
MEDICAID
DEMONSTRATIONS
Actions Needed to
Address Weaknesses
in Oversight of Costs
to Administer Work
Requirements
Report to Congressional Requesters
October 2019
GAO-20-149
United States Government Accountability Office

United States Government Accountability Office
Highlights of GAO-20-149, a report to
congressional requesters
October 2019
MEDICAID DEMONSTRATIONS
Actions Needed to
Address Weaknesses in
Oversight
of Costs
to Administer Work Requirements
What GAO Found
Medicaid demonstrations enable states to test new approaches to provide
Medicaid coverage and services. Since January 2018, the Centers for Medicare
& Medicaid Services (CMS) has approved nine states’ demonstrations that
require beneficiaries to work or participate in other activities, such as training, in
order to maintain Medicaid eligibility. The first five states that received CMS
approval for work requirements reported a range of administrative activities to
implement these requirements.
These five states provided GAO with estimates of their demonstrations’
administrative costs, which varied, ranging from under $10 million to over $250
million. Factors such as differences in changes to information technology
systems and numbers of beneficiaries subject to the requirements may have
contributed to the variation. The estimates do not include all costs, such as
ongoing costs states expect to incur throughout the demonstration.
Selected States’ Estimates of Administrative Costs to Implement Work Requirements in
Approved Medicaid Demonstrations and Federal Share of those Costs
State
Number of beneficiaries
subject to requirements
Estimated costs
(dollars in millions)
Estimated federal
share (percentage)
Kentucky
620,000
271.6
87
Wisconsin
150,000
69.4
55
Indiana
420,000
35.1
86
Arkansas
115,000
26.1
83
New Hampshire
50,000
6.1
79
Source: GAO analysis of data reported by selected states and selected state documents. | GAO-20-149
Notes: Estimates of beneficiaries subject to work requirements include those who may be eligible for
an exemption. Estimates of costs do not include all costs, and in Kentucky and Wisconsin include
some costs not specific to work requirements. Estimates generally cover from 1 to 3 years of costs.
GAO found weaknesses in CMS’s oversight of the administrative costs of
demonstrations with work requirements.
• No consideration of administrative costs during approval. GAO found
that CMS does not require states to provide projections of administrative
costs when requesting demonstration approval. Thus, the cost of
administering demonstrations, including those with work requirements, is not
transparent to the public or included in CMS’s assessments of whether a
demonstration is budget neutral—that is, that federal spending will be no
higher under the demonstration than it would have been without it.
• Current procedures may be insufficient to ensure that costs are
allowable and matched at the correct rate. GAO found that three of the
five states received CMS approval for federal funds—in one case, tens of
millions of dollars—for administrative costs that did not appear allowable or
at higher matching rates than appeared appropriate per CMS guidance. The
agency has not assessed the sufficiency of its procedures for overseeing
administrative costs since it began approving demonstrations with work
requirements.
View GAO-20-149. For more information,
contact
Carolyn L. Yocom at (202) 512-7114
or
Why GAO Did This Study
Section 1115 demonstrations are a
significant component of Medicaid
spending and affect the care of millions
of low-income and medically needy
individuals. In 2018, CMS announced a
new policy allowing states to test work
requirements under demonstrations
and soon after began approving such
demonstrations. Implementing work
requirements can involve various
administrative activities, not all of
which are eligible for federal funds.
GAO was asked to examine the
administrative costs of demonstrations
with work requirements. Among other
things, this report examines (1) states’
estimates of costs of administering
work requirements in selected states,
and (2) CMS’s oversight of these
costs. GAO examined the costs of
administering work requirements in the
first five states with approved
demonstrations. GAO also reviewed
documentation for these states’
demonstrations, and interviewed state
and federal Medicaid officials.
Additionally, GAO assessed CMS’s
policies and procedures against federal
internal control standards.
What GAO Recommends
GAO makes three recommendations,
including that CMS (1) require states to
submit projections of administrative
costs with demonstration proposals,
and (2) assess risks of providing
federal funds that are not allowable to
administer work requirements and
improve oversight procedures, as
warranted. CMS did not concur with
the recommendations and stated that
its procedures are sufficient given the
level of risk. GAO maintains that the
recommendations are warranted as
discussed in this report.

Page i GAO-20-149 Medicaid Demonstration Administrative Costs
Letter 1
Background 6
States’ Work Requirements Varied in Terms of Target Population,
Required Activities, and Consequences of Non-Compliance 14
Available Estimates of Costs to Implement Work Requirements
Varied among Selected States, with the Majority of Costs
Expected to Be Financed by Federal Dollars 19
Weaknesses Exist in CMS’s Oversight of Administrative Costs of
Demonstrations with Work Requirements 25
Conclusions 34
Recommendation for Executive Action 34
Agency Comments and Our Evaluation 34
Appendix I Other Beneficiary Requirements in States with Approved Medicaid
Work Requirements 38
Appendix II Comments from the Department of Health and Human Services 40
Appendix III GAO Contact and Staff Acknowledgments 44
Related GAO Reports 45
Tables
Table 1: Beneficiary Groups Subject to and Characteristics of
Medicaid Work Requirements in States that Received
Approval for Such Requirements, as of May 2019 15
Table 2: Beneficiary Consequences for Non-Compliance with
Medicaid Work Requirements in States with Approved
Requirements, as of May 2019 17
Table 3: Selected States’ Estimates of Administrative Costs and of
Initial Expenditures for Implementing Medicaid Work
Requirements 20
Table 4: CMS Initiatives that May Provide the Agency with
Information on Demonstration Administrative Costs 27
Contents

