
Louisiana’s Medicaid Managed Care Quality
Strategy
Prepared by: The Bureau of Health Services Financing
Louisiana Medicaid
Quality Improvement, Population Health, and Health
Equity Section
September 2023

Louisiana Medicaid Managed Care Quality Strategy
i
i
Table of Contents
1. INTRODUCTION – MANAGED CARE GOALS, OBJECTIVES AND OVERVIEW..........1
1.1 History of Managed Care in Louisiana .......................................................... …..... 1
1.2 Quality Strategy Aims, Goals, and Objectives ............................................. .......... 2
1.3 Quality Management Structure................................................................................. 4
2. DRIVING IMPROVEMENT AND MONITORING PROGRESS ........................................... 5
2.1 Goals and Objectives for Continuous Quality Improvement ................................. 5
2.2 MCO Performance Measures .................................................................................... 5
2.3 Performance Measures and Performance Improvement Projects (PIPs) ............. 5
2.4 Other Medicaid Quality Interventions .................................................................... 10
2.5 Annual External Independent Reviews .................................................................. 12
2.6 Procedures for Identifying, Evaluating, and Reducing Health Disparities ......... 13
2.7 Use of Sanctions ........................................................................................................ 15
3. STATE STANDARDS FOR ACCESS AND CLINICAL POLICIES AND GUIDELINES 17
3.1 Provider Network Adequacy Standards and Availability of Services ................. 17
3.2 Adoption & Dissemination of Evidence-Based Clinical Practice Guidelines .....29
3.3 Transition of Care Policy ......................................................................................... 29
3.4 Mechanisms Used to Identify Persons with Special Health Care Needs (SHCN)
.................................................................................................................................... 30
3.5 Non-Duplication Strategy ........................................................................................ 31
4. EVALUATING, UPDATING, AND DISSEMINATING THE QUALITY STRATEGY .... 33
4.1 Quality Strategy Development and Public Comment ........................................... 33
4.2 Quality Strategy Review, Update, and Evaluation ................................................ 33
5. APPENDIX A: Louisiana Medicaid MCO Performance Measures (Measurement Year 2023
and Subsequent Years) ..............................................................
.................................................. 35

Louisiana Medicaid Managed Care Quality Strategy
1
1
1 Introduction – Managed Care Goals, Objectives and
Overview
1.1 History of Managed Care in Louisiana
Louisiana’s Medicaid managed care program is responsible for providing high-quality, innovative, and
cost-effective health care to Medicaid enrollees. Guided by the Triple Aim, the Louisiana Department of
Health (LDH) partners with enrollees, providers, and health plans to continue building a Medicaid
managed care delivery system that improves the health of populations (better health), enhances the
experience of care for individuals (better care) and effectively manages costs of care (lower costs).
More specifically, the Department’s Medicaid managed care objectives include:
advancing evidence-based practices, high-value care and service excellence;
supporting innovation and a culture of continuous quality improvement (CQI) in Louisiana;
ensuring enrollees ready access to care, including through innovative means such as medical
homes and telehealth;
improving enrollee health;
decreasing fragmentation and increasing integration across providers and care settings,
particularly for enrollees with behavioral health needs;
using a population health approach, supported by health information technology, to advance
health equity and address social determinants of health (SDOH);
reducing complexity and administrative burden for providers and enrollees;
aligning financial incentives and building shared capacity to improve health care quality through
data and collaboration; and,
minimizing wasteful spending, unnecessary utilization, and fraud.
Today, Louisiana Medicaid serves over 1.8 million Louisianans, approximately 39% percent of the state’s
population. Six (6) statewide Managed Care Organizations (MCOs), one (1) Behavioral Health Prepaid
Inpatient Health Plan (PIHP) and two (2) Dental Prepaid Ambulatory Health Plan (PAHP) pay for
healthcare services for more than 90 percent of the Louisiana Medicaid population, including more than
481,000 new adults since Medicaid expansion took effect in July 2016. These managed care entities
(MCOs) pay for Medicaid benefits and services included in the Louisiana Medicaid state Plan, state
statutes and administrative rules, Medicaid policy and procedure manuals. In addition, these MCOs also
provide specified value-added Medicaid benefits and services. Accreditation information for Louisiana’s
MCOs are posted to the Medicaid Quality Initiatives website and can be accessed at
https://ldh.la.gov/index.cfm/subhome/47. Accreditation information for Louisiana’s PIHP is posted to the
Behavioral Health Coordinated System of Care (CSoC) website and can be accessed at
https://ldh.la.gov/index.cfm/page/1342. Accreditation information for Louisiana’s PAHPs are posted to
the Dental Services website and can be accessed at https://ldh.la.gov/index.cfm/page/2067 or directly at
https://ldh.la.gov/assets/docs/BayouHealth/Dental/DBPM_Accreditation_Web_Posting_11.3.22.pdf.
On February 1, 2012, the Louisiana Department of Health (LDH) transitioned nearly 900,000 Medicaid
enrollees from the state’s 45-year-old fee-for-service (FFS) program to a Medicaid managed care model.
Rollout occurred in phases based upon designated geographic service areas, with the statewide rollout

Louisiana Medicaid Managed Care Quality Strategy
2
completed on June 1, 2012. In transitioning from fee-for-service to a Medicaid managed care model,
Louisiana sought to:
Improve access to care
Improve care coordination
Increase emphasis on disease prevention and the early diagnosis and management of chronic
conditions
Improve health outcomes and quality of care
Provide for a more financially stable Medicaid program
In 2014, LDH issued a request for proposal (RFP) for its second-generation, full-risk Medicaid managed
care contracts, with a start date of February 1, 2015. The RFP provided for an initial three-year contract
term and the option to extend the contracts up to 24 months. Subsequently, the Louisiana Legislature
approved a 23-month extension to these contracts, from February 1, 2018 through the contract expiration
date of December 31, 2019.
In December 2015, LDH integrated specialized behavioral health services into the managed care
program in an effort to improve care coordination for enrollees and facilitate provision of whole-person
health care. Louisiana also continues to administer the Coordinated System of Care (CSoC), a single
behavioral health PIHP to help children with behavioral health challenges that are at risk for out of home
placement. Wraparound support and other services are provided to assist children with staying in or
returning to their home.
In 2021, LDH initiated procurement for its third-generation, full-risk Medicaid managed care contracts.
The new third-generation, full-risk Medicaid managed care contracts with six (6) MCOs went into effect
on January 1, 2023.
1.2 Quality Strategy Aims, Goals, and Objectives
This Quality Strategy establishes clear aims, goals, and objectives to drive improvements in care delivery
and health outcomes as well as metrics by which progress will be measured. It articulates priority
interventions, and details the standards and mechanisms for holding MCOs accountable for desired
outcomes. The Quality Strategy is a roadmap by which LDH will use the managed care infrastructure to
facilitate improvement in health and health care through programmatic interventions.
Guided by the Triple Aim and the broad aims of the National Quality Strategy – Better Care, Healthy
People, Healthy Communities, and Affordable Care – Louisiana’s Quality Strategy framework defines
and drives the overall vision for advancing health outcomes and quality of care provided to Louisiana
Medicaid enrollees. Described in Table 1, these broad aims link to Louisiana specific goals and
objectives, intended to highlight key areas of quality focus for the Louisiana Medicaid managed care
program.
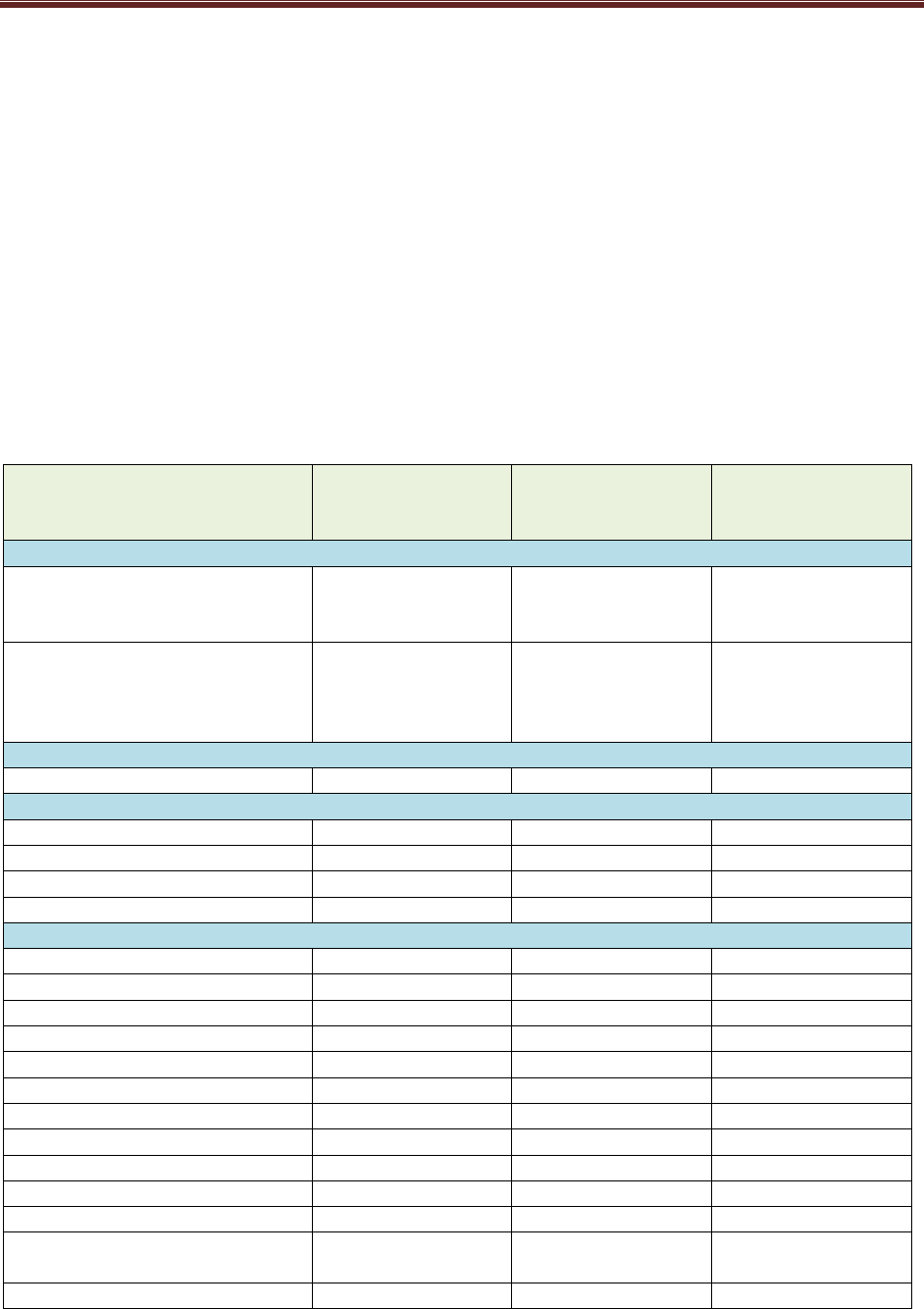
Table 1: Louisiana Quality Strategy Aims, Goals, and Objectives
Aims Goals Objectives
Better Care. Make
health care more
Ensure access to care to
meet enrollee needs
Ensure timely and approximate access to primary
and specialty care

Louisiana Medicaid Managed Care Quality Strategy
3
Aims Goals Objectives
person-centered,
coordinated, and
accessible so it occurs
at the “Right care, right
time, right place.”
Improve coordination
and transitions of care
Ensure appropriate follow-up after emergency
department visits and hospitalizations through
effective care coordination and case management
Ensure appropriate hospice onboarding and
transitioning from palliative care to hospice
Facilitate patient-
centered, whole-person
care
Engage and partner with enrollees to improve
enrollee experience and outcomes
Integrate behavioral and physical health
Healthier People,
Healthier
Communities. Improve
the health of
Louisianans through
better prevention and
treatment and proven
interventions that
address physical,
behavioral, and social
needs.
Promote wellness and
prevention
Ensure maternal safety and appropriate care during
childbirth and postpartum
Prevent prematurity and reduce infant mortality
Promote healthy development and wellness in
children and adolescents
Promote oral health in children
Improve immunization rates
Prevent obesity and address physical activity and
nutrition in children and adults
Prevent prematurity and reduce infant mortality
Improve cancer screening
Improve HIV and Hepatitis C virus infection
screening
Promote early initiation of palliative care to improve
quality of life.
Promote healthy development and wellness in
children and adolescents
Promote use of evidence-based tobacco cessation
treatments
Improve chronic
disease management
and control
Improve hypertension, diabetes, and cardiovascular
disease management and control
Improve respiratory disease management and
control
Improve HIV control
Improve quality of mental health and substance use
disorder care
Partner with
communities to
improve population
health and address
Stratify key quality measures by race/ethnicity and
rural/urban status and narrow health disparities
Advance specific interventions to address social
determinants of health

Louisiana Medicaid Managed Care Quality Strategy
4
Aims Goals Objectives
health disparities
Smarter Spending.
Demonstrate good
stewardship of public
resources by ensuring
high-value
*
, efficient
care.
Pay for value and
incentivize innovation
Advance value-based payment arrangements and
innovation
Minimize wasteful
spending
Ensure members that are improving or stabilized in
hospice are considered for discharge
Reduce low value care
*
*High value services, as defined by the Institute of Medicine, represent the “best care for the patient, with the optimal result for
the circumstances, delivered at the right price.” Low-value services represent care that does not meet these criteria.
Underpinning these aims, objectives and goals are a robust set of quality interventions/strategies and
quality performance measures that MCOs are required to measure and report progress against, as
described in Section 2, Driving Improvement and Monitoring Progress.
1.3 Quality Management Structure
The day-to-day operations of the Medicaid managed care program are the responsibility of the Bureau of
Health Services Financing within LDH, with support from all LDH “program offices” – Office of
Behavioral Health (OBH), Office of Public Health (OPH), Office of Aging and Adult Services (OAAS),
and Office for Citizens with Developmental Disabilities (OCDD). The Medicaid Quality Improvement,
Population Health, and Health Equity Section, in collaboration with these program offices, the Medicaid
Chief Medical Officer and Medicaid Executive Management Team, is responsible for the development,
implementation and evaluation of the Medicaid Managed Care Quality Strategy.
The Louisiana Medical Care Advisory Committee fulfills the role required by 42 CFR 431.12. The
Committee provides focus and direction for Medicaid program quality improvement activities to promote
access and utilization of quality, evidence-based healthcare that is designed to meet the health needs of all
Louisiana Medicaid and Children’s Health Insurance Program enrollees.
Members of the Committee and its subcommittees provide advisory insight to the Medicaid program.
This Committee provides recommendations for the delivery of high quality care. It is interdisciplinary and
includes representatives who are familiar with quality improvement and the medical needs of Medicaid
enrollees.

