g u i d e b o o k
Florida Mobile
Integrated Healthcare
Community Paramedicine
Program Guidebook
Copyright © 2019 Florida Department of Health. All rights reserved.
This project was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department
of Health and Human Services (HHS) as part of an award totaling $428,942 with zero percent financed with non-
governmental sources. The contents are those of the authors and do not necessarily represent the official views of,
nor an endorsement, by HRSA, HHS or the U.S. Government.