Page ii GAO-20-149 Medicaid Demonstration Administrative Costs
Table 5: Other Beneficiary Requirements in States with Approved
Medicaid Work Requirements, as of May 2019 38
Figures
Figure 1: States with Approved or Pending 1115 Demonstrations
with Work Requirements, as of May 2019 9
Figure 2: Approval and Effective Dates for States with Approved
Work Requirements, as of August 2019 10
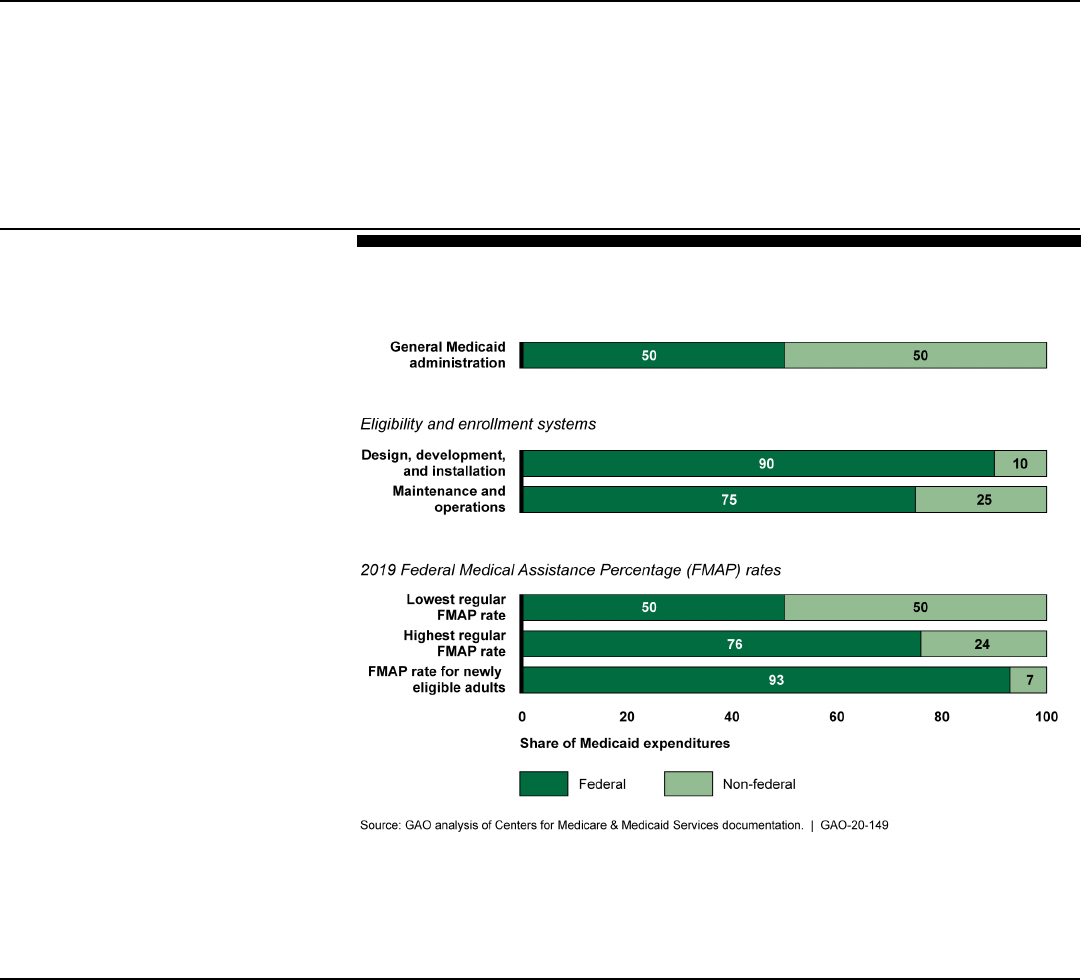
Figure 3: Federal and Non-Federal Shares for Selected Types of
Medicaid Expenditures, Fiscal Year 2019 12

Page iii GAO-20-149 Medicaid Demonstration Administrative Costs
Abbreviations
CMS Centers for Medicare & Medicaid Services
FMAP Federal Medical Assistance Percentage
HHS Department of Health and Human Services
IT information technology
MCO managed care organization
PPACA Patient Protection and Affordable Care Act
SNAP Supplemental Nutritional Assistance Program
TANF Temporary Assistance to Needy Families
This is a work of the U.S. government and is not subject to copyright protection in the
United States. The published product may be reproduced and distributed in its entirety
without further permission from GAO. However, because this work may contain
copyrighted images or other material, permission from the copyright holder may be
necessary if you wish to reproduce this material separately.

Page 1 GAO-20-149 Medicaid Demonstration Administrative Costs
441 G St. N.W.
Washington, DC 20548
October 1, 2019
The Honorable Ron Wyden
Ranking Member
Committee on Finance
United States Senate
The Honorable Frank Pallone, Jr.
Chairman
Committee on Energy and Commerce
House of Representatives
Medicaid section 1115 demonstrations—which allow states to test and
evaluate new approaches for delivering health care services under the
federal-state Medicaid program—have become a significant feature of the
program.
1
Section 1115 of the Social Security Act authorizes the
Secretary of Health and Human Services to waive certain federal
Medicaid requirements and approve new types of expenditures that would
not otherwise be eligible for federal Medicaid funds for experimental, pilot,
or demonstration projects that, in the Secretary’s judgment, are likely to
promote Medicaid objectives.
2
As of November 2018, over three-quarters
of states operated at least part of their Medicaid program under a section
1115 demonstration; in fiscal year 2017, federal spending for
demonstrations was about $145 billion, or over one-third of federal
Medicaid program expenditures.
The Centers for Medicare & Medicaid Services (CMS), within the
Department of Health and Human Services (HHS), oversees Medicaid
section 1115 demonstrations (referred to hereafter as demonstrations)
and has approved states’ use of demonstrations for a variety of purposes.
For example, under demonstrations, states have extended coverage to
populations, offered services not otherwise eligible for Medicaid, and
increased beneficiary premiums and cost-sharing above statutory limits.
1
Medicaid is a joint, federal-state program that finances health care coverage for low-
income and medically needy individuals. The program is a significant component of
federal and state budgets. It covered an estimated 75 million individuals at an estimated
cost of $629 billion in fiscal year 2018, including about $393 billion in federal spending and
$236 billion in state spending, according to estimates from the Centers for Medicare &
Medicaid Services’ Office of the Actuary.
2
42 U.S.C. § 1315(a).
Letter

Page 2 GAO-20-149 Medicaid Demonstration Administrative Costs
In January 2018, CMS issued guidance announcing a new opportunity for
states to use demonstrations to require certain beneficiaries to work or
participate in community engagement activities, such as vocational
training or volunteer activities, as a condition of Medicaid eligibility.
3
CMS
gave states flexibility in designing the work requirements within certain
parameters. Medicaid beneficiaries not meeting these work requirements
can face suspension or termination of coverage if they do not meet—and
do not appropriately report having met—the number of hours of activity
required. CMS approved the first demonstration testing work
requirements in Kentucky in January 2018 and has since approved such
requirements in eight other state demonstrations, with seven more state
demonstration applications pending as of May 2019. While work
requirements have long been a feature of programs such as Temporary
Assistance to Needy Families (TANF), CMS has not previously approved
work requirements in state Medicaid programs. As of August 2019, there
is ongoing litigation challenging CMS’s approvals of such requirements in
three states that had implemented, or were preparing to implement, work
requirements: Arkansas, Kentucky, and New Hampshire.
4
Implementing work requirements—like other changes in Medicaid—can
increase Medicaid administrative costs, as states may need to change
eligibility and enrollment systems and conduct additional beneficiary
outreach, monitoring, and evaluation.
5
In general, the federal government
3
According to CMS’s guidance, work requirements are to be targeted to non-elderly, non-
pregnant adult Medicaid beneficiaries who are eligible for Medicaid on a basis other than
disability. The guidance indicates that states will be required to provide exemptions for
beneficiaries based on medical frailty, disability, and other reasons. See CMS, State
Medicaid Director Letter; Re: Opportunities to Promote Work and Community Engagement
Among Medicaid Beneficiaries, SMD: 18-002 (Baltimore, Md.: Jan. 11, 2018).
CMS and states have used various terms to refer to these requirements including “work
requirements,” “community engagement requirements,” and “work and community
engagement requirements.” We use the term “work requirements” in this report consistent
with how similar requirements are referenced by other federal programs, including the
Supplemental Nutritional Assistance Program (SNAP) and Temporary Assistance to
Needy Families (TANF).
4
The U.S. District Court for the District of Columbia vacated CMS’s approvals of the
Arkansas and Kentucky demonstrations with work requirements in March 2019 and CMS’s
approval of New Hampshire’s demonstration in July 2019. Gresham v. Azar, 363 F. Supp.
3d 165 (D.D.C. 2019); Stewart v. Azar, 366 F. Supp. 3d 125 (D.D.C. 2019); Philbrick v.
Azar, No. 19-773 (JEB) (D.D.C. July 29, 2019). As of August 2019, CMS was appealing
the decisions vacating demonstrations in Arkansas and Kentucky.
5
In fiscal year 2018, Medicaid administrative expenditures were estimated to be $28.8
billion or about 4.6 percent of total Medicaid expenditures, according to CMS’s Office of
the Actuary.