Louisiana Medicaid Managed Care Quality Strategy
5
2 DRIVING IMPROVEMENT AND MONITORING
PROGRESS
2.1 Goals and Objectives for Continuous Quality Improvement
LDH is committed to a culture of Continuous Quality Improvement (CQI). We require MCOs to engage
in and support CQI on clinical and administrative metrics, and work with providers and the Department to
bring innovation to all aspects of health care. We expect MCOs to evaluate the effectiveness of program
interventions and adjust continuously to optimally support whole-person centered care and improved
health outcomes for enrollees.
2.2 MCO Performance Measures
Louisiana requires MCOs to report annually on patient outcome performance measures, including the
Healthcare Effectiveness Data and Information Set (HEDIS®) quality metrics, CMS Adult and Children
Core Set, Agency for Healthcare Research and Quality (AHRQ) Prevention Quality Indicators, Consumer
Assessment of Healthcare Providers and Systems (CAHPS) measures, and state-specified quality
measures. The state may add or remove performance measure reporting requirements prior to the start of
a measurement year. Current MCO performance measure reporting requirements are described in
Appendix A. All performances measures listed in Appendix A are listed on the Louisiana Medicaid
Managed Care Quality Dashboard, which can be accessed at http://qualitydashboard.ldh.la.gov/.
Currently, one percent of each MCO’s monthly capitated payment is withheld to incentivize a core set of
quality and health outcomes (denoted in Appendix A with “$$”). The MCO may earn back the quality
withhold for the measurement year based on its performance on incentive-based measures relative to
targets as established by LDH. LDH aligns HEDIS benchmarks to NCQA Quality Compass Medicaid
National 50th percentile. Targets for non-HEDIS incentive-based measures are equal to the best
performance reported to LDH by any MCO for the prior measurement year. To earn back the full
withhold amount associated with each incentive-based measure, MCO performance must either meet the
target for that measure or improve by at least two points from the prior measurement year.
2.3 Performance Measures and Performance Improvement Projects
(PIPs)
In accordance with 42 CFR 438.340 and 42 CFR § 438.330(d), MCOs must have an ongoing program of
PIPs that focus on clinical and non-clinical areas. A PIP is intended to improve the care, services or
enrollee outcomes in a focused area of study. In addition to any CMS specified PIPs, LDH requires
MCOs to perform two LDH-approved PIPs, a minimum of one additional LDH-approved behavioral-
health PIP each contract year, and may require up to two additional projects for a maximum of five PIPs.
PIPs are designed to achieve, through ongoing cycles of enrollee input, planned intervention, and
measurement, significant improvement on priority health outcomes sustained over time.
LDH-approved MCO, PIHP, and PAHP PIPs are listed below in Tables 2 and 3.

Louisiana Medicaid Managed Care Quality Strategy
6
Table 2: Medicaid MCO Performance Improvement Projects
2021-2023 Ensuring access to the
COVID-19 vaccine among
Healthy Louisiana vaccine-
eligible enrollees
Implement interventions to achieve the following
objectives:
Enrollee Interventions
o Refer and facilitate making appointments for
eligible enrollees engaged in case
management to COVID-19 vaccination sites.
o Refer and facilitate making appointments for
eligible enrollees NOT engaged in case
management to COVID-19 vaccination sites.
o Educate and inform enrollees on vaccine
merits, safety and accessibility with
comprehensive and clear communication in
accordance with the State of Louisiana
communication plan for the COVID-19
vaccine [e.g., LDH COVID-19 website:
Louisiana Coronavirus COVID-19 |
Department of Health | State of Louisiana
(la.gov) ].
o Provide enrollees with second dose reminders
for those overdue.
Provider Interventions
o Distribute listings of COVID-19 vaccine-
eligible enrollees, as well as listings of
pharmacy vaccination sites and other LINK-
enrolled providers, to PCPs.
o Conduct training and education of providers,
when necessary, using LINKS training videos
and CDC/ACIP evidence-based guidance in
collaboration with the Tri-Regional LINKS
Outreach Coordinators.
Collaborate with state and local partners
o Outreach to racial/ethnic minority enrollees.
Utilize COVID-19 vaccination coverage
reports generated in LINKS to track and
monitor COVID-19 vaccination rates and to
determine pockets of need (e.g., zip code and
region level). Collaborate and coordinate with
the Louisiana Department of Health
Vaccination Strike Teams to vaccinate hard-
to-reach target populations in Louisiana.
o Collaborate with the Office of Public Health
on vaccine education materials.

Louisiana Medicaid Managed Care Quality Strategy
7
2023 Cervical Cancer Screening
Implement interventions to achieve the following
objectives:
Member Objective: Improve the HEDIS
Cervical Cancer Screening performance indicator
by developing and implementing interventions for
the following eligible populations ages 21-64
years:
o Eligible population of women who are in
case management.
o Eligible population of women who are not
in case management and have at least one
PCP or OB/GYN visit during the
measurement year.
o Eligible population of women who are not
in case management and have not had any
PCP or OB/GYN visits during the
measurement year. Interventions must
address provider linkage.
o Disparity subpopulations identified using
the Analysis of Disproportionate Over-
Representation (cervical cancer
prevalence) and Under-Representation
(cervical cancer screening).
Provider Objective: Improve the HEDIS
Cervical Cancer Screening performance indicator
by developing and implementing provider
interventions (must include Gaps-In-Care Report
and Provider Education).
2023 HIV Screening
Implement interventions to achieve the following
objectives:
Member Objective: Improve the HIV screening
rate by developing and implementing member
interventions for the following eligible adolescent
and adult with populations 1 through 3 screened
during the measurement year, and the last eligible
population ever screened:
o Pregnant persons or persons with
encounters for labor and delivery
o Persons with past or present injection
drug use
o Persons with contact with and (suspected)
exposure to infections with a

Louisiana Medicaid Managed Care Quality Strategy
8
predominantly sexual mode of
transmission or to human
immunodeficiency virus or persons with
high-risk heterosexual behavior, high-risk
homosexual behavior, or high-risk
bisexual behavior; This would also
include persons diagnosed with infections
with a predominantly sexual mode of
transmission
o All others aged 15 to 65 years (without a
current or past HIV diagnosis)
Provider Objective: Improve the HIV screening
rate for the total eligible population by implement
provider interventions for PCP providers and
OB/GYN/prenatal care providers
2022-2023 Dental: Fluoride Varnish
Application to Primary
Teeth of All Enrollees
Aged 6 Months through 5
Years by Primary Care
Clinicians
Implement interventions to:
Perform member outreach
Perform provider education
Prepare Member Fluoride Varnish Care Gap
Report
2022-2023 Behavioral Health
Transitions in Care
Implement interventions to improve performance
improvement of the following measures:
Follow-Up after Hospitalization for Mental Illness
Follow-Up After Emergency Department Visit for
Mental Illness
Follow-Up After Emergency Department Visit for
Alcohol and Other Drug Abuse or Dependence
Table 3: Dental (PAHP) and CSoC (PIHP) Performance Improvement Projects
2021-2023 Dental: Improving the
percentage of children with
their 10th birthdate in the
measurement year who
have ever received sealants
on permanent molar teeth:
at least one sealant
and
all four molars
sealed
Implement interventions to:
Improve member access to preventive dental
visits
Educate parents about the importance of dental
sealants to prevent cavities
Educate dental providers about evidence-based
clinical recommendations regarding sealants.

Louisiana Medicaid Managed Care Quality Strategy
9
2023 CSoC: Increase the
Effectiveness of Plans of
Care in Addressing
Actionable Clinical Needs
of Youth Enrolled in CSoC
CSoC enrollees are deemed at risk for or are currently in
out-of-home placement and often have cross-system
involvement (e.g., juvenile justice, child welfare, or
special education). Services are administered using the
Wraparound model, an intensive, structured, team-based
care coordination process that prioritizes the preferences
and perspectives of the youth and family throughout the
design and implementation of the plan of care (POC).
This project aims to improve the integration and
incorporation of clinical interventions and evidence-based
treatment (EBT) in addressing the actionable clinical
needs of youth enrolled in CSoC. This will be measured
through Plan of Care (POC) Reviews completed by the
CSoC Contractor’s Care Managers to monitor POC
submissions to assess adherence to practice standards and
verify that required program activities are completed.
Specifically, Care Managers will review members’ POCs
to determine the extent to which member needs are linked
to the assessment, evidence-based practices are considered
to address member needs where appropriate, and strategies
reflect member strengths and needs (and the effectiveness
of strategies).
2019-2022 CSoC: Monitoring
Hospitalization Follow Up
Practices
Implement the following interventions with the objective
to drive improvement in the rate of Coordinated System of
Care (CSoC) enrollee discharges from a mental health
hospitalization with appropriate follow up:
Utilize PST services of members to increase
engagement with families while the youth is
hospitalized with purpose of providing additional
support to family and educating family about the
importance of FUH process.
Expand the accessibility and availability of
Licensed Mental Health Professional (LMHP)
providers by increasing the reimbursement rates
to incentivize qualified providers to schedule
appointments within 7 days of discharge.
Magellan will conduct clinical rounds for youth
while hospitalized in order to identify risks, need
for specialized services, supports available to
family during times of crisis, exchange
information between the care and utilization
management teams and facilitate coordination of
care between the WAA and the inpatient provider.
Wraparound facilitators will conduct a crisis CFT
during the inpatient hospitalization or no later
than three business days from the date of the

Louisiana Medicaid Managed Care Quality Strategy
10
discharge with a goal of revising the Plan of Care
and crisis plan
2.3.1 PIP Topics and Processes
Each PIP must be completed in a reasonable time period so as to generally allow information on the
success of PIPs in the aggregate to produce new information regarding quality of care every year. Quality
improvement project topics should:
Include aims that are expressed as a Specific, Measureable, Actionable, Realistic, and Time-bound
(SMART)
Connect to the specific health outcomes prioritized in the LDH Quality Strategy
Use key driver diagrams (or other cause-and-effect diagrams) to show the theory of improvement or
how the interventions being tested are thought to impact the project goal (SMART aim)
Incorporate enrollee voice and concerns into topic choice and/or theory of improvement
Use clear descriptions of methods used to identify key drivers, associated interventions, and
prioritization of interventions (e.g., process mapping, Pareto analyses, root cause analyses, Failure
Mode & Effects Analysis, Gemba walk)
Reflect examples of intervention tests (PDSAs) and lessons learned
Use objective quality indicators to measure performance including: whether the measure is a process
measure, an outcome measure, or balancing measure, data source(s) for the measure, the intervention
or driver to which the measure is linked, the frequency of measurement, the frequency of review of
longitudinal (time series) measurement data, stratification of key data by race and other demographic
factors to assess for disparities, and, mention of methods used to draw conclusions from the data (e.g.,
identification of special cause or the degree of variance in processes)
Use longitudinal (trended) depictions (run charts, control charts, line graphs) of the MCO’s
improvement project outcomes over time with annotation of intervention periods and special cause
identification
Include results and lessons learned from performance and quality improvement projects and describe
how these are communicated within and across the organization, as well as integrated into the overall
MCO QAPI program
Define processes or procedures that have been or will be put in place to sustain and spread successful
interventions
LDH facilitates regular PIP meetings with MCOs to provide guidance and clinical leadership and allow
for MCO collaboration. The EQRO validates MCO PIPs and related performance measures each year and
produces a report, reviewed and approved by LDH prior to release to MCOs, which summarizes the PIP
results and findings for each MCO and recommendations for improvement.
2.4 Other Medicaid Quality Interventions
LDH has developed a series of interventions aligned closely with the Quality Strategy, designed to build
an innovative, whole-person centered, well-coordinated system of care that addresses both medical and
non-medical drivers of health. These interventions drive progress towards the Quality Strategy aims,
goals, and objectives described in Section 1, Introduction – Managed Care Goals, Objectives and
Overview. Progress against these aims, goals, and objectives, and the role of interventions in achieving
those goals, will be assessed using the measures defined in Appendix A of this document.