Page 3 GAO-20-149 Medicaid Demonstration Administrative Costs
provides 50 percent of the funds for administrative costs, but pays for up
to 90 percent of certain costs, including those for information technology
(IT) system changes. CMS is responsible for overseeing Medicaid
administrative spending and ensuring that federal matching funds are
only provided for costs that are allowable under Medicaid rules.
Stakeholders have raised concerns that work requirements will increase
administrative costs.
Given the number of states opting to test work requirements, you asked
us to examine the administrative costs of demonstrations with work
requirements and CMS oversight of those expenditures. This report
examines
1. characteristics of work requirements in states with approved
demonstrations and pending applications;
2. selected states’ estimates of the administrative costs to implement
demonstrations with work requirements; and
3. CMS’s oversight of the administrative costs of demonstrations with
work requirements.
To examine the characteristics of work requirements in states that have
received approval and those with pending demonstration applications, we
reviewed demonstration documentation from CMS. Specifically, we
reviewed approval documents for the nine states that had received CMS
approval as of May 2019.
6
As part of our review, we identified the extent
of variation across states in the beneficiary groups subject to the work
requirements, including the age and eligibility groups; the hours of work
required and frequency of required reporting; and the consequences for
non-compliance, including both the nature of the consequence—
suspension or termination of coverage—and when it would take effect.
7
We also identified the extent of any variation in the populations states
exempted from the work requirements and the types of activities that met
the requirements. For the seven states with demonstration applications to
6
The nine states that received approval included Arizona, Arkansas, Indiana, Kentucky,
Michigan, New Hampshire, Ohio, Utah, and Wisconsin. A tenth state, Maine, received
CMS approval for work requirements, but the state subsequently terminated the
demonstration. As such, we did not include Maine in our review.
7
Medicaid eligibility groups include low-income individuals who meet financial and
categorical requirements, such as adults, pregnant women, parents and children,
individuals who are aged, and individuals with disabilities.

Page 4 GAO-20-149 Medicaid Demonstration Administrative Costs
implement work requirements that were pending as of May 2019, we
reviewed application documents for these same characteristics.
To examine selected states’ estimates of the administrative costs of
demonstrations with work requirements, we reviewed state data and
documentation for the five selected states that had received approval as
of November 2018. These states—Arkansas, Indiana, Kentucky, New
Hampshire, and Wisconsin—had the most time to implement work
requirements or make significant preparations to do so during the time
that we conducted our review.
8
Using a data collection instrument
provided to the selected states, we collected available estimates of the
administrative costs for implementing and administering work
requirements over the course of the demonstration approval periods (3 to
5 years), including the states’ estimates of federal and non-federal costs.
9
We also requested available information on the amounts of expenditures
for implementing and administering work requirements incurred from the
date the state submitted its application through the end of calendar year
2018.
10
We asked the selected states to break those expenditures out
according to several types of administrative activities, such as
implementation and operation of IT systems, beneficiary outreach, and
staff training, as well as by expected federal and non-federal amounts.
8
As noted earlier, the U.S. District Court for the District of Columbia vacated approvals for
Arkansas and Kentucky in March 2019 and the approval for New Hampshire in July 2019.
We included these states in the scope of our review because they had completed
implementation activities prior to the approvals being vacated. Arkansas received approval
of its demonstration in March 2018, implemented work requirements on June 1, 2018, and
administered the requirements for 9 months before the relevant approval was vacated.
Kentucky received approval for its demonstration in January 2018 and initially prepared to
implement work requirements on July 1, 2018. That approval was vacated on June 29,
2018. Kentucky received a new approval for work requirements in November 2018 and
began preparing for implementation in April 2019 before that approval was vacated on
March 27, 2019. New Hampshire received approvals for its demonstration in May and
November 2018, and implemented the demonstration in March 2019 before its approval
was vacated 4 months later.
9
States finance the non-federal share of Medicaid costs in large part through state general
funds and depend on other sources of funds, such as taxes on health care providers and
funds from local governments, to finance the remainder.
10
States sometimes began IT system development activities while their applications were
under review. According to CMS, states can receive federal approval and funds for related
expenditures prior to the approval of the demonstration to the extent CMS determines they
are reasonable and align with required business processes. See, CMS, Medicaid and
CHIP Frequently Asked Questions (FAQs) Advanced Planning Documents (APD) for
System Development Associated with 1115 Demonstrations (Baltimore, Md.: June 13,
2019). Selected states submitted applications between August 2016 and July 2018.

Page 5 GAO-20-149 Medicaid Demonstration Administrative Costs
Where states could not provide expenditure amounts for a given type of
activity, we asked them to affirm whether expenditures were incurred for
that activity. We also reviewed related state documentation detailing the
use of the these funds, including descriptions of changes to IT systems
and agreements state Medicaid agencies entered into with managed care
organizations (MCO) or other state agencies to carry out administrative
tasks related to work requirements.
11
In addition, we interviewed Medicaid
officials in the five selected states and asked them about the
administrative activities they had undertaken or planned to take to
implement work requirements, expected ongoing annual costs, and
factors that affected implementation costs. We used our reviews of state
documentation and interviews with officials to identify any inconsistencies
or limitations in the data reported by the states. Based on these steps, we
found the data were sufficiently reliable for the purpose of our reporting
objectives.
To examine CMS’s oversight of the administrative costs of
demonstrations with work requirements, we reviewed documentation of
policies and procedures for approving, monitoring, and evaluating
demonstrations. This included the policies and procedures applied to all
demonstrations, as well as those applied to demonstrations with work
requirements.
12
We also reviewed policies and procedures for approving
federal funds for changes to Medicaid IT systems. In addition, for our five
selected states, we reviewed state demonstration applications and
interviewed state Medicaid officials about information the states provided
to CMS during the approval process about projected administrative costs.
11
Descriptions of changes to IT systems included proposals submitted by states to CMS
for approval of federal funds at higher federal matching rates available for certain system
development, and maintenance and operations costs, or for updates to previous
approvals, correspondence between the state and CMS on those proposals, and approval
documents.
12
With regard to policies and procedures with general application, we reviewed regulations
detailing state requirements and CMS procedures for transparency of demonstration
approvals and outcomes. 42 C.F.R. pt. 431 subpt. G. We also reviewed CMS’s policy for
ensuring that demonstrations are budget neutral. CMS, State Medicaid Director Letter; Re:
Budget Neutrality Policies for Section 1115(a) Medicaid Demonstration Projects, SMD: 18-
009 (Baltimore, Md.: Aug. 22, 2018). For policies and procedures specific to work and
community engagement requirements, we reviewed guidance to states, issued in January
2018, on applying for approval of work requirements, as well as subsequent guidance,
issued in March 2019, on monitoring and evaluation of demonstrations with work
requirements. CMS, SMD: 18-002; and CMS, 1115 Demonstration State Monitoring &
Evaluation Resources, accessed March 14, 2019,
https://www.medicaid.gov/medicaid/section-1115-demo/evaluation-reports/evaluation-
designs-and-reports/index.html.
Page 6 GAO-20-149 Medicaid Demonstration Administrative Costs
We also reviewed state documents detailing plans for obtaining and using
federal funds for the administrative costs associated with work
requirements and related CMS approval documents. We compared
states’ plans with CMS policy on allowable administrative activities—
those eligible for federal Medicaid matching funds—and the appropriate
federal matching rates for those activities. We also interviewed CMS
officials about the extent to which CMS considers administrative costs
when approving demonstrations, how CMS oversees the administrative
costs of demonstrations through the approval of IT funds and other
processes, and how CMS ensures that states receive appropriate federal
matching rates for allowable administrative costs under Medicaid rules.
Finally, we assessed CMS’s policies and procedures against federal
standards for internal controls related to risk assessment.
13
We conducted this performance audit from August 2018 to September
2019 in accordance with generally accepted government auditing
standards. Those standards require that we plan and perform the audit to
obtain sufficient, appropriate evidence to provide a reasonable basis for
our findings and conclusions based on our audit objectives. We believe
that the evidence obtained provides a reasonable basis for our findings
and conclusions based on our audit objectives.
As of November 2018, 43 states operated at least part of their Medicaid
programs under demonstrations. State demonstrations can vary in size
and scope, and many demonstrations are comprehensive in nature,
affecting multiple aspects of states’ Medicaid programs. In fiscal year
2017, federal spending on demonstrations accounted for more than one-
third of total federal Medicaid spending and in eight states accounted for
75 percent or more of Medicaid expenditures.
CMS typically approves demonstrations for an initial 5-year period that
can be extended in 3- to 5-year increments with CMS approval. Some
states have operated portions of their Medicaid programs under a
13
See GAO, Standards for Internal Control in the Federal Government, GAO-14-704G
(Washington, D.C.: Sept. 10, 2014). Internal control is a process affected by an entity’s
oversight body, management, and other personnel that provides reasonable assurance
that the objectives of an entity will be achieved.
Background
Medicaid Section 1115
Demonstrations