Louisiana Medicaid Managed Care Quality Strategy
11
2.4.1 MCO Withhold of Capitation Payments for Increasing Use of Value-Based
Payments (VBP) and Improving Health Outcomes
Effective February 2018, Medicaid introduced a two percent (2%) withhold requirement into its MCO
contracts to incentivize quality, health outcomes, and VBP. Effective January 2023, health equity was
introduced as a third component of the two percent (2%) withhold.
Half of the total withhold (i.e., 1%) is tied to the achievement of quality and health outcomes,
specifically on MCOs’ performance on the Medicaid managed care incentive-based quality
measures identified in Appendix A.
Half of the remaining total withhold amount (i.e., 0.5%) is linked to increasing the use of VBP.
The MCO’s VBP strategy must pertain to measurable outcomes that are meant to improve
quality, reduce costs, and increase patient satisfaction. The VBP strategy placed emphasis on the
establishment of provider payment arrangements designated as categories 3 and 4 and the
evolution of providers along the APM model continuum (i.e. from less sophisticated to more
advanced categories) with consideration of provider readiness to take on financial risk.
The remaining withhold (i.e., 0.5%) is linked to MCO reporting and performance relative to the
MCO’s health equity strategies, including health equity deliverables such as the MCO’s Health
Equity Plan.
2.4.2 Managed Care Incentive Payment (MCIP) Program
Effective January 2019, the MCIP program is designed to provide incentive payments to Medicaid MCOs
for achieving quality reforms that increase access to health care, improve the quality of care, and/or
enhance the health of MCO enrollees. Current quality reforms focus on increasing enrollees’ access to
primary health care, improving health outcomes for pregnant women, newborns, and enrollees with
chronic conditions, as well as reducing inefficiencies and costs by reducing unnecessary utilization,
promoting evidence-based practices, and reducing low-value care.
2.4.3 Health Information Technology (HIT)
LDH’s approach to the long-term sustainability of its current and future HIT and health information
exchange (HIE) statewide infrastructure began with the creation of its 2018 - 2021 Louisiana HIT
Roadmap. The Roadmap and concepts developed since it was published provide provides a foundational
framework to achieve ubiquitous, interoperable health care data sharing among participants throughout
the broader Louisiana health care community. LDH continues to support current opportunities and build
upon statewide initiatives with the collective purpose of improving the health of individuals, families and
communities. LDH is currently working on its’ future sustainability plan and reviewing several of the
initiatives outlined in the current Roadmap. These reviews will result in the updating of the Louisiana
Department of Health Roadmap with future state goals that will support sustainability of current projects
and statewide interoperability development.
2.4.4 Other LDH Department-Wide Quality Initiatives
Integral to this Quality Strategy and related aims, goals, and objectives are LDH-wide quality strategies
and initiatives supported by the Medicaid managed care program, such as:
Taking Aim at Cancer in Louisiana: a statewide initiative that brings together leaders across
sectors in healthcare, business, government, community, advocacy, philanthropy and other
sectors to work toward the common goal of improving cancer outcomes in Louisiana.
Louisiana Perinatal Quality Collaborative: a voluntary network of perinatal care providers,
public health professionals and patient and community advocates who work to advance equity

Louisiana Medicaid Managed Care Quality Strategy
12
and improve outcomes for parents, families, and newborns in Louisiana, supported by LDH and
authorized by the Louisiana Commission on Perinatal Care and Prevention of Infant Mortality.
Opioid Strategy: Through expanded federal grants from the Centers for Disease Control and
Prevention and the Substance Abuse and Mental Health Services Administration, LDH will
continue to work to expand access to opioid use disorder treatment in primary care settings.
Hepatitis C Elimination Strategy: LDH executed an innovative payment model for direct-acting
antivirals in Medicaid with the goal of eliminating hepatitis C virus infection in Louisiana.
2.5 Annual External Independent Reviews
The MCOs’ adherence to federal and state regulatory requirements and performance standards will be
evaluated annually, in accordance with 42 CFR 438.340, by an independent EQRO. This will include a
review of the services for timeliness, outcomes, and accessibility, using definitions contained in 42 CFR
438.320.
The scope of the annual EQR conducted by the state for MCOs, as outlined in 42 CFR 438.310(b),
includes: a) criteria used to select entities to perform the reviews, b) specification of activities to be
performed by the EQRO, c) the circumstances in which the EQR may use other accreditation review
results and d) standards for availability of review results. The annual EQR will be conducted each
calendar year, with the first EQR report including any months prior to the first full calendar year of
operation.
The activities to be performed by the EQRO broadly include: measurement of quality and appropriateness
of care and services; synthesis of results compared to the standards, and recommendations based on the
findings. The EQRO will meet these obligations by utilizing the EQR protocols developed by CMS to
perform the mandatory activities required of EQROs, as mentioned in 42 CFR 438.352 and 438.358,
including data to be gathered, data sources, activities to ensure accuracy, validity and reliability of data,
proposed data analysis and interpretation methods and documents and/or tools necessary to implement the
protocol.
The state ensures the EQRO has sufficient information for the review from the mandatory and optional
EQR-related activities described in the regulation, as outlined in 42 CFR 438.350. This information will
be obtained through methods consistent with established protocols, include the elements described in the
EQR results section, and results will be made available, as specified in the regulation.
Requirements of MCOs include the following:
The MCO shall provide all information requested by the EQRO and/or LDH including, but not
limited to, information concerning timeliness of, and enrollee access to, benefits and services.
The MCO shall cooperate with the EQRO during the review (including medical records review),
which will be done at least one (1) time per calendar year.
A description of the performance improvement goals, objectives, and activities developed and
implemented in response to the EQRO findings will be included in the MCO's QAPI program. LDH
may also require separate submission of an improvement plan specific to the findings of the EQRO.
If an MCO is deemed non-compliant during any aspect of the EQR process, a corrective action plan may
be developed to address areas of noncompliance, including a timeline for achieving compliance. LDH
provides ongoing monitoring of the corrective action plan.

Louisiana Medicaid Managed Care Quality Strategy
13
If the EQRO indicates that the quality of care is not within acceptable limits set forth in the Contract,
LDH may sanction the MCO in accordance with the provisions of the MCO contract and may suspend
automatic assignment until the MCO attains a satisfactory level of quality of care as determined by the
EQRO.
The EQRO produces, at least, the following information, as required in 42 CFR 438.364(a), without
disclosing the identity of any patient, as mentioned in 42 CFR 438.364(c):
A detailed technical report describing data aggregation and analysis and the conclusions
(including an assessment of strengths and weaknesses) that were drawn as to the quality,
timeliness, and access to care furnished by the MCO. For each activity conducted, the report does
include objectives, technical methods of data collection and analysis, description of data obtained
and conclusions drawn from the data;
Recommendations for improving the quality of health care services furnished by the MCO; and,
An assessment of the degree to which the MCO effectively addressed previous EQRO review
recommendations.
EQR results and technical reports are reviewed by LDH. Ongoing EQR status reports and final technical
and project reports are communicated through the Louisiana Medicaid Provider and Plan Resources,
Reporting and Accountability website (http://ldh.la.gov/index.cfm/page/1582). Report results, including
data and recommendations, are analyzed and used to identify opportunities for process and system
improvements in LDH and MCO quality management programs, improvements to PIPs and Medicaid
managed care quality performance measures, and determination of regulatory compliance of the MCOs.
LDH will provide copies of the EQRO results and reports, upon request, to interested parties through
print or electronic media or alternative formats for persons with sensory impairments, as mentioned in 42
CFR 438.364(c). LDH will also provide copies of the EQRO results and reports to CMS. In addition,
summary results and findings will be included in reports to the legislature and to the public, as
appropriate.
2.6 Procedures for Identifying, Evaluating, and Reducing Health
Disparities
2.6.1 Diversity and Inclusion
LDH characterizes diversity as representing the differences and similarities of all of us that include, for
example, individual characteristics (e.g., disability, age, education level, poverty status, rural/urban
setting, race, ethnicity, and sexual orientation), values, beliefs, experiences and backgrounds. LDH also
characterizes inclusion as creating a work environment in which all individuals are treated fairly and
respectfully, have equal access to opportunities and resources, and can contribute fully to the work of our
agency. This is inclusive of LDH also building its capacity to create, support and/or fund (i.e., via
programming projects and contracts) efforts that do not discriminate against people, populations, and/or
communities due to disability, age, education level, poverty status, rural/urban setting, race, ethnicity, and
sexual orientation. LDH believes that diversity and inclusion aid in more equitably achieving its mission
– “…protect and promote health and to ensure access to medical, preventive and rehabilitative services
for citizens of the State of Louisiana.”
2.6.2 Data Collection
In compliance with the requirements set forth in 42 CFR 438.340 (b)(6), and described in Section 2,
Driving Improvement and Monitoring Progress, MCOs must report select measures outlined in Appendix
A based on select strata such as age, race, ethnicity, sex, primary language, rural/urban status and

Louisiana Medicaid Managed Care Quality Strategy
14
disability status, where feasible. This information is provided to MCOs upon enrollee enrollment and will
be used by LDH to better understand disparities of care within and across MCOs.
The five racial categories for which data are gathered by the MCOs are: American Indian/Alaskan Native,
Asian, Native Hawaiian/Pacific Islander, Black/African American and White. The two ethnic categories
are: Hispanic or Latino and Non-Hispanic or Latino. When individuals do not self-identify their race and
ethnicity, alternative system checks and follow-up with households are performed. If a racial and/or
ethnic category cannot be obtained, the identification defaults to “Unknown.” Medicaid enrollees, who
are a member of any federally recognized American Indian or Alaskan Native tribe, may voluntarily elect
to enroll in the Medicaid managed care program.
During the Medicaid application process, the applicant may identify race, ethnicity, and primary spoken
language. The data collected for race and language is processed through the Louisiana Medicaid
Eligibility Determination System and downloaded nightly into the Medicaid Management Information
System (MMIS). The applicant’s preferred language is also identified and forwarded to the MMIS.
Because this is a voluntary disclosure, LDH relies on demographic updates to the eligibility system.
Although this method does not collect 100 percent of the required data, there are data for a significant
portion of Medicaid enrollees.
2.6.3 Communications with MCOs
LDH contracts with an Enrollment Broker that is responsible for Medicaid managed care program
enrollment and disenrollment. Daily, the Enrollment Broker provides updates on those newly enrolled
into the Medicaid managed care program. In addition, at specified times each month, the Enrollment
Broker notifies each MCO regarding those that will be enrolled, re-enrolled or disenrolled to/from their
MCO for the following month. The Enrollment Broker provides LDH a listing of current enrollees, via
electronic media, on a monthly basis. MCOs, or their administrators, must be capable of uniquely
identifying each enrollee across multiple systems within its span of control. To facilitate care delivery
appropriate to client needs, the enrollment file includes race/ethnicity, primary language spoken, and
selective health information. MCOs utilize this information to provide interpreter services and facilitate
enrollee needs in the context of their cultural and language requirements.
MCOs are required to ensure that translation services are provided for written marketing and enrollee
education materials for any language that is spoken as a primary language for 200 or more MCO enrollees
within the geographic service area. The state requires that MCOs and any contractors have interpretation
services for those who speak any language other than English. The Enrollment Broker will provide multi-
lingual interpreters and enrollment material in other alternate formats (large print, and/or Braille) as
needed.
2.6.4 Evaluating Health Disparities
LDH is committed to ensuring that improvements in health outcomes lead to equitable improvements in
all groups. As a first step, LDH is requiring routine reporting of quality measures stratified by
race/ethnicity as well as urban/rural status. LDH will support MCOs in including measures of health
disparities in all quality improvement activities. Based on their results over time, LDH will develop (or
require MCOs to develop) targeted interventions and/or other strategies to address identified disparities.
In addition, beginning in 2018, LDH’s EQRO conducts a Health Disparities Survey of each MCO and
includes the results in the Annual Technical Reports (ATR).

Louisiana Medicaid Managed Care Quality Strategy
15
In 2020, LDH formed a Medicaid Health Equity Action Team to review Medicaid policy, procedures and
processes to advance health equity initiatives and strategic goals.
Furthermore, LDH has strategies to address health disparities identified through data collection, data
stratification, and analysis. Strategies include, but are not limited to leveraging managed care contracts to
address disparities, health equity and SDOH; stratification of Medicaid performance measures; utilizing
performance improvement projects to create targeted interventions for subpopulations experiencing health
disparities; track and monitor improvements; publish quality measure data for public review; administer
health disparities surveys to the MCOs to identify gaps in care; stakeholder engagement and collaboration
with internal and external entities; and implementing the LDH Health Equity Framework.
2.7 Use of Sanctions
LDH may impose any or all sanctions, including requiring an MCO to take remedial action, imposing
intermediate sanctions, and/or assessing liquidated damages due to non-compliance with contract
requirements or applicable federal or state laws.
2.7.1 Acts or Failures to Act Subject to Intermediate Sanctions
Pursuant to 42 CFR §438.700, et seq., LDH may impose on the MCO intermediate sanctions if it
determines that an MCO acts or fails to act as follows:
Fails substantially to provide medically necessary services that the MCO is required to provide, under
law or under the Contract, to an enrollee covered under the Contract;
Imposes on enrollees premiums or charges that are in excess of the premiums or charges permitted
under the Louisiana Medicaid MCO Program;
Acts to discriminate among enrollees on the basis of their health status or need for health care
services; this includes termination of enrollment or refusal to reenroll an enrollee, except as permitted
in Contract Section 2.3.13.3, or any practice that would reasonably be expected to discourage
enrollment by recipients whose medical condition or history indicates probable need for substantial
medical services.
Misrepresents or falsifies information that it furnishes to CMS or to LDH;
Misrepresents or falsifies information that it furnishes to an enrollee, potential enrollee, or a health
care provider;
Fails to comply with the requirements for physician incentive plans, as set forth (for Medicare) in 42
CFR §422.208 and §422.210;
Distributes directly, or indirectly through any agent or independent contractor, marketing materials
that have not been approved by LDH or that contain false or materially misleading information; or
Violates any of the other applicable requirements of Section 1903(m), 1905(t)(3) or 1932 of the
Social Security Act and any implementing regulations.
2.7.2 Other Misconduct Subject to Intermediate Sanctions
LDH also may impose sanctions against any MCO if it finds any of the following non-exclusive
actions/occurrences:

Louisiana Medicaid Managed Care Quality Strategy
16
The MCO has failed to correct deficiencies in its delivery of service after having received written
notice of these deficiencies from LDH;
The MCO has been excluded from participation in Medicare because of fraudulent or abusive
practices pursuant to Public Law 95-142;
The MCO or any of its owners, officers or directors has been convicted of a criminal offense relating
to performance of the Contract with LDH or of fraudulent billing practices or of negligent practice
resulting in death or injury to the MCO’s enrollee;
The MCO has presented, or has caused to be presented, any false or fraudulent claim for services or
has submitted or has caused to be submitted false information to be furnished to the state or the
Secretary of the federal Department of Health and Human Services;
The MCO has engaged in a practice of charging and accepting payment (in whole or part) from
enrollees for services for which a PMPM payment was made by LDH;
The MCO has rebated or accepted a fee or portion of fee or charge for a patient referral;
The MCO has failed to repay or make arrangements for the repayment of identified overpayments or
otherwise erroneous payments;
The MCO has failed to keep or make available for inspection, audit or copying, such records
regarding payments claimed for providing services;
The MCO has failed to furnish any information requested by LDH regarding payments for providing
goods or services;
The MCO has made, or caused to be made, any false statement or representation of a material fact to
LDH or CMS in connection with the administration of the Contract;
The MCO has furnished goods or services to an enrollee which at the sole discretion of LDH, and
based on competent medical judgment and evaluation are determined to be 1) insufficient for his or
her needs, 2) harmful to the enrollee, or 3) of grossly inferior quality.
2.7.3 Sanction Types
The types of intermediate sanctions that LDH may impose on the MCO shall be in accordance with §1932
of the Social Security Act (42 U.S.C. §1396u-2) and 42 CFR §438.702-708 and may include any of the
following:
Civil monetary penalties in the amounts specified in 42 CFR §438.704
Appointment of temporary management for an MCO as provided in 42 CFR §438.706;
Granting enrollees the right to terminate enrollment without cause and notifying the affected
enrollees of their right to disenroll;
Suspension of all new enrollments, including automatic assignment, after the effective date of the
sanction;
Suspension of payment for enrollees enrolled after the effective date of the sanction and until
CMS or LDH is satisfied that the reason for imposition of the sanction no longer exists and is not
likely to recur in accordance with 42 CFR §438.730; and
Additional sanctions allowed under state statutes or regulations that address areas of
noncompliance described above.
Louisiana Medicaid Managed Care Quality Strategy
17
3 State Standards for Access and Clinical Policies and
Guidelines
3.1 Provider Network Adequacy Standards and Availability of
Services
Louisiana’s MCO contracts include robust requirements to ensure that MCOs meet federal and state
requirements and standards for adequate Medicaid enrollee access to covered services. All standards for
network adequacy and availability of services are in accordance with the access and network adequacy
standards set forth in the applicable federal regulations.
The following tables summarize provider network standards, as indicated in LDH’s Medicaid MCO
Contract Attachment F: Provider Network Standards, and other access performance standards.
Table 4: Provider Access and Distance Standards
Type
1
Network Ratio
2
(Provider:
Member)
Rural Parishes
3
(miles)
Urban Parishes
3
(miles)
Primary Care
4
Adult
5
PCP (Family/General
Practice; Internal Medicine;
FQHC; RHC)
6
1:1,000 30 10
Pediatric
5
PCP (Pediatrics;
Family/General Practice;
Internal Medicine; FQHC;
RHC)
6
1:1,000 30 10
Hospitals
Acute Inpatient Hospitals 30 10
Ancillary
Laboratory 30 20
Radiology 30 20
Pharmacy 30 10
Hemodialysis Centers 30 10
Specialty Care
OB/GYN
4
1:10,000 30 15
Allergy/Immunology 1:100,000 60 60
Cardiology 1:20,000 60 60
Dermatology 1:40,000 60 60
Endocrinology and Metabolism
7
1:25,000 60 60
Gastroenterology 1:30,000 60 60
Hematology/Oncology 1:80,000 60 60
Nephrology 1:50,000 60 60
Neurology
7
1:35,000 60 60
Ophthalmology 1:20,000 60 60
Orthopedics
7
1:15,000 60 60
Otorhinolaryngology/
Otolaryngology
1:30,000 60 60
Urology 1:30,000 60 60

Louisiana Medicaid Managed Care Quality Strategy
18
Type
1
Network Ratio
2
(Provider:
Member)
Rural Parishes
3
(miles)
Urban Parishes
3
(miles)
Other Specialty Care 60 60
Type
1
Rural
Parishes
3
(miles)
Urban Parishes
3
(miles)
Psychiatrists 30 15
Specialty Care
Physicians and LMHPs
who specialize in pregnancy-related
and postpartum depression or related mental health disorders
and pregnancy-related
60 60
Physicians and LMHPs who specialize in pregnancy-related
and postpartum substance use disorders
60 60
Other Specialty Care 60 60
Licensed Mental Health Specialists
7, 9
Advanced Practice Registered Nurse (Nurse Practitioners and
Clinical Nurse Specialists with a behavioral health specialty)
30 15
Medical or Licensed Psychologist 30 15
Licensed Clinical Social Worker 30 15
Psychiatric Residential Treatment Facilities (PRTFs) (pediatric
5
)
9
Psychiatric Residential Treatment Facility 200 200
Psychiatric Residential Treatment Facility Addiction (ASAM
Level 3.7)
200 200
Psychiatric Residential Treatment Facility Other
Specialization
200 200
Substance Abuse and Alcohol Abuse Center - Outpatient
ASAM Level 1 30 15
ASAM Level 2.1 30 15
ASAM Level 2WM 60 60
Substance Use Residential Treatment Facilities (adult
5
)
ASAM Levels 3.1 30 30
ASAM Levels 3.3 30 30
ASAM Levels 3.5 30 30
ASAM Levels 3.2 –Withdrawal Management 60 60
ASAM Level 3.7 60 60
ASAM Level 3.7-Withdrawal Management 60 60
Substance Use Residential Treatment Facilities (pediatric
5
)
ASAM Level 3.1 60 60
ASAM Level 3.2 Withdrawal Management 60 60
ASAM Level 3.5 60 60
Psychiatric Inpatient Hospital Services
9
Hospital, Free Standing Psychiatric Unit 75 60
Hospital, Distinct Part Psychiatric Unit 75 60
Behavioral Health Rehabilitation Services
9
Mental Health Rehabilitation Agency (Legacy MHR) 30 15

Louisiana Medicaid Managed Care Quality Strategy
19
Behavioral Health Rehab Provider Agency (Non-Legacy
MHR)
30 15
1
For the purposes of assessing Network Adequacy, the MCO shall consider only those
Providers who are actively providing services to enrollees, which shall be defined as (1)
physical health providers who have submitted at least twenty-five (25) claims in an office
setting within the prior six (6) calendar months; (2) behavioral health providers who have
submitted at least twenty-five (25) claims within the prior six (6) calendar months; or (3)
any providers who were newly contracted within the prior six (6) calendar months,
regardless of claim submissions.
2
The network ratio is a calculation of the MCO’s Network Providers relative to the MCO’s
members.
3
Unless otherwise specified in this Attachment, the Contractor must demonstrate that one
hundred percent (100%) of applicable members (adult or pediatric) have access to
Network Providers for the type of service specified within the identified distance standard
from the Enrollee’s residence, based on a driving route versus a straight line calculation.
4
For purposes of assessing Network Adequacy for OB/GYN specialty services, access
standards are established based on female members age 21 and over. The Contractor
shall not include OB/GYN providers in its assessment of Network Adequacy for Primary
Care Services.
5
For purposes of reporting Network Adequacy for both physical and behavioral health
services, adult is defined as an Enrollee age 21 and over and pediatric is defined as an
enrollee under age 21.
6
In order to be included in the calculation, the Provider must work as a PCP at least 24
hours per week. The MCO may use physician extenders to meet PCP network ratios and
distance standards. Physician extenders include nurse practitioners and physician
assistants linked to a physician group who provide Primary Care Services. For calculation
of the network ratio, each physician extender is counted with a factor of 0.5 while physician
PCPs are counted with a factor of 1.0.
7
For these specialties, the travel distance standards shall be applied separately to the
Contractor’s adult and pediatric member populations and to specialists serving the
applicable age group(s).
8
The linkage ratio is a calculation of the MCO’s network provider to his/her patients who are
Louisiana Medicaid managed care enrollees, regardless of MCO. The linkage ratios
specified are applicable to providers who work as PCPs at least 24 hours per week.
9
Network standards are applied across the provider types listed collectively within the
identified distance standard from the Enrollee’s residence, based on a driving route versus
a straight line calculation from the applicable members (adult or pediatric) residences.

Louisiana Medicaid Managed Care Quality Strategy
20
Table 5: Provider Access and Timeliness Standards
Type of Visit/Admission/Appointment Access/Timeliness Standard
Emergency care 24 hours, 7 days/week within 1 hour of request
Urgent non-emergency care 24 hours, 7 days/week within 24 hours of request,
Non-urgent sick primary care 72 hours
Non-urgent routine primary care 6 weeks
After hours, by phone
Answer by live person or call-back from a
designated medical practitioner within 30 minutes
Ob/Gyn care for pregnant women
1st Trimester 14 days
2nd Trimester 7 days
3rd Trimester 3 days
High risk pregnancy, any trimester 3 days
Family planning appointments 1 week
Specialist appointments 1 month
Scheduled appointments Less than a 45 minute wait in office
Non-urgent routine behavioral health care 14 days
Urgent non-emergency behavioral health care 24 hours
Psychiatric inpatient hospital (emergency
involuntary)
4 hours
Psychiatric inpatient hospital (involuntary) 24 hours
Psychiatric inpatient hospital (voluntary) 24 hours
ASAM Level 3.3, 3.5 & 3.7 10 business days
Residential withdrawal management 24 hours when medically necessary
Psychiatric Residential Treatment Facility
(PRTF)
20 calendar days
Table 6: Dental Access to Care and Network Availability Standards
Network Capacity and Geographic Access Standards
The Primary Dental Provider (PDP) may practice in a solo or group practice or may practice in a clinic
(i.e. Federally Qualified Health Center (FQHC), Rural Health Clinic (RHC) or outpatient clinic). The
Dental Benefit Program Manager (DBPM) shall contract with a sufficient number of PDPs needed to
meet the geographic access, appointment, and wait time standards outlined in this contract.
The DBPM shall provide access to dentists that offer extended office hours (before 8:00 a.m., after 4:30
p.m., and/or on Saturdays) at least one (1) day per week.
Network providers must offer office hours at least equal to those offered by commercial dental
insurance plans.
If an enrollee requests a provider who is located beyond access standards, and the DBPM has an
appropriate provider within the DBPM network who accepts new patients, it shall not be considered a
violation of the access requirements for the DBPM to grant the enrollee’s request. The DBPM shall not

Louisiana Medicaid Managed Care Quality Strategy
21
submit encounters for travel outside of the access standards if an appropriate provider was available
within the access standards.
The DBPM shall comply with the following maximum distance requirements, as determined by
mapping software (e.g. MapQuest, Google Maps, ArcGIS). Requests for exceptions as a result of
prevailing community standards must be submitted in writing to LDH for approval.
Distance to Primary Dental Services
Travel distance from enrollee’s place of residence shall not exceed thirty (30) miles one-way for rural
areas and ten (10) miles one way for urban areas.
Distance to Specialty Dental Services
Travel distance shall not exceed sixty (60) miles one-way from the enrollee’s place of residence for at
least seventy-five (75) percent of enrollees and shall not exceed ninety (90) miles one-way from the
enrollee’s place of residence for all enrollees.
The DBPM shall ensure, at a minimum, the availability of the following specialists and other
providers for enrollees under the age of twenty-one (21) years:
Endodontists;
Maxillofacial Surgeons;
Oral Surgeons;
Orthodontists;
Pedodontists;
Periodontists;
Prosthodontists; and
Special Needs Pedodontists.
Timely Access Standards
Urgent care services – within twenty-four (24) hours of a request for services that do not require prior
authorization and within forty-eight (48) hours for a request for services that do require prior
authorization;
Primary Dental Care – within thirty (30) days; and
Follow-up Dental Services – within thirty (30) days after assessment.
Table 7: Access Performance Standards
Access Performance Standards
Delivery Network
Contracted network of appropriate providers (42 CFR 438.206(b)(1))
Each MCO must meet the following requirements.
Maintains and monitor a network of appropriate providers that is supported by written agreements and is
sufficient to provide adequate access to all services covered under the contract. In establishing and
maintaining the network, each MCO must consider the anticipated Medicaid enrollment, the expected
utilization of services, and take into consideration the characteristics and health care needs of specific,
Medicaid populations enrolled. The MCO must also consider the numbers and types (in terms of
training, experience, and specialization) of providers required to furnish the contracted Medicaid
services, the number of network providers who are not accepting new Medicaid patients, and the
geographic location of providers and Medicaid enrollees. Distance, travel time, the means of
transportation ordinarily used by Medicaid enrollees, will be considered and whether the location
provides physical access for Medicaid enrollees with disabilities.