Page 7 GAO-20-149 Medicaid Demonstration Administrative Costs
demonstration for decades. Each demonstration is governed by special
terms and conditions, which reflect the agreement reached between CMS
and the state, and describe the authorities granted to the state. For
example, the special terms and conditions may define what
demonstration funds can be spent on—including which populations and
services—as well as specify reporting requirements, such as monitoring
or evaluation reports states must submit to CMS.
In January 2018, CMS announced a new policy to support states
interested in using demonstrations to make participation in work or
community engagement a requirement to maintain Medicaid eligibility or
coverage.
14
CMS’s guidance indicates that states have flexibility in
designing demonstrations that test work requirements, but it also
describes parameters around the populations that could be subject to
work requirements and other expectations. CMS guidance addresses
several areas, including the following:
• Populations. Work requirements should apply to working-age, non-
pregnant adult beneficiaries who qualify for Medicaid on a basis other
than a disability.
• Exemptions and qualifying activities. States must create
exemptions for individuals who are medically frail or have acute
medical conditions. States must also take steps to ensure eligible
individuals with opioid addiction and other substance use disorders
have access to coverage and treatment services and provide
reasonable modifications for them, such as counting time spent in
medical treatment toward work requirements. The guidance indicates
that states can allow a range of qualifying activities that satisfy work
requirements, such as job training, education programs, and
community service. The guidance also encourages states to consider
aligning Medicaid work requirements with work requirements in other
federal assistance programs operating in their states.
15
14
See CMS, SMD: 18-002.
15
For example, SNAP includes work requirements that certain adult participants must
comply with as a condition of eligibility for benefits. However, certain participants are
exempt from SNAP work requirements, such as those who are physically unfit for
employment or those participating in a drug addiction or alcohol treatment and
rehabilitation program.
Work Requirements

Page 8 GAO-20-149 Medicaid Demonstration Administrative Costs
• Beneficiary supports. States are expected to describe their
strategies to assist beneficiaries in meeting work requirements and to
link them to additional resources for job training, child care assistance,
transportation, or other work supports. However, CMS’s guidance
specifies that states are not authorized to use Medicaid funds to
finance these beneficiary supports.
About one-third of states have either received CMS approval or submitted
applications to CMS to test work requirements in their demonstrations.
Nine states have had work requirements approved as part of new
demonstrations or extensions of or amendments to existing
demonstrations as of May 2019.
16
Also as of May 2019, seven more
states had submitted demonstration applications with work requirements,
which were pending CMS approval. (See fig. 1.)
16
CMS also approved a demonstration for Maine to institute work requirements in
December 2018, with implementation scheduled for July 2019. However, in January 2019,
Maine communicated to CMS that the state would not be implementing the demonstration.

Page 9 GAO-20-149 Medicaid Demonstration Administrative Costs
Figure 1: States with Approved or Pending 1115 Demonstrations with Work Requirements, as of May 2019
a
A federal district court vacated CMS’s approvals of demonstrations in Arkansas and Kentucky in
March 2019, and in New Hampshire in July 2019; as of August 2019, CMS was appealing the
decisions vacating demonstrations in Arkansas and Kentucky. CMS approved a demonstration for
Maine to institute work requirements in December 2018. However, in January 2019, Maine
communicated to CMS that the state would not be implementing the demonstration, and, as a result,
we listed Maine as having no pending or approved application.

Page 10 GAO-20-149 Medicaid Demonstration Administrative Costs
States with approved work requirements were in various stages of
implementation as of August 2019, and three states faced legal
challenges to implementation. The requirements were in effect in
Arkansas for 9 months before a federal district court vacated the approval
in March 2019.
17
Work requirements became effective in Indiana in
January 2019 and will be enforced beginning in January 2020. CMS’s
approval of work requirements in Kentucky was vacated in March 2019—
several days before the work requirements were set to become effective
on April 1, 2019.
18
As of August 2019, CMS was appealing the court
decisions vacating demonstration approvals in Arkansas and Kentucky.
Other states’ requirements are approved to take effect in fiscal years
2020 and 2021. (See fig. 2.)
Figure 2: Approval and Effective Dates for States with Approved Work Requirements, as of August 2019
17
Gresham v. Azar, 363 F. Supp. 3d 165 (D.D.C. 2019).
18
CMS’s initial approval of Kentucky’s demonstration in January 2018 was vacated by the
U.S. District Court for the District of Columbia in June 2018. Stewart v. Azar, 313 F. Supp.
3d 237 (D.D.C. 2018). CMS reapproved Kentucky’s demonstration on November 20,
2018. The U.S. District Court for the District of Columbia vacated this approval on March
27, 2019. Stewart v. Azar, 366 F. Supp. 3d 125 (D.D.C. 2019).

Page 11 GAO-20-149 Medicaid Demonstration Administrative Costs
Notes: Kentucky was first approved to implement work requirements in January 2018; this approval
was vacated by the U.S. District Court for the District of Columbia in June 2018. CMS reapproved
Kentucky’s demonstration in November 2018. New Hampshire was first approved in May 2018 to
implement work requirements, and, in November 2018, CMS approved an extension of the state’s
demonstration, including its work requirements. Under the terms of the approvals, states have
discretion to delay effective dates for work requirements.
Implementing work requirements, as with other types of beneficiary
requirements, can involve an array of administrative activities by states,
including developing or adapting eligibility and enrollment systems,
educating beneficiaries, and training staff. In general, CMS provides
federal funds for 50 percent (referred to as a 50 percent matching rate) of
state Medicaid administrative costs. These funds are for activities
considered necessary for the proper and efficient administration of a
state’s Medicaid program, including those parts operated under
demonstrations.
19
CMS provides higher matching rates for certain
administrative costs, including those related to IT systems. For example,
expenditures to design, develop, and install Medicaid eligibility and
enrollment systems are matched at 90 percent, and maintenance and
operations of these systems are matched at 75 percent.
20
States may also receive federal funds for administrative activities
delegated to MCOs. The amount of federal Medicaid funds states receive
for payments to MCOs that bear financial risk for Medicaid expenditures
is determined annually by a statutory formula based on the state’s per
capita income, known as the Federal Medical Assistance Percentage
(FMAP).
21
The FMAP sets a specific federal matching rate for each state
that, for fiscal year 2019, ranges from 50 percent to 76 percent. There are
exceptions to this rate for certain populations, providers, and services.
For example, states that chose to expand Medicaid under the Patient
Protection and Affordable Care Act (PPACA) receive a higher FMAP for
newly eligible adults, equal to 93 percent in 2019.
22
(See fig. 3.)
19
42 U.S.C. § 1396b(a)(7).
20
42 U.S.C. § 1396b(a)(3)(A)(i), (a)(3)(B).
21
42 U.S.C. § 1396d(b). The FMAP applies broadly to Medicaid expenditures, including
expenditures for most Medicaid services.
22
Newly eligible adults under PPACA include nonelderly, nonpregnant adults who are not
eligible for Medicare, and whose income does not exceed 138 percent of the federal
poverty level. The FMAP for newly eligible adults will decrease to 90 percent in 2020.
Federal Funding for
Administrative Costs to
Implement Work
Requirements
Page 12 GAO-20-149 Medicaid Demonstration Administrative Costs
Figure 3: Federal and Non-Federal Shares for Selected Types of Medicaid
Expenditures, Fiscal Year 2019
Notes: The FMAP is a statutory formula that determines the federal government’s share for most
Medicaid expenditures based on each state’s per capita income relative to the national average. In
2019, the federal share ranged from 50 percent to 76 percent. Newly eligible adults refer to
individuals eligible because their state chose to expand Medicaid under the Patient Protection and
Affordable Care Act. Under the act, costs for these individuals are matched at a higher rate than the
regular FMAP rates.
CMS has several different related processes under which the agency
oversees Medicaid administrative costs, including those for
demonstrations.
• Demonstration approval, monitoring, and evaluation. States
seeking demonstration approvals must meet transparency
requirements established by CMS. For example, states must include
certain information about the expected changes in expenditures under
the demonstration in public notices seeking comment at the state level
and in the application to CMS, which is posted for public comment at
the federal level. In addition, CMS policy requires that demonstrations
be budget neutral—that is, that the federal government should spend
no more under a demonstration than it would have without the
demonstration. Prior to approval, states are required to submit an
CMS Oversight of
Administrative Costs

Page 13 GAO-20-149 Medicaid Demonstration Administrative Costs
analysis of their projected costs with and without the demonstration.
CMS uses this information to determine budget neutrality and set
spending limits for demonstrations. During the demonstration, CMS is
responsible for monitoring the state’s compliance with the terms and
conditions of the demonstration, including those related to how
Medicaid funds can be spent and the demonstration spending limit.
States must also evaluate their demonstrations to assess the effects
of the policies being tested, which could include impacts on cost.
• Review and approval of federal matching funds for IT projects.
To request higher federal matching rates for changes to Medicaid IT
systems, including eligibility and enrollment systems, states must
submit planning documents to CMS for review and approval. States’
plans must include sufficient information to evaluate the state’s goals,
procurement approach, and cost allocations within a specified budget.
States may request funds for system development related to a
proposed demonstration before the demonstration is approved.
Funding can be approved and expended under the approved plan
while the demonstration application is being reviewed.
23
States submit
updates to planning documents annually for CMS review, which can
include requested changes to the approved budget.
• Quarterly expenditure reviews. In order to receive federal matching
funds, states report their Medicaid expenditures quarterly to CMS,
including those made under demonstrations. Expenditures associated
with demonstrations, including administrative expenditures, are
reported separately from other expenditures. CMS is responsible for
ensuring that expenditures reported by states are supported and
allowable, meaning that the state actually made and recorded the
expenditure and that the expenditure is consistent with Medicaid
requirements. With regard to consistency, this includes comparing
reported expenditures to various approval documents. For example,
CMS is responsible for comparing reported demonstration
expenditures against the special terms and conditions that authorize
payment for specified services or populations and establish spending
limits. CMS is also responsible for reviewing states’ reported
expenditures against budgets in states’ planning documents to ensure
that states do not exceed approved amounts.
A list of GAO reports related to these CMS oversight processes is
included at the end of this report.
23
CMS’s process recognizes that for timely implementation, some system design,
development, and installation may need to occur prior to demonstration approval.

Page 14 GAO-20-149 Medicaid Demonstration Administrative Costs
States took different approaches to designing work requirements under
their Medicaid demonstrations. These requirements varied in terms of the
beneficiary groups subject to the requirements; the required activities,
such as frequency of required reporting; and the consequences
beneficiaries face if they do not meet requirements.
In the nine states with approved work requirements as of May 2019, we
found differences in the age and eligibility groups subject to work
requirements, and, to a lesser extent, the number of hours of work
required and frequency of required reporting to the state. For example:
• Age and eligibility groups subject to work requirements. Four of
these states received approval to apply the requirements to adults
under the age of 50, similar to how certain work requirements are
applied under the Supplemental Nutrition Assistance Program
(SNAP).
24
Among the other five states, approved work requirements
apply to adults up to the age of 59 (Indiana and Utah), 62 (Michigan),
and 64 (Kentucky and New Hampshire). States generally planned to
apply the requirements to adults newly eligible under PPACA or a
previous coverage expansion, but some states received approval to
apply the requirements to additional eligibility groups, such as parents
and caretakers of dependents.
25
• Number of hours of work required and frequency of required
reporting. Under approved demonstrations in seven states, Medicaid
beneficiaries must complete 80 hours of work or other qualifying
24
Generally, SNAP recipients ages 18 through 49 who are not physically or mentally unfit
for employment, are in a household not responsible for a dependent child, and do not
meet other exemptions must work or participate in a work program 20 hours or more per
week or otherwise earn the value of their SNAP benefits. In addition, SNAP recipients
ages 16 through 59 must generally comply with general work requirements that typically
include registering for work and may include additional required activities.
25
Prior to PPACA, states could expand coverage to populations not traditionally eligible for
Medicaid—such as childless adults—using state funds or through a section 1115
demonstration.
States’ Work
Requirements Varied
in Terms of Target
Population, Required
Activities, and
Consequences of
Non-Compliance
Beneficiaries Subject to
Work Requirements and
Required Activities