Louisiana Medicaid Managed Care Quality Strategy
22
Access Performance Standards
The MCO networks must be comprised of hospitals, physicians and specialists in sufficient numbers to
make available all covered services in a timely manner.
The primary care network of the MCO must have at least 1 full time equivalent PCP for every 2,500
patients. Physicians with physician extenders (nurse practitioner/physician assistant, certified nurse
midwife or OB/GYNs only) may increase the physician ration by 1,000 per extender. The maximum
number of extenders shall not exceed two extenders per physician.
The MCO shall ensure the availability of timely access to hospital care. Transport time will be usual and
customary, not to exceed 30 miles, except in rural areas where distance may be greater. If greater, the
standard shall be the community standard for accessing care. Exceptions must be justified, documented,
and submitted to LDH for approval. The MCO shall include, at a minimum, access to the following:
o One (1) hospital that provides emergency room services, inpatient, and outpatient care in each
parish in the state, provided the parish has such a hospital (free standing psychiatric hospitals
and distinct part psychiatric hospitals do not meet this requirement). The MCO must establish
access to the following within their network of hospitals:
Level III Obstetrical services;
Level III Neonatal Intensive Care (NICU) services;
Pediatric services;
Trauma services;
Burn services; and
A Children’s Hospital that meets the CMS definition in 42 C.F.R. §495.302 and
§412.23(d).
o Tertiary care is defined as health services provided by highly specialized providers, such as
medical sub-specialists; these services frequently require complex technological and support
facilities. The MCO shall provide tertiary care services including trauma centers, burn centers,
level III (high-risk) nurseries, rehabilitation facilities, and medical sub-specialists twenty-four
(24) hours per day. If the MCO does not have a full range of tertiary care services, the MCO
shall have a process for providing such services including transfer protocols and arrangements
with out-of-network providers.
Timely services for enrollees 438.3(q)(3)
Each MCO must provide for arrangements with, or referrals to, sufficient numbers of physicians and other
practitioners to ensure that services under the contract can be furnished to enrollees promptly and without
compromise to quality of care.
Direct Access to Women’s Health Specialist (42 CFR 438.206(b)(2)
Provides female enrollees with direct access to women’s health specialist within the network for covered
care, necessary to provide women’s routine and preventive health care services. This is in addition to the
enrollee’s designated source of primary care if that source is not a women’s health specialist.
Contractors must ensure that the network procedures for accessing family planning services are convenient
and easily comprehensible to enrollees.
A women's health specialist may serve as a primary care provider.
Adequate and Timely Second Opinion (42 CFR 438.206(b)(3))
Provides for a second opinion from a qualified health care professional within the network, or arranges for
the enrollee to obtain one outside the network, at no cost to the enrollee.
Adequate and Timely Out-of-Network Providers (42 CFR 438.206(b)(4) & (b)(5))
If the provider network is unable to provide necessary services, covered under the contract, to a particular
enrollee, the MCO must adequately and timely cover these services out of network for the enrollee, for as
long as the MCO provide
r
network is unable to provide them.

Louisiana Medicaid Managed Care Quality Strategy
23
Access Performance Standards
Requires out-of-network providers to coordinate with the MCO with respect to payment and ensures that
cost to the enrollee is no greater than it would be if the services were furnished within the network.
Provider Credentialing as required in regulation (42 CFR 438.206(b)(6))
Demonstrates that its providers are credentialed as required by § 438.214
Timely Access (42 CFR 438.206(c)(1)(i-vi))
Each MCO must meet and require its network providers to meet State standards for timely access to care
and services, taking into account the urgency of the need for services. Standards for access and timeliness
are identified in the Provider Network Companion Guide.
Ensure that the network providers offer hours of operation that are no less than the hours of operation offered
to commercial enrollees or comparable to Medicaid fee-for-service, if the provider serves only Medicaid
enrollees.
Make services included in the contract available 24 hours a day, 7 days a week, when medically necessary.
Establish mechanisms to ensure compliance by network providers, take corrective action if there is a failure
to comply.
Monitor network providers regularly to determine compliance
Take corrective action if there is a failure to comply by a network provider.
Reasonable and Adequate Hours of Operation 438.3(q)(1)
Each MCO must provide for reasonable and adequate hours of operation, including 24-hour availability of
information, referral, and treatment for emergency medical conditions.
Cultural Considerations (42 CFR 438.206(c)(2))
Each MCO participates in the state’s efforts to promote the delivery of services in a culturally competent
manner to all enrollees, including those with limited English proficiency and diverse cultural and ethnic
backgrounds.
o The MCO is required to have available interpretive services for all languages other than English upon
request.
o The MCO will encourage and foster cultural competency in its employees.
Assurances of Adequate Capacity 438.207
Documentation and Assurances of Adequate Capacity and Services (42 CFR 438.207 (b), (c))
Each MCO must give assurances to the state and provide supporting documentation that demonstrates that it
has the capacity to serve the expected enrollment in its service area and in accordance with the State’s
standards for access to care including § 438.68 and § 438.206(c)(1)
o Nature of supporting documentation: Each MCO must submit documentation to the state, in a format
specified by the state to demonstrate that it complies with the requirements below.
o Offers an appropriate range of preventive, primary care, and specialty services that are adequate for
the anticipated number of enrollees for the service area.
o Maintains a network of providers that is sufficient in number, mix, and geographic distribution to
meet the needs of the anticipated number of enrollees in the service area.
o Timing of documentation: Each MCO must submit the required documentation, no less frequently than:
o at the time it enters into a contract with the state or at any time there has been a significant change
(as defined by the state) in the MCO operations that would affect adequate capacity and services,
including changes in Contractor services, benefits, geographic service area, payments or enrollment
of a new population with the MCO.
Coordination and Continuity of Care 438.208

Louisiana Medicaid Managed Care Quality Strategy
24
Access Performance Standards
Except as specified below, the State must ensure that through its contracts, each MCO complies with the
requirements of this section.
Exception for MCOs that serve dually eligible enrollees.
o For a MCO that serves enrollees who are also enrolled in and receive Medicare benefits from a
Medicare+Choice plan, the state determines to what extent that a MCO must meet the primary care
coordination, identification, assessment, and treatment planning provisions of this section.
o The state bases its determination on the services it requires the MCO to furnish to dually eligible
enrollees.
Primary care and coordination of health care services for all MCO enrollees.
Each MCO must implement procedures to deliver primary care to and coordinate health care services for all
MCO enrollees. These procedures must meet state requirements and must do the following:
Ensure that each enrollee has an ongoing source of primary care appropriate to his or her needs and a person
or entity designated as primarily responsible for coordinating the health care services furnished to the
enrollee.
Coordinate the services the MCO furnishes to the enrollee with the services the enrollee receives from any
other MCO, PIHP, or PAHP, with services the enrollee receives in FFS; and with the services the enrollee
receives from community and social support providers.
Provide that the MCO makes a best effort to conduct an initial screening of each enrollee’s needs, within 90
days of the effective date of enrollment for all new enrollees, including subsequent attempts if the initial
attempt to contact the enrollee is unsuccessful.
Share with the State or other MCOs serving the enrollee the results of any identification and assessment of
that enrollee’s needs to prevent duplication of those activities.
Ensure that in the process of coordinating care, each enrollee’s privacy is protected in accordance with the
privacy requirements in 45 CFR parts 160 and 164 subparts A and E, to the extent that they are applicable.
MCO contract §6.39 (Case Management)
The MCO shall maintain a case management program through a process which provides appropriate and
medically-related services, social services, and basic and specialized behavioral health services that are
identified, planned, obtained and monitored for identified members who are in the special healthcare needs
(SHCN) population and identified members who have high risk or have unique, chronic, or complex needs.
The process shall integrate the member’s and case manager’s review of the member's strengths and needs
resulting in a mutually agreed upon appropriate plan that meets the medical, functional, social and
behavioral health needs of the member.
Identification and Assessment (42 CFR 438.208(c)(1)(2))
Identification. The State must implement mechanisms to identify persons who need LTSS or persons with
SHCN needs to MCO, as those persons are defined by the State. These identification mechanisms:
o Must be specified in the State’s quality strategy in § 438.340;
and
o May use State staff, the State’s enrollment broker, or the State’s MCOs.
Assessment: Each MCO must implement mechanisms to comprehensively assess each Medicaid enrollee
identified by the State (through the mechanism specified in paragraph (c)(1) of this section) and identified to
the MCO by the State as LTSS or SHCN in order to identify any ongoing special conditions of the enrollee
that require a course of treatment or regular care monitoring. The assessment mechanisms must use
appropriate providers or individuals meeting LTSS service coordination requirements of the State or the
MCO as appropriate.
Mechanisms for Enrollees with SHCN or who need LTSS (42 CFR 438.208(c)(3))
Treatment/service plans: MCOs must produce a treatment or service plan meeting the criteria in
paragraphs (c)(3)(i) through (v) of this section for enrollees who require LTSS and, if the State requires,

Louisiana Medicaid Managed Care Quality Strategy
25
Access Performance Standards
must produce a treatment or service plan meeting the criteria in paragraphs (c)(3)(iii) through (v) of this
section for enrollees with special health care needs that are determined through assessment to need a
course of treatment or regular care monitoring. The treatment or service plan must be:
o Developed by an individual meeting LTSS service coordination requirements with enrollee
participation, and in consultation with any providers caring for the enrollee;
o (ii) Developed by a person trained in person-centered planning using a person-centered process
and plan as defined in § 441.301(c)(1) and (2) of this chapter for LTSS treatment or service
plans;
o (iii) Approved by the MCO, PIHP, or PAHP in a timely manner, if this approval is required by
the MCO, PIHP, or PAHP;
o (iv) In accordance with any applicable State quality assurance and utilization review standards;
and
o (v) Reviewed and revised upon reassessment of functional need, at least every 12 months, or
when the enrollee's circumstances or needs change significantly, or at the request of the enrollee
per § 441.301(c)(3) of this chapter.
o .
Mechanisms for Enrollees with SHCN: Direct Access to Specialists (42 CFR 438.208(c)(4))
Direct access to specialists: For enrollees with SHCN determined through an assessment (consistent with §
438.208(c)(2)), to need a course of treatment or regular care monitoring, each MCO must have a mechanism
in place to allow enrollees to directly access a specialist (for example, through a standing referral or an
approved number of visits) as appropriate for the enrollee’s condition and identified needs.
Coverage and Authorization of Services §438.210
The State must ensure through its contracts with each MCO complies with the requirements of this section.
o Identify, define, and specify the amount, duration, and scope of each service that the MCO, PIHP, or
PAHP is required to offer.
o Require that the services identified in paragraph §438.210 (a)(1) of this section be furnished in an
amount, duration, and scope that is no less than the amount, duration, and scope for the same
services furnished to beneficiaries under FFS Medicaid, as set forth in § 440.230 and for enrollees
under the age of 21, as set forth in subpart B of part 441.
Provide that the MCO:
o Must ensure that the services are sufficient in amount, duration, or scope to reasonably achieve the
purpose for which the services are furnished.
o May not arbitrarily deny or reduce the amount, duration, or scope of a required service solely
because of diagnosis, type of illness, or condition of the beneficiary.
The MCO may place appropriate limits on a service based criteria applied under the State plan, such as
medical necessity or for the purpose of utilization control, provided the services furnished can reasonably be
expected to achieve their purpose. The MCO must also specify what constitutes “medically necessary
services” in a manner that:
o is no more restrictive than that used in the State Medicaid program as indicated in State statutes and
regulations, the State plan, and other state policy and procedures manuals; and
o addresses the extent to which the MCO is responsible for covering services related to the following:
The prevention, diagnosis, and treatment of enrollee’s disease, condition and/or disorder that results
in health impairments and/or disability;

Louisiana Medicaid Managed Care Quality Strategy
26
Access Performance Standards
The ability to achieve age-appropriate growth and development
The ability to attain, maintain, or regain functional capacity and
The opportunity for an enrollee receiving long-term services and supports to have access to the
benefits of community living, to achieve person-centered goals, and live and work in the setting of
their choice.
Policies and Procedures for Authorization of Services (42 CFR 438.210(b)(1), (2), and (3))
For the processing of requests for initial and continuing authorizations of services, each contract must
require:
o That the MCO and its subcontractors have in place, and follow, written policies and procedures.
o That the MCO
Have in effect mechanisms to ensure consistent application of review criteria for authorization
decisions; and
Consult with the requesting provider when appropriate.
Authorize LTSS based on an enrollee’s current needs assessment and consistent with the person-
centered service plan.
That any decision to deny a service authorization request or to authorize a service in an amount,
duration, or scope that is less than requested, be made by an individual who has appropriate
expertise in addressing the enrollee's medical, behavioral health, or long-term services and supports
needs.
Notice of Adverse Action (42 CFR 438.210(c))
Each contract must provide for the MCO to notify the requesting provider, and give the enrollee written
notice of any decision by the MCO to deny a service authorization request, or to authorize a service in
an amount, duration, or scope that is less than requested. The notice must meet the requirements of
§438.404, except that the notice to the provider need not be in writing. For Medicaid contracts with an
applicable integrated plan, as defined in § 422.561, in lieu of the provisions in this paragraph governing
notices of adverse benefit determinations, the provisions set forth in §§ 422.629 through 422.634 apply
to determinations affecting dually eligible individuals who are also enrolled in a dual eligible special
needs plan with exclusively aligned enrollment, as defined in § 422.2
Timeframe for decisions (42 CFR 438.210(d))(1), (2)&(e)
Each MCO contract must provide for the following decisions and notices:
o Standard authorization decisions: For standard authorization decisions, provide notice as expeditiously
as the enrollee’s health condition requires and within State-established timeframes that may not exceed
14 calendar days, following receipt of the request for service, with a possible extension of up to 14
additional calendar days, if:
The enrollee, or the provider, requests extension: or
The MCO justifies (to the state agency upon request) a need for additional information and the
extent to which the extension is in the enrollee’s interest.
o Expedited authorization decisions: For cases in which a provider indicates, or the MCO determines,
that following the standard timeframe could seriously jeopardize the enrollee’s life or health or ability to
attain, maintain, or regain maximum function, the MCO must make an expedited authorization decision
and provide notice as expeditiously as the enrollee’s health condition requires and no later than 3
working days after receipt of the request for service.