Page 15 GAO-20-149 Medicaid Demonstration Administrative Costs
activities per month to comply with work requirements. Five states’
approved demonstrations require beneficiaries to report each month
on their hours of work or other qualifying activities, using methods
approved by the state, such as online or over the phone. (See table
1.)
We saw similar variation under the seven state applications that were
pending as of May 2019.
26
Table 1: Beneficiary Groups Subject to and Characteristics of Medicaid Work Requirements in States that Received Approval
for Such Requirements, as of May 2019
Beneficiary groups subject to the work requirements
Beneficiary reporting requirements
State
Maximum age
Newly eligible
adults
a
Other eligibility
groups
b
Number of
hours required
monthly
Frequency of
required
reporting to state
Arizona
49
✓
—
80
Monthly
Arkansas
49
✓
—
80
Monthly
Indiana
59
✓
✓
80
Annually
Kentucky
64
✓
✓
80
Monthly
Michigan
62
✓
—
80
Monthly
New Hampshire
64
✓
—
100
Monthly
Ohio
49
✓
—
80
Annually
Utah
59
c
✓
d
Annually
Wisconsin
49
c
—
80
e
Legend:
✓ = yes
— = not applicable
Source: Centers for Medicare & Medicaid Services (CMS) documentation. | GAO-20-149
Note: The U.S. District Court for the District of Columbia vacated CMS’s approvals of demonstrations
in Arkansas and Kentucky in March 2019, and in New Hampshire in July 2019. Gresham v. Azar, 363
F. Supp. 3d 165 (D.D.C. 2019); Stewart v. Azar, 366 F. Supp. 3d 125 (D.D.C. 2019); Philbrick v. Azar,
No. 19-773 (JEB) (D.D.C. July 29, 2019).
a
The Patient Protection and Affordable Care Act (PPACA) permitted states to expand Medicaid
coverage to nonelderly, non-pregnant adults who are not eligible for Medicare and whose income
does not exceed 138 percent of the federal poverty level.
b
This includes such groups as parents and caretakers of dependents.
26
States’ pending applications varied in terms of the age groups subject to the
requirements with maximum ages ranging from 50 years to 65 years. In terms of eligibility
groups, six of the seven states had not expanded Medicaid to those newly eligible under
PPACA. Thus, those states’ applications focused the work requirements on other eligibility
groups, such as parents and caretakers of dependents. All seven states were seeking
approval to require beneficiaries to complete 80 hours per month (or 20 hours per week)
of work or other qualifying activities, and one state planned to require childless adults to
participate 30 hours per week.

Page 16 GAO-20-149 Medicaid Demonstration Administrative Costs
c
Utah and Wisconsin expanded coverage to adults with incomes at or below 100 percent—rather than
138 percent—of the federal poverty level and gained approval to subject those beneficiaries to work
requirements.
d
Utah requires beneficiaries to work 30 hours per week or complete a set of qualifying activities.
e
Wisconsin’s approval to implement work requirements does not specify the frequency of required
reporting.
All nine states with approved work requirements as of May 2019
exempted several categories of beneficiaries and counted a variety of
activities as meeting the work requirements. For example, all nine states
exempted from the work requirements people with disabilities, pregnant
women, and those with certain health conditions, such as a serious
mental illness.
27
In addition, depending on the state, other groups were
also exempted, such as beneficiaries who are homeless, survivors of
domestic violence, and those enrolled in substance use treatment
programs. States also counted activities other than work as meeting the
work requirements, such as job training, volunteering, and caregiving for
non-dependents. In addition to work requirements, eight of the nine states
received approval under their demonstrations to implement other
beneficiary requirements, such as requiring beneficiaries to have
expenditure accounts.
28
(See app. I for more information on these other
beneficiary requirements.)
The consequences Medicaid beneficiaries faced for non-compliance and
the timing of the consequences varied across the nine states with
approved work requirements. The consequences for non-compliance
included coverage suspension and termination.
29
For example, Arizona
received approval to suspend beneficiaries’ coverage after 1 month of
non-compliance. In contrast, Wisconsin will not take action until a
beneficiary has been out of compliance for 4 years, at which time
27
CMS guidance requires states to exempt certain populations, such as individuals
determined to be medically frail and individuals classified as “disabled” for Medicaid
eligibility purposes, and to make reasonable modifications for others.
28
Beneficiary expenditure accounts are similar to health savings accounts where funds are
used to pay for health care expenses.
29
Under a suspension, beneficiaries remain enrolled, but coverage is suspended until they
come into compliance with the work requirements or a specified period of time has
elapsed. Under termination, enrollment in the Medicaid program is terminated for
individuals and they must reapply to regain coverage. In some states, coverage may first
be suspended and subsequently terminated if beneficiaries do not come into compliance
by their annual eligibility redetermination.
Beneficiary Consequences
for Non-Compliance

Page 17 GAO-20-149 Medicaid Demonstration Administrative Costs
coverage will be terminated. Three states (Arkansas, Michigan, and
Wisconsin) imposed or planned to impose a non-eligibility period after
terminating a beneficiary’s enrollment.
30
For example, under Arkansas’
demonstration, after 3 months of non-compliance, the beneficiary was not
eligible to re-enroll until the next plan year, which began in January of
each year. Thus, beneficiaries could be locked out of coverage for up to 9
months. (See table 2.) For states with pending applications, suspension
or termination of coverage takes effect after 2 or 3 months of non-
compliance.
Table 2: Beneficiary Consequences for Non-Compliance with Medicaid Work Requirements in States with Approved
Requirements, as of May 2019
State
Number of months of non-
compliance before consequence Type of consequence
a
Non-eligibility period
b
Arizona
1
Suspension
—
Arkansas
3 in a calendar year
Termination
0 to 9 months
Indiana
4 in a calendar year
Suspension then termination
—
Kentucky
2 in a row
Suspension then termination
—
Michigan
3 in 12 months
Termination
At least 1 month
New Hampshire
2 in a row
Suspension then termination
—
Ohio
2 (60 days)
Termination
—
Utah
3 in 12 months
Termination
—
Wisconsin
48
Termination
6 months
Legend:
— = not applicable
Source: Centers for Medicare & Medicaid Services (CMS) documentation. | GAO-20-149
Note: The U.S. District Court for the District of Columbia vacated CMS’s approvals of demonstrations
in Arkansas and Kentucky in March 2019, and in New Hampshire in July 2019. Gresham v. Azar, 363
F. Supp. 3d 165 (D.D.C. 2019); Stewart v. Azar, 366 F. Supp. 3d 125 (D.D.C. 2019); Philbrick v. Azar,
No. 19-773 (JEB) (D.D.C. July 29, 2019).
a
Under a suspension, beneficiaries remain enrolled, but coverage is suspended until they come into
compliance with the work requirements or a specified period of time has elapsed. Under termination,
enrollment in the Medicaid program is terminated for individuals and they must reapply to regain
coverage. In some states, coverage may first be suspended and subsequently terminated if
beneficiaries do not come into compliance by their annual eligibility redetermination.
b
States with a non-eligibility period restrict an individual from reenrolling in the program following a
coverage termination due to noncompliance with the work requirements for a set period of time or
until certain conditions are met.
30
States with a non-eligibility period restrict an individual from reenrolling in the program
following a coverage termination due to noncompliance with the work requirements for a
set period of time or until certain conditions are met.
Page 18 GAO-20-149 Medicaid Demonstration Administrative Costs
For states that suspend coverage for beneficiaries, there are different
conditions for coming into compliance and lifting the suspension. For
example:
• Arizona received approval to automatically reactivate an individual’s
eligibility at the end of each 2-month suspension period.
• In other states, such as Indiana, beneficiaries must notify the state
that they have completed 80 hours of work or other qualifying
activities in a calendar month, after which the state will reactivate
eligibility beginning the following month. (See text box.)
Indiana’s Suspension Process for Non-Compliance with Medicaid Work
Requirements
At the end of each year, the state reviews beneficiaries’ activities related to work
requirements. Beneficiaries must meet the required monthly hours 8 out of 12 months of
the year to avoid a suspension of Medicaid coverage.
If coverage is suspended for not meeting work requirements, the suspension will start
January 1 and could last up to 12 months. During a suspension, beneficiaries will not be
able to access Medicaid coverage to receive health care.
Beneficiaries with suspended Medicaid coverage can reactivate coverage if they become
• pregnant;
• medically frail; or
• employed, enrolled in school, or engaged in volunteering.
Beneficiaries must contact the state to reactivate coverage.
Source: GAO summary of Indiana’s “Gateway to Work suspension process” website, accessed June 24, 2019,
https://www.in.gov/fssa/hip/2593.htm. | GAO-20-149.
To prevent suspension from taking effect, two states (Kentucky and New
Hampshire) require beneficiaries to make up required work hours that
were not completed in order to maintain compliance with work
requirements. For example, in Kentucky, if the beneficiary worked 60
hours in October (20 hours less than the required 80), the beneficiary

Page 19 GAO-20-149 Medicaid Demonstration Administrative Costs
must work 100 hours in November to avoid suspension of coverage in
December.
31
Available estimates of the costs to implement Medicaid work
requirements varied considerably among the five selected states, and
these estimates did not account for all costs. These states estimated that
federal funding would cover the majority of these costs, particularly costs
to modify IT systems.
Selected states (Arkansas, Indiana, Kentucky, New Hampshire, and
Wisconsin) reported estimates of the costs to implement work
requirements that ranged from under $10 million in New Hampshire to
over $250 million in Kentucky.
32
These estimates—compiled by states
and reported to us—did not include all planned costs. The estimates were
based on information the states had readily available, such as the costs
of contracted activities for IT systems and beneficiary outreach, and
primarily reflect up-front costs. Four selected states (Arkansas, Indiana,
Kentucky, and New Hampshire) had begun implementing work
requirements and making expenditures by the end of 2018. Together,
these states reported to us having spent more than $129 million in total
31
Kentucky’s vacated approval also allowed beneficiaries to avoid suspension or have
their coverage reactivated if they become suspended if they complete a state-approved
health or financial literacy course—an option that could be used once in a 12-month
period.
32
We collected information from the five states that received approval for demonstrations
with work requirements as of November 2018, which had the most time to implement work
requirements or make significant preparations to do so during the time that we conducted
our review. Kentucky’s and Wisconsin’s estimates include some costs not specific to work
requirements.
Available Estimates of
Costs to Implement
Work Requirements
Varied among
Selected States, with
the Majority of Costs
Expected to Be
Financed by Federal
Dollars
Selected States’ Estimates
of Administrative Costs
Associated with Work
Requirements Ranged
from Millions to Hundreds
of Millions of Dollars

Page 20 GAO-20-149 Medicaid Demonstration Administrative Costs
for implementation activities from the time the states submitted their
demonstration applications through the end of 2018.
33
(See table 3.)
Table 3: Selected States’ Estimates of Administrative Costs and of Initial Expenditures for Implementing Medicaid Work
Requirements
State
Estimated
costs
(dollars in
millions)
Description of estimates of administrative costs and of initial expenditures
Kentucky
271.6
•
Estimate includes $220.9 million in information technology (IT) costs for the Medicaid
demonstration as a whole, including work requirements, for fiscal years 2019 and 2020, and
$50.7 million in payments for managed care organizations’ cost to administer work and other
beneficiary requirements for the period of July 2018 through June 2020.
• Estimate does not include expected costs for evaluating work requirements.
Expenditures from application date (August 2016) through 2018: more than $99.5 million.
a
Wisconsin
69.4
•
Estimate includes $57.3 million for beneficiary outreach, evaluation, and other services from July
2019 through June 2021, and $12.1 million in fiscal year 2019 for IT systems changes for the
Medicaid demonstration as a whole.
Expenditures from application date (January 2018) through 2018: None.
b
Indiana
35.1
•
Estimate includes $14.4 million for IT systems for fiscal years 2018 through 2021, and $20.7
million for managed care organizations’ activities in 2019.
• Estimate does not include expected costs for evaluation.
Expenditures from application date (July 2017) through 2018: more than $800,000.
c
Arkansas
26.1
•
Estimate includes contracts in place from July 2017 through June 2019 for IT systems,
beneficiary outreach, and other activities, such as data analysis.
• Estimate does not include expected costs for beneficiary notices and increased payments to
qualified health plans.
Expenditures from application date (June 2017) through 2018: more than $24.1 million.
d
New
Hampshire
6.1
•
Estimate includes $4.5 million for IT system and other contracts in place from July 2018 through
June 2019, and $1.6 million for evaluation activities from 2019 through 2025.
• Estimate does not include all expected costs, such as increased payments to managed care
organizations.
Expenditures from application date (October 2017) through 2018: more than $4.4 million.
e
Source: GAO analysis of data reported by selected states and selected state documents. | GAO-20-149
Notes: States used standardized data collection instruments to report to GAO their estimated costs
and expenditures to implement work requirements approved under Medicaid section 1115
demonstrations.
a
Kentucky’s expenditures include costs associated with the demonstration as a whole, such as project
management and training costs. These costs do not include payments to managed care
organizations.
33
As with estimated costs, states’ expenditure amounts represented available information
and did not include all expenditures associated with implementing Medicaid work
requirements.
Page 21 GAO-20-149 Medicaid Demonstration Administrative Costs
b
Wisconsin had not begun to implement work requirements by the end of 2018 and so had not made
associated expenditures.
c
Indiana did not include expenditures they could not separately identify, such as expenditures
associated with beneficiary outreach, staff training, demonstration evaluation, and other activities.
d
Arkansas did not include expenditures they could not separately identify, such as expenditures
associated with notices, staff training, qualified health plans’ activities to educate beneficiaries, and
other activities. Arkansas included all expenditures for one contract that expired in March 2019.
e
New Hampshire did not include expenditures they could not separately identify, such as certain
beneficiary outreach expenditures.
Several factors may have contributed to the variation in the selected
states’ estimated costs of administering work requirements, including
planned IT system changes and the number of Medicaid beneficiaries
subject to the work requirements.
IT system changes. Selected states planned distinct approaches to
modify their IT systems in order to administer work requirements. For
example:
• Indiana, which implemented work requirements by expanding on an
existing work referral program, planned to leverage existing IT
systems, making modifications expected to result in IT costs of $14.4
million over 4 years.
• In contrast, Kentucky planned to develop new IT system capabilities
to communicate, track, and verify information related to work
requirements. Kentucky received approval to spend $220.9 million in
fiscal years 2019 and 2020 to do that and make changes needed to
implement other beneficiary requirements in its demonstration.
Number of beneficiaries subject to requirements. The estimated cost
of some activities to administer work requirements depended on the
number of Medicaid beneficiaries subject to work requirements, which
varied across selected states. For example:
• Kentucky estimated 620,000 beneficiaries would be subject to work
requirements—including those who may qualify for exemptions—and
estimated costs of $15 million for fiscal years 2019 and 2020 to
conduct beneficiary education, outreach, and customer service.
• In contrast, Arkansas had fewer beneficiaries subject to work
requirements (about 115,000 in February 2019, with about 100,000 of
those eligible for exemptions) and estimated fewer outreach costs.