Louisiana Medicaid Managed Care Quality Strategy
27
Access Performance Standards
o The MCO may extend the 72-hour time period by up to 14 calendar days if the enrollee requests an
extension, or if the MCO justifies (to the State agency upon request) a need for additional information
and how the extension is in the enrollee’s interest.
Compensation for utilization management activities: Each contract between the State and MCO must
provide that, consistent with §§438.3(i)), and §422.208 of this chapter, compensation to individuals or
entities that conduct utilization management activities is not structured so as to provide incentives for the
individual or entity to deny, limit, or discontinue medically necessary services to any enrollee.
Emergency and Post–Stabilization Care Service (42 CFR 438.114)
The MCOs will comply with the definitions used in this section:
Emergency medical condition means a medical condition manifesting itself by acute symptoms of sufficient
severity (including severe pain) such that a prudent layperson, who possesses an average knowledge of
health and medicine, could reasonably expect the absence of immediate medical attention to result in the
following:
o Placing the health of the individual (or for pregnant woman, the health of the woman or her unborn
child) in serious jeopardy;
o Serious impairment to bodily functions; or
o Serious dysfunction of any bodily organ or part.
Emergency services means covered inpatient and outpatient services that are:
o Furnished by a provider that is qualified to furnish emergency services.
o Needed to evaluate or stabilize an emergency medical condition.
Post-stabilization care services means covered services, related to an emergency medical condition, that are
provided after an enrollee is stabilized in order to maintain the stabilized condition, or, under the
circumstances described in paragraph (e) of this section, to improve or resolve the enrollee’s condition.
Coverage and payment: MCOs are responsible for coverage and payment of emergency services and post-
stabilization care services.
Coverage and payment: Emergency services.
(1) The entities identified in this section -
Must cover and pay for emergency services regardless of whether the provider that furnishes the
services has a contract with the MCO; and
May not deny payment for treatment obtained under either of the following circumstances:
o An enrollee had an emergency medical condition, including cases in which the absence of
immediate medical attention would not have had the outcomes specified in paragraphs (1), (2),
and (3) of the definition of emergency medical condition in this section.
o A representative of the MCO instructs the enrollee to seek emergency services.
Additional rules for emergency services.
(1) The MCOs may not -
Limit what constitutes an emergency medical condition on the basis of lists of diagnoses or symptoms;
and
Refuse to cover emergency services based on the emergency room provider, hospital, or fiscal agent not
notifying the enrollee's primary care provider, MCO or applicable State entity of the enrollee's screening
and treatment within 10 calendar days of presentation for emerg
ency services.
(2) An enrollee who has an emergency medical condition may not be held liable for payment of subsequent
screening and treatment needed to diagnose the specific condition or stabilize the patient.

Louisiana Medicaid Managed Care Quality Strategy
28
Access Performance Standards
(3) The attending emergency physician, or the provider actually treating the enrollee, is responsible for
determining when the enrollee is sufficiently stabilized for transfer or discharge, and that determination is
binding on the entities identified in paragraph (b) of this section as responsible for coverage and payment.
Coverage and payment: Post-stabilization care services. Post-stabilization care services are covered and paid
for in accordance with provisions set forth in 42 CFR §422.113(c). In applying those provisions, reference to
“MA organization” and “financially responsible” must be read as reference to the entities responsible for
Medicaid payment, as specified in paragraph (b) of this section, and payment rules governed by Title XIX of the
Act and the States.
(2) MA organization financial responsibility. The MA organization -
Is financially responsible (consistent with § 422.214) for post-stabilization care services obtained within
or outside the MA organization that are pre-approved by a plan provider or other MA organization
representative;
Is financially responsible for post-stabilization care services obtained within or outside the MA
organization that are not pre-approved by a plan provider or other MA organization representative, but
administered to maintain the enrollee's stabilized condition within 1 hour of a request to the MA
organization for pre-approval of further post-stabilization care services;
Is financially responsible for post-stabilization care services obtained within or outside the MA
organization that are not pre-approved by a plan provider or other MA organization representative, but
administered to maintain, improve, or resolve the enrollee's stabilized condition if –
o The MA organization does not respond to a request for pre-approval within 1 hour;
o The MA organization cannot be contacted; or
o The MA organization representative and the treating physician cannot reach an agreement
concerning the enrollee's care and a plan physician is not available for consultation. In this
situation, the MA organization must give the treating physician the opportunity to consult with a
plan physician and the treating physician may continue with care of the patient until a plan
physician is reached or one of the criteria in § 422.113(c)(3) is met; and
Must limit charges to enrollees for post-stabilization care services to an amount no greater than what the
organization would charge the enrollee if he or she had obtained the services through the MA
organization. For purposes of cost sharing, post-stabilization care services begin upon inpatient
admission.
(3) End of MA organization's financial responsibility. The MA organization's financial responsibility for post-
stabilization care services it has not pre-approved ends when -
A plan physician with privileges at the treating hospital assumes responsibility for the enrollee's care;
A plan physician assumes responsibility for the enrollee's care through transfer;
An MA organization representative and the treating physician reach an agreement concerning the
enrollee's care; or
The enrollee is discharged.
Applicability to PIHPs and PAHPs. To the extent that services required to treat an emergency medical condition
fall within the scope of the services for which the PIHP or PAHP is responsible, the rules under this section
apply.

Louisiana Medicaid Managed Care Quality Strategy
29
3.2 Adoption & Dissemination of Evidence-Based Clinical Practice
Guidelines
The application of evidence-based clinical practice guidelines has proven to reduce variation in treatment,
resulting in improved quality. The MCO’s development and use of evidence-based clinical practice
guidelines for physical and behavioral health is expected and must be consistent with the requirements of
42 CFR 438.236:
Are based on valid and reliable clinical evidence or a consensus of providers in the particular
field;
Consider the needs of enrollees;
Are adopted in consultation with; and
Are reviewed and updated periodically as appropriate.
LDH expects MCOs to coordinate the development of clinical practice guidelines with other MCOs and
Louisiana Medicaid clinical leadership team through the process established to create provider manual
updates, to avoid providers receiving conflicting practice guidelines.
MCOs must use clinical care standards and/or practice guidelines to objectively evaluate the care the
MCO delivers or fails to deliver for targeted clinical conditions. These guidelines and/or clinical care
standards must be formally adopted by the MCO’s Quality Assessment and Performance Improvement
(QAPI) Committee and disseminated to all affected providers and, upon request, to enrollees and potential
enrollees. Decisions for utilization management, enrollee education, coverage of services, and other areas
to which the guidelines apply must be consistent with the guidelines. MCOs must monitor adherence to
practice guidelines by medical record reviews and performance measure outcomes.
Examples of evidence-based practices guidelines plans are required to use are in the following categories:
Federal guidelines (e.g., Agency for Healthcare Research and Quality evidence reviews and
United States Preventive Service Taskforce recommendations)
Specialty society guidelines (e.g., the Infectious Diseases Society of America/American
Association for the Study of Liver Diseases Hepatitis C treatment guidelines)
Other clinical practice guidelines produced by other organizations (e.g., Milliman Care
Guidelines)
3.3 Transition of Care Policy
LDH monitors the development and maintenance of effective continuity of care activities to ensure a
continuum of care approach to enrollees. MCOs are required to provide service authorization, referrals,
coordination, and/or assistance in scheduling the covered services consistent with standards as defined in
the Louisiana Medicaid State Plan and as specified in the terms of the MCO contract.
The MCO shall provide active assistance to enrollees when transitioning to another MCO or to Medicaid
FFS. A receiving MCO is responsible for the provision of medically necessary services during the
transition period that shall not exceed thirty (30) calendar days from the effective date of the enrollee’s
enrollment in the receiving MCO unless the enrollee has been identified as an individual with special
health care needs. The MCO shall provide continuation/coordination of services for enrollees identified as
having special health care needs up to ninety (90) calendar days or until the enrollee may be reasonably
transferred without disruption, whichever is less. During the transition period, the receiving MCO shall be

Louisiana Medicaid Managed Care Quality Strategy
30
responsible for notification to the new primary care provider of the enrollee’s selection, initiation of the
request of transfer for the enrollee’s medical files, and arrangement of medically necessary services.
If an enrollee is to be transferred between MCOs but is hospitalized at the time, the transfer shall be
effective for the date of enrollment into the receiving MCO; however, the relinquishing MCO is
responsible for the enrollee’s hospitalization until the enrollee is discharged. The receiving MCO is
responsible for all other care.
The MCO shall not require service authorization for the continuation of medically necessary covered
services of a new enrollee transitioning into the MCO, regardless of whether such services are provided
by an in-network or out-of-network provider; however, the MCO may require prior authorization of
services beyond thirty (30) calendar days. For the first thirty (30) calendar days of enrollment, the MCO
is prohibited from denying prior authorization solely on the basis of the provider being an out-of-network
provider.
3.4 Mechanisms Used to Identify Persons with Special Health Care
Needs (SHCN)
An enrollee with SHCN is an individual of any age with a mental disability, physical disability, or other
circumstance that places his or her health and ability to fully function in society at risk, and thus requires
individualized health care requirements. Identification mechanisms should include:
The MCO’s use of historical claims data (if available) to identify enrollees who meet Medicaid
managed care program eligibility criteria for SHCN. Enrollees with Special Health Care Needs is
defined as individuals of any age with a behavioral health disability, physical disability,
developmental disability, or other circumstances that place their health and ability to fully
function in society at risk, requiring individualized care approaches. Enrollees with Special
Health Care Needs shall include any enrollees who:
o have complex needs such as multiple chronic conditions, co-morbidities, and co-existing
functional impairments;
o are at high risk for admission/readmission to a hospital within the next six (6) months;
o are at high risk of institutionalization;
o have been diagnosed with a Serious Emotional Disturbance, a Severe and Persistent
Mental Illness, or a Substance Use Disorder, or otherwise have significant behavioral
health needs;
o are homeless as defined in Section 330(h)(5)(A) of the Public Health Services Act and
codified by the US Department of Health and Human Services in 42 U.S.C. 254(b);
o are women with high-risk pregnancies (i.e., pregnancies that have one or more risk
factors) or who have had an adverse pregnancy outcome during the pregnancy, including
preterm birth of less than thirty-seven (37) weeks;
o have been recently incarcerated and are transitioning out of custody;
o are at high risk of inpatient admission or Emergency Department visits, including certain
enrollees transitioning care across acute hospital, chronic disease and rehabilitation
hospital or nursing facility setting;
o are members of the Department of Justice (DOJ) Agreement Target Population;
o are enrolled under the Act 421 Children’s Medicaid Option; or
o receive care from other state agency programs, including but not limited to programs
through Office of Juvenile Justice (OJJ), Department of Children and Family Services
(DCFS), or Office of Public Health (OPH).

Louisiana Medicaid Managed Care Quality Strategy
31
The MCO must identify enrollees with SHCN within 90 days of receiving the enrollee’s historical
claims data.
Primary care physicians can identify enrollees with SHCN at any time. An appropriate healthcare
professional must conduct an assessment of those enrollees within 90 days of identification. If an
assessment determines a course of treatment or regular care monitoring, referral for case
management will be provided.
Enrollees may also self-identify as SHCN to either the Enrollment Broker or the MCO.
MCOs monitor and assess the appropriateness of care furnished to individuals with SHCN
through various means including but not limited to evaluation of the quality assessment and
performance improvement programs, comprehensive care management program reporting, care
coordination, and use of the CAHPS Children with Chronic Conditions survey
Louisiana implemented Act 421 enacted by the Louisiana Legislature effective January, 1, 2022.
The program is titled the Act 421 Children’s Medicaid Option (“Act 421-CMO”). The Act 421-
CMO extends Medicaid eligibility to children covered by § 1902(e)(3) of the Social Security Act,
i.e., children age 18 and younger who meet institutional level of care (Nursing Facility, Hospital,
Intermediate Care Facility for Individuals with Intellectual/Developmental Disabilities) and are in
families with income that is too high to qualify for Medicaid, who could otherwise become
Medicaid eligible if receiving extended care in an institutional setting.
o The Demonstration option allows these children with disabilities to become Medicaid
eligible based on their own resources in order to receive medical services in less-costly
home-settings instead of an institution.
o The 1115 demonstration waiver authority is to be used to provide coverage to eligible
children but with a condition of coverage that families maintain pre-existing private
major medical health insurance (obtained through employment or the private insurance
market) unless the family demonstrates that maintaining private insurance would create a
financial hardship for the family and meets good cause exception criteria.
o The enrollment cap for 421-CMO is the number of children who can be served based on
annual legislative appropriation. With the exception of children with dual coverage in
Medicare and Medicaid, enrollment in managed care is required of all participants in
order to control costs and enhance budget predictability.
3.5 Non-Duplication Strategy
The CMS External Quality Review (EQR) regulations (42 CFR 438.360) allow for non-duplication of
mandatory EQR activities at the state’s discretion. These regulations permit use of information about an
MCO obtained from a private accreditation review to be used in the annual EQR if certain conditions are
met. These conditions include, but are not limited to, compliance with the standards established by a
national accrediting organization when the organization’s standards are comparable to the federal
standards. For MCOs achieving accreditation, the LDH External Quality Review Organization (EQRO)
can use the toolkits produced by the accrediting organizations and the MCO-specific accreditation
reports/results to identify standards meeting federal and state regulatory requirements. The EQRO can
then use the accrediting organization’s results for those standards.
Beginning with the 2020-2021 EQR reports published in 2022, the Information Systems Capabilities
Assessment (ISCA) mandatory EQR activity is substituted by the system reviews conducted as part of the
MCO’s NCQA HEDIS Compliance Audit, as outlined by CMS. Should the state determine in the future

Louisiana Medicaid Managed Care Quality Strategy
32
that a private accreditation activity (e.g., National Committee on Quality Assurance [NCQA]
accreditation) is comparable to any other EQR activities, the state will work with the EQRO to identify
any areas in the NCQA accreditation program that may be redundant with the EQR review and deem
these activities accordingly.

Louisiana Medicaid Managed Care Quality Strategy
33
4 EVALUATING, UPDATING, AND DISSEMINATING
THE QUALITY STRATEGY
4.1 Quality Strategy Development and Public Comment
The Quality Strategy reflects significant stakeholder input as well as thoughtful consideration of the
quality priorities and issues that are most important in Louisiana. Through multiple, ongoing public
stakeholder forums across the state and engagement with the Medical Care Advisory Committee, LDH
specifies a set of measures that represent critical targets to improve the quality of care and health
outcomes for Medicaid enrollees.
In 2017, in preparation for Louisiana’s transition to its VBP program, Medicaid conducted “A Deep Dive
into Quality” through a series of public town hall meetings across the state. Led by Medicaid’s Chief
Medical Officer and Chief Transformation Officer for Quality Improvement, LDH traveled to seven
regions of the state to gain stakeholder input on quality measurement priorities that best reflect the needs
and desired health outcomes of Medicaid enrollees. The results of this effort culminated in the prioritized
set of MCO incentivized and monitored quality performance measures referenced in Section 2, Driving
Improvement and Monitoring Progress, as ratified by the Medical Care Advisory Committee.
Later, in 2018, Medicaid conducted another series of public stakeholder events titled, “Paving the Way to
a Healthier Louisiana: Advancing Medicaid Managed care,” to communicate its future vision for the
Medicaid managed care program and gain stakeholder input on key managed care policies. These events
laid the foundation for managed care policy priorities, including the Quality Strategy Aims, Goals and
Objectives, as described in Section 1, Managed Care Goals, Objectives and Overview.
In preparation for the future Medicaid managed care program effective 2021, LDH updated its MCO
quality performance measures (currently referenced in Section 2, Driving Improvement and Monitoring
Progress) to best align with the priorities and objectives of the Louisiana Managed Care Quality Strategy
and other LDH Department-wide priorities. LDH undertook a broad public stakeholder input process
across major regions of the state in early 2019. As part of this effort, LDH worked in concert with the
Medical Care Advisory Committee to reach consensus on the final set of performance measures.
In accordance with the state’s Tribal consultation policy, tribal notification was also made to request
further input into the Quality Strategy. In parallel, prior to finalizing the Quality Strategy, LDH made the
Quality Strategy available for public comment and incorporated edits as appropriate. LDH made the final
Quality Strategy available on its website.
4.2 Quality Strategy Review, Update, and Evaluation
The Quality Strategy will be reviewed and updated as needed, but no less than once every three years as
required by the CMS Medicaid Managed Care Final Rule or when there is a significant change, defined as
any change to the Quality Strategy that may reasonably be foreseen to materially affect the delivery or
measurement of the quality of health care services. The Quality Strategy review includes an evaluation of
the effectiveness of the quality strategy. Currently, the state’s EQRO conducts an in-depth, independent
evaluation and produces an annual report on the implementation and effectiveness of the Quality Strategy.
This evaluation can include feedback from both internal and external stakeholders. The Quality Strategy
Evaluation report is published on LDH’s website.

Louisiana Medicaid Managed Care Quality Strategy
34
MCO quality performance measure results, stakeholder input on current issues and barriers to health care
access and quality, and LDH strategic priorities all inform decisions regarding quality goals and
measures. Measures are assessed to determine what, if any, updates should be made, including the
addition and removal of measures and the selection of incentive-based measures. Criteria used to make
decisions regarding measure recommendations includes:
Relevance: Measures must be relevant to Medicaid enrollees
Scientific Soundness: Measures must be based on evidence produced through research and
evaluation, ideally at the national level
Feasibility: Measures initially must meet at least one of three requirements:
o Be retrievable through routinely collected administrative data
o Be collected via survey of enrollees or their caretakers
o Be collected via a medical record review
Additional considerations for decisions regarding quality measures and initiatives include technical
aspects, such as whether:
The measure has been in operation for a sufficient period of time to demonstrate effectiveness
The measure has demonstrated success documented through tangible results
The measure is consistent with current policy and evidence-based practice

Louisiana Medicaid Managed Care Quality Strategy
35
APPENDIX A: Louisiana Medicaid MCO Performance Measures (Measurement Year 2023 and Subsequent Years)
Aims Goals Objectives $$ Measures Measure Description Steward
Better Care.
Make health
care more
person-
centered,
coordinated,
and accessible
so that
enrollees get
the right care
at the right
time in the
right place.
Ensure access
to care to
meet enrollee
needs
Ensure timely
and approximate
access to primary
and specialty
care
1. Child and Adolescent Well-Care Visits
The percentage of members 3–21 years of age who had at least one
comprehensive well-care visit with a PCP or an OB/GYN practitioner
during the measurement year.
NCQA
2. Well-Child Visits in the First 30 Months of Life
The percentage of members who had the following number of well-
child visits with a PCP during the last 15 months. The following rates
are reported:
1. Well-Child Visits in the First 15 Months. Children who turned 15
months old during the measurement year: Six or more well-child
visits.
2. Well-Child Visits for Age 15 Months–30 Months. Children who
turned 30 months old during the measurement year: Two or more
well-child visits.
3. Inpatient Utilization – General Hospital/Acute Care
(IPU)
This measure summarizes utilization of acute inpatient care and
services in the following categories:
Maternity
Surgery
Medicine
Total inpatient (the sum of Maternity, Surgery and Medicine)
4. Adult Access to Preventive/Ambulatory Services
The percentage of members age 20 years and older who had an
ambulatory or preventive care visit during the measurement year.
Three age stratifications and a total rate are reported:
20-44 years
45-64 years
65 years and older
Total
Improve
coordination
and
transitions of
care
Ensure
appropriate
follow-up after
emergency
department visits
and
hospitalizations
through effective
care coordination
and case
management
5. Ambulatory Care
This measure summarizes utilization of ambulatory care in the
following categories:
Outpatient Visits Including Telehealth
ED Visits
Note: A lower rate indicates better performance for ED visits.
NCQA
$$
6. Follow-Up After Hospitalization for Mental Illness
The percentage of discharges for members 6 years of age and older
who were hospitalized for treatment of selected mental illness or
intentional self-harm diagnoses and who had a follow-up visit with a
mental health practitioner. Two rates are reported:
$$: The percentage of discharges for which the member received
follow-up within 30 days after discharge.
The percentage of discharges for which the member received
follow-up within 7 days after discharge.

Louisiana Medicaid Managed Care Quality Strategy
36
Aims Goals Objectives $$ Measures Measure Description Steward
$$
7. Follow-Up After Emergency Department Visit for
Mental Illness
The percentage of emergency department (ED) visits for members 6
years of age and older with a diagnosis of mental illness or intentional
self-harm, who had a follow-up visit for mental illness. Two rates are
reported:
$$: The percentage of ED visits for which the member received
follow-up within 30 days of the ED visit (31 total days).
The percentage of ED visits for which the member received
follow-up within 7 days of the ED visit (8 total days).
$$
8. Follow-Up After Emergency Department Visit for
Substance Use
The percentage of emergency department (ED) visits among members
age 13 years and older with a principal diagnosis of substance use
disorder (SUD), or any diagnosis of drug overdose, for which there was
follow-up. Two rates are reported:
The percentage of ED visits for which the member received
follow-up within 30 days of the ED visit (31 total days)
The percentage of ED visits for which the member received
follow-up within 7 days of the ED visit (8 total days).
9. Plan All-Cause Readmissions
For members 18 -64 years of age, the risk-adjusted rate of acute
inpatient stays during the measurement year that were followed by an
unplanned acute readmission for any diagnosis within 30 days.
Facilitate
patient-
centered,
whole person
care
Engage and
partner with
enrollees to
improve enrollee
experience and
outcomes
10. Consumer Assessment of Healthcare Providers and
Systems (CAHPS®) Health Plan Survey 5.1H – Child
Version (Medicaid)
This measure provides information on parents’ experience with their
child’s Medicaid organization.
NCQA
11. Consumer Assessment of Healthcare Providers and
Systems (CAHPS®) Health Plan Survey 5.1H, Adult
Version (Medicaid)
This measure provides information on the experiences of Medicaid
members with the organization and gives a general indication of how
well the organization meets members’ expectations.
12. Children with Chronic Conditions
This measure provides information on parents’ experiences of
Medicaid members with the organization and gives a general
indication of how well the organization meets members’ expectations.
Integrate
behavioral and
physical health
13. Depression Screening and Follow-Up for Adolescents
and Adults
(Please note: This is a pilot measure and LDH will
work with the MCO on strategies to collect this
information. This measure is not required for
reporting).
The percentage of members 12 years of age and older who were
screened for clinical depression using a standardized instrument and,
if screened positive, received follow-up care.
Depression Screening. The percentage of members who
were screened for clinical depression using a standardized
instrument.
Follow-Up on Positive Screen. The percentage of members
who received follow-up care within 30 days of screening
positive for depression.
NCQA
14. Diabetes Screening for People with Schizophrenia or
Bipolar Disorder Who Are Using Antipsychotic
Medications
The percentage of members 18–64 years of age with schizophrenia,
schizoaffective disorder or bipolar disorder, who were dispensed an

Louisiana Medicaid Managed Care Quality Strategy
37
Aims Goals Objectives $$ Measures Measure Description Steward
antipsychotic medication and had a diabetes screening test during the
measurement year.
15. Diabetes Monitoring for People with Diabetes and
Schizophrenia
The percentage of members 18–64 years of age with schizophrenia or
schizoaffective disorder and diabetes who had both an LDL-C test
and an HbA1c test during the measurement year.
16. Cardiovascular Monitoring for People with
Cardiovascular Disease and Schizophrenia
The percentage of members 18–64 years of age with schizophrenia or
schizoaffective disorder and cardiovascular disease, who had an
LDL-C test during the measurement year.
17. Metabolic Monitoring for Children and Adolescents
on Antipsychotics
The percentage of children and adolescents with ongoing
antipsychotic medication use who had metabolic testing during the
year
Healthier
People,
Healthier
Communities.
Improve the
health of
enrollees
through
evidence-
based
prevention and
treatment
interventions
that address
physical and
behavioral
health needs.
Promote
wellness and
prevention
Improve overall
health
18. Self-Reported Overall Health (Adult and Child)
Note: This measure is from the CAHPS survey.
Reporting will be dependent on availability and
validity of data.
The percentage of members reporting overall excellent or very good
health.
AHRQ
19. Self-Reported Overall Mental or Emotional Health
(Adult and Child)
Note: This measure is from the CAHPS survey.
Reporting will be dependent on availability and
validity of data.
The percentage of members reporting overall excellent or very good
mental or emotional health.
Ensure maternal
safety and
appropriate care
during childbirth
and postpartum
20. Prenatal and Postpartum Care: Timeliness of Prenatal
Care
The percentage of deliveries of live births on or between October 8 of
the year prior to the measurement year and October 7 of the
measurement year that received a prenatal care visit in the first
trimester, on or before the enrollment start date or within 42 days of
enrollment in the organization.
NCQA
$$
21. Cesarean Rate for Low-Risk First Birth Women
$$: The percentage of cesareans in live births at or beyond 37.0
weeks gestation to women that are having their first delivery and are
singleton (no twins or beyond) and are vertex presentation (no breech
or transverse positions).
Note: A lower rate indicates better performance.
TJC
22. Prenatal and Postpartum Care: Postpartum Care
The percentage of deliveries of live births on or between October 8
of the year prior to the measurement year and October 7 of the
measurement year that had a postpartum visit on or between 7 and 84
days after delivery.
NCQA
Reduce infant
mortality
23. Percentage of Low Birthweight Births
Percentage of live births that weighted less than 2,500 grams in the
state during the reporting period.
AHRQ

Louisiana Medicaid Managed Care Quality Strategy
38
Aims Goals Objectives $$ Measures Measure Description Steward
Promote healthy
development and
wellness in
children and
adolescents
24. Developmental Screening in the First Three Years of
Life
The percentage of children screened for risk of developmental,
behavioral, and social delays using a standardized screening tool in
the 12 months preceding or on their first, second, or third birthday.
CMS
25. Lead Screening in Children
The percentage of children 2 years of age who had one or more
capillary or venous lead blood test for lead poisoning by their second
birthday.
NCQA
Promote oral
health in children
26. Topical Fluoride for Children
The percentage of members 1-4 years of age who received at least
two fluoride varnish applications during the measurement year.
Report two age stratifications and a total rate:
1-2 years
3-4 years
Total
NCQA
27. Oral Evaluation, Dental Services
The percentage of members under 21 years of age who received a
comprehensive or periodic oral evaluation with a dental provider
during the measurement year. Report four age stratifications and a
total rate:
0-2 years
3-5 years
6-14 years
15-20 years
Total
Improve
immunization
rates
$$
28. Childhood Immunization Status
The percentage of children 2 years of age who had four diphtheria,
tetanus and acellular pertussis (DTaP); three polio (IPV); one
measles, mumps and rubella (MMR); three haemophilus influenza
type B (HiB); three hepatitis B (HepB), one chicken pox (VZV); four
pneumococcal conjugate (PCV); one hepatitis A (HepA); two or three
rotavirus (RV); and two influenza (flu) vaccines by their second
birthday. The measure calculates a rate for each vaccine and nine
separate combination rates. ($$: Combo 3)
NCQA
$$
29. Immunizations for Adolescents
Percentage of adolescents that turned 13 years old during the
measurement year and had specific vaccines by their 13th birthday.
Report all individual vaccine numerators and combinations. ($$:
Combo 2)
Prevent obesity
and address
physical activity
and nutrition in
children and
adults
30. Weight Assessment and Counseling for Nutrition and
Physical Activity for Children/Adolescents – Body
Mass Index Assessment for Children/Adolescents
The percentage of members 3–17 years of age who had an outpatient
visit with a PCP or OB/GYN and who had evidence of the following
during the measurement year.
BMI percentile documentation
Counseling for nutrition
Counseling for physical activity
NCQA
31. Contraceptive Care – All Women Ages 15-20
The percentage of women ages 15-20 who are at risk of unintended
pregnancy and were provided a most or moderately effective method
of contraception or were provided a LARC. Two rates are reported.
OPA

Louisiana Medicaid Managed Care Quality Strategy
39
Aims Goals Objectives $$ Measures Measure Description Steward
32. Contraceptive Care – Postpartum Women Ages 15-20
The percentage of women ages 15-20 who had a live birth and were
provided a most or moderately effective method of contraception
within 3 and 90 days of delivery or were provided a LARC within 3
and 90 days of delivery. Four rates are reported.
Promote
reproductive
health
33. Contraceptive Care – All Women Ages 21–44
The percentage of women ages 21-44 who are at risk of unintended
pregnancy and were provided a most or moderately effective method
of contraception or were provided a LARC. Two rates are reported.
34. Contraceptive Care – Postpartum Women Ages 21–44
The percentage of women ages 21-44 who had a live birth and were
provided a most or moderately effective method of contraception
within 3 and 90 days of delivery or were provided a LARC within 3
and 90 days of delivery. Four rates are reported.
35. Chlamydia Screening in Women
The percentage of women 16–24 years of age who were identified as
sexually active and who had at least one test for Chlamydia during
the measurement year.
NCQA
Improve cancer
screening
$$
36. Cervical Cancer Screening
$$: Percentage of women 21–64 years of age who were screened for
cervical cancer:
Women 21-64 who had cervical cytology performed every 3
years.
Women 30-64 who had cervical cytology/HPV co-testing
performed every 5 years.
NCQA
$$
37. Colorectal Cancer Screening
$$: The percentage of members 45-75 years of age who had
appropriate screening for colorectal cancer. Report two age
stratifications and a total rate:
46-49 years.
50-75 years.
Total.
Improve hepatitis
C virus infection
screening
38. Hepatitis C Virus Screening
Percentage of eligible individuals screened for hepatitis C virus
infection.
State
Promote use of
evidence-based
tobacco cessation
treatments
39. Medical Assistance With Smoking and Tobacco Use
Cessation
Assesses different facets of providing medical assistance with
smoking and tobacco use cessation.
MCOs will report three components (questions):
Advising Smokers and Tobacco Users to Quit
Discussing Cessation Medications
Discussing Cessation Strategies
NCQA
Improve
chronic
disease
Improve
hypertension,
diabetes, and
cardiovascular
disease
$$
40. Controlling High Blood Pressure
$$: The percentage of members 18-85 years of age who had a
diagnosis of hypertension (HTN) and whose blood pressure (BP) was
adequately controlled (<140/90 mm Hg) during the measurement
year.
NCQA
41. Diabetes Short-Term Complications Admission Rate
Number of discharges for diabetes short term complications per
100,000 member months per Medicaid enrollees age 18 and older.
AHRQ

Louisiana Medicaid Managed Care Quality Strategy
40
Aims Goals Objectives $$ Measures Measure Description Steward
management
and control
management and
control
Note: A lower rate indicates better performance.
42. Statin Therapy for Patients with Cardiovascular
Disease
The percentage of males 21-75 years of age and females 40-75
years of age during the measurement year, who were identified as
having clinical atherosclerotic cardiovascular disease (ASCVD)
and who received statin therapy (were dispensed at least one high
or moderate-intensity statin medication during the measurement
year.)
The percentage of males 21-75 years of age and females 40-75
years of age during the measurement year, who were identified as
having clinical atherosclerotic cardiovascular disease (ASCVD)
and who had statin adherence of at least 80% (who remained on a
high or moderate-intensity statin medication for at least 80% of the
treatment period.)
NCQA
43. Heart Failure Admission Rate
Percent of population with an admissions for heart failure (reported
by Recipient Parish). The number of discharges for heart failure per
100,000 member months for Medicaid enrollees age 18 and older
(reported by Recipient Parish).
AHRQ
$$
44. Hemoglobin A1c Control for Patients With Diabetes
The percentage of members 18–75 years of age with diabetes
(types 1 and 2) whose hemoglobin A1c (HbA1c) was at the
following levels during the measurement year:
HbA1c control (<8.0%).
$$: HbA1c poor control (>9.0%)
Note: A lower rate indicates better performance for HbA1c
poor control (i.e., low rates of poor control indicate better
care).
NCQA
45. Blood Pressure Control for Patients With Diabetes
The percentage of members 18–75 years of age with diabetes
(types 1 and 2) whose blood pressure (BP) was adequately
controlled (<140/90 mm Hg) during the measurement year
NCQA
46. Eye Exam for Patients With Diabetes
The percentage of members 18–75 years of age with diabetes
(types 1 and 2) who had a retinal eye exam
NCQA
Improve
respiratory
disease
management and
control
47. Asthma in Younger Adults Admission Rate
Admissions for a principal diagnosis of asthma per 100,000
population, ages 18 to 39 years. Excludes admissions with an
indication of cystic fibrosis or anomalies of the respiratory system,
obstetric admissions, and transfers from other institutions. Number of
discharges for asthma per 100,000 member months for Medicaid
enrollees ages 18 to 39.
Note: A lower rate indicates better performance.
AHRQ
48. Chronic Obstructive Pulmonary Disease or Asthma in
Older Adults Admission Rate
This measure is used to assess the number of admissions for chronic
obstructive pulmonary disease (COPD) per 100,000 population. The

Louisiana Medicaid Managed Care Quality Strategy
41
Aims Goals Objectives $$ Measures Measure Description Steward
number of discharges for chronic obstructive pulmonary disease
(COPD) or asthma per 100,000 member months for Medicaid
enrollees age 40 and older.
Note: A lower rate indicates better performance.
49. Asthma Medication Ratio
The percentage of members 5-64 years of age who were identified as
having persistent asthma and had a ratio of controller medications to
total asthma medications of 0.50 or greater during the measurement
year. Ages 5-64 as of December 31 of the measurement year. Report
the following age stratifications and a total rate:
5-11 years
12-18 years
19-50 years
51-64 years
Total
NCQA
Improve HIV
control
$$
50. HIV Viral Load Suppression
$$: Percentage of patients, regardless of age, with a diagnosis of HIV
with a HIV viral load less than 200.
HRSA
Improve quality
of mental health
and substance
use disorder care
51. Pharmacotherapy for Opioid Use Disorder
The percentage of new opioid use disorder (OUD)
pharmacotherapy episodes that resulted in 180 or more covered
treatment days among members 16 years
of age and older with a diagnosis of OUD
NCQA
52. Initiation and Engagement of Substance Use Disorder
Treatment
The percentage of adolescent and adult members with a new episode
of alcohol or other drug (AOD) abuse or dependence who received
the following.
Initiation of AOD Treatment. The percentage of members who
initiate treatment through an inpatient AOD admission,
outpatient visit, intensive outpatient encounter or partial
hospitalization, telehealth or medication treatment within 14 days
of the diagnosis.
Engagement of AOD Treatment. The percentage of members
who initiated treatment and who had two or more additional
AOD services or medication treatment within 34 days of the
initiation visit.
53. Use of First-Line Psychosocial Care for Children and
Adolescents on Antipsychotics
The percentage of children and adolescents 1–17 years of age who
had a new prescription for an antipsychotic medication and had
documentation of psychosocial care as first-line treatment.
54. Adherence to Antipsychotic Medications for
Individuals with Schizophrenia
The percentage of members 18 years of age and older during the
measurement year with schizophrenia or schizoaffective disorder who
were dispensed and remained on an antipsychotic medication for at
least 80% of their treatment period.
55. Follow-Up Care for Children Prescribed Attention-
Deficit/Hyperactivity Disorder Medication
The percentage of children newly prescribed attention-
deficit/hyperactivity disorder (ADHD) medication who had at least
three follow-up care visits within a 10-month period, one of which

Louisiana Medicaid Managed Care Quality Strategy
42
Aims Goals Objectives $$ Measures Measure Description Steward
was within 30 days of when the first ADHD medication was
dispensed. Two rates are reported.
Initiation Phase. The percentage of members 6–12 years of age as
of the IPSD with an ambulatory prescription dispensed for
ADHD medication, who had one follow-up visit with practitioner
with prescribing authority during the 30-day Initiation Phase.
Continuation and Maintenance (C&M) Phase. The percentage of
members 6–12 years of age as of the IPSD with an ambulatory
prescription dispensed for ADHD medication, who remained on
the medication for at least 210 days and who, in addition to the
visit in the Initiation Phase, had at least two follow-up visits with
a practitioner within 270 days (9 months) after the Initiation
Phase ended.
56. Antidepressant Medication Management
The percentage of members 18 years of age and older with a
diagnosis of major depression and were newly treated with
antidepressant medication, and who remained on an antidepressant
medication treatment. Two rates are reported.
Improve
population
health and
address health
disparities
Stratify key
quality measures
by race/ethnicity
and rural/urban
status and narrow
health disparities
57. Measures for stratified data:
a. Pregnancy: Percentage of Low Birthweight
Births, Contraceptive Care – Postpartum Women
Ages 21–44
b. Child: Well Child Visits in the First 30 Months
of Life, Childhood Immunizations (Combo 3),
Immunizations for Adolescents (Combo 2)
c. Adult: Colorectal Cancer Screening, HIV Viral
Load Suppression, Cervical Cancer Screening
d. Behavioral Health: Follow-Up After Emergency
Department Visit for Mental Illness (within 30
days), Follow-Up After Emergency Department
Visit for Alcohol and Other Drug Abuse or
Dependence (within 30 days), Follow-Up After
Hospitalization for Mental Illness (within 30
days)
*Refer to individual measures
Various
58. Enrollment by Product Line
The total number of members enrolled in the product line, stratified
by age.
NCQA
59. Language Diversity of Membership
An unduplicated count and percentage of members enrolled at any
time during the measurement year by spoken language preferred for
health care and preferred language for written materials.

Louisiana Medicaid Managed Care Quality Strategy
43
Aims Goals Objectives $$ Measures Measure Description Steward
60. Race/Ethnicity Diversity of Membership
An unduplicated count and percentage of members enrolled any time
during the measurement year, by race and ethnicity.
Smarter
Spending.
Advance high-
value, efficient
care.
Minimize
wasteful
spending
Reduce low
value care
61. Appropriate Treatment for Children With Upper
Respiratory Infection
The percentage of children 3 months–18 years of age who were given
a diagnosis of upper respiratory infection (URI) and were not
dispensed an antibiotic prescription.
NCQA
62. Avoidance of Antibiotic Treatment in Adults With
Acute Bronchitis
The percentage of adults 18–64 years of age with a diagnosis of acute
bronchitis who were not dispensed an antibiotic prescription.
63. Use of Imaging Studies for Low Back Pain
The percentage of members with a primary diagnosis of low back
pain who did not have an imaging study (plain X-ray, MRI, CT scan)
within 28 days of the diagnosis.
64. Non-recommended Cervical Cancer Screening in
Adolescent Females
The percentage of adolescent females 16–20 years of age who were
screened unnecessarily for cervical cancer.
Note: A lower rate indicates better performance.