Page 22 GAO-20-149 Medicaid Demonstration Administrative Costs
The state estimated $2.9 million in costs from July 2018 through June
2019 to conduct education and outreach.
34
As noted earlier, states’ available estimates did not include all expected
Medicaid costs. For example, four of the five selected states planned to
use MCOs or other health plans to help administer work requirements,
but two of these four did not have estimates of the associated costs.
Indiana and Kentucky estimated additional payments to MCOs—$20.7
million in Indiana to administer work requirements in 2019 and $50.7
million in Kentucky to administer its demonstration from July 2018 through
June 2020. In contrast, officials in New Hampshire told us that no
estimates were available. In Arkansas, where beneficiaries receive
premium support to purchase coverage from qualified health plans on the
state’s health insurance exchange, plans were instructed to include the
costs of administering work requirements in the premiums, according to
Arkansas officials. State officials and representatives from a qualified
health plan we spoke with could not provide the amount that the state’s
premium assistance costs increased as a result.
States’ estimates also did not include all ongoing costs that they expect to
incur after the up-front costs and initial expenditures related to
implementation of the work requirements. States had limited information
about ongoing costs, but we collected some examples. For instance, New
Hampshire provided estimated costs of $1.6 million to design and
implement the evaluation of its demonstration, which all states are
required to perform. In addition, officials or documents in each selected
state acknowledged new staffing costs that may be ongoing, such as
Indiana’s costs for five full-time employees to assist beneficiaries with
suspended coverage to meet requirements or obtain exemptions.
35
Finally, states reported that administering Medicaid work requirements
will increase certain non-Medicaid costs—costs that are not funded by
federal Medicaid, but are borne by other federal and state agencies,
stakeholders, or individuals. For instance, New Hampshire officials
34
Other selected states’ estimates of the number of beneficiaries potentially subject to the
requirements (including those who may qualify for exemptions) were as follows: 420,000
in Indiana; 50,000 in New Hampshire; and 150,000 in Wisconsin, although this included
beneficiaries aged 50 and up who are not subject to work requirements.
35
Another example of new staffing costs that may be ongoing is Kentucky’s estimate of
MCOs’ annual costs of $5.4 million for 270 caseworkers to help identify beneficiaries with
certain medical frailties. These beneficiaries receive 12-month exemptions from work
requirements, mandatory cost sharing, and healthy behavior incentives.

Page 23 GAO-20-149 Medicaid Demonstration Administrative Costs
planned to use approximately $200,000 to $300,000 in non-Medicaid
funds for six positions performing case management for workforce
development. Similarly, in July 2017, Indiana estimated that providing
beneficiaries with job skills training, job search assistance, and other
services would cost $90 per month per beneficiary, although state officials
said these costs were uncertain after learning they were not eligible for
federal Medicaid funds. In addition, beneficiaries and entities other than
states, such as community organizations, may incur costs related to the
administration of work requirements that are not included in states’
estimates.
36
All five selected states expected to receive federal funds for the majority
of estimated costs and expenditures (described previously) for
implementing work requirements.
37
For example, the four selected states
that provided data on expenditures to administer work requirements
through 2018 (Arkansas, Indiana, Kentucky, and New Hampshire)
expected the portion of those expenditures paid by the federal
government to range from 82 percent in Indiana to 90 percent in New
Hampshire and Kentucky.
38
These effective matching rates exceed the 50
percent matching rate for general administrative costs, largely due to
higher matching rates of 75 and 90 percent of applicable IT costs. For
example, Kentucky received approval to spend $192.6 million in federal
funds for its $220.9 million in expected IT costs over 2 years to implement
work requirements and other beneficiary requirements, an effective match
rate of 87 percent.
In addition to higher federal matching rates for IT costs, the selected
states receive federal funds for the majority of MCO capitation payments,
which the states planned to increase to pay MCOs’ costs to administer
36
For example, according to representatives of a stakeholder organization we interviewed,
churches, libraries, and homeless services organizations in Arkansas have dedicated
resources to help beneficiaries comply with work requirements, and beneficiaries spent
time and resources for transportation costs and cellular phone minutes to comply with
work requirements. In addition, we spoke with representatives of a qualified health plan in
Arkansas that serves Medicaid beneficiaries who said that administering work
requirements would increase non-Medicaid members’ premiums.
37
States reported that the federal share of estimated costs would be as follows: Arkansas,
83 percent; Indiana, 86 percent; Kentucky, 87 percent; New Hampshire, 79 percent; and
Wisconsin, 55 percent.
38
The federal share of expenditures reported by Arkansas was 86 percent.
Selected States Estimated
the Federal Government
Would Pay the Majority of
Administrative Costs
Associated with Work
Requirements

Page 24 GAO-20-149 Medicaid Demonstration Administrative Costs
work requirements.
39
Each of the three states that planned to use MCOs
to administer work requirements planned to increase capitation payments
in order to do so. For example, Indiana planned to increase capitation
payments to MCOs by approximately 1 percent (or $20.7 million in 2019)
to pay for a variety of ongoing activities to administer work requirements,
including requiring MCOs to help beneficiaries report compliance,
reporting beneficiaries who qualify for exemptions, and helping the state
verify the accuracy of beneficiary reporting, according to state officials.
The federal government pays at least 90 percent of capitation payments
to MCOs to provide covered services to beneficiaries who are newly
eligible under PPACA, the primary population subject to work
requirements among the five selected states.
40
Indiana and Kentucky also
received approval to apply work requirements to other populations, and
capitation payments for these other populations receive federal matching
rates of 66 percent in Indiana and 72 percent in Kentucky in fiscal year
2019.
States’ approaches to implementing work requirements can affect the
federal matching funds they receive. For example, Arkansas officials told
us that the state decided to collect information on beneficiary compliance
through an on-line portal—the initial cost of which received an effective
federal matching rate of 87 percent, according to Arkansas. Officials told
us that the state avoided having beneficiaries report compliance to staff—
costs of which receive a 75 percent matching rate.
41
However, after
approximately 17,000 beneficiaries lost coverage due to non-compliance
with work requirements, Arkansas revised its procedures to allow
beneficiaries to report compliance to state staff over the phone.
Three of the five selected states sought to leverage other programs
funded by the federal government to help implement work requirements
39
Capitation payments provide MCOs a set payment per beneficiary to provide a specific
set of Medicaid-covered services to Medicaid beneficiaries.
40
Specifically, states will receive a 93 percent federal matching rate for medical assistance
costs for newly eligible beneficiaries in fiscal year 2019, and 90 percent thereafter. States
receive this federal matching rate for the non-benefit portion of MCO capitation payments
if states transfer the financial risk associated Medicaid beneficiaries to the MCO. In
addition, Arkansas receives this federal matching rate for premiums to qualified health
plans for these beneficiaries.
41
Costs for developing the IT systems may be eligible for a 90 percent federal match rate
and 75 percent match rate for ongoing maintenance and operation, including staffing
costs.

Page 25 GAO-20-149 Medicaid Demonstration Administrative Costs
or provide beneficiary supports, such as employment services. Kentucky
officials reported piloting elements of Medicaid work requirements using
its SNAP Employment and Training program. Similarly, Arkansas officials
sought a waiver to be able to use TANF funds to provide employment
services to individuals without children in order to serve Medicaid
beneficiaries subject to work requirements.
42
New Hampshire also used
TANF funds to provide employment services to Medicaid beneficiaries
who were also enrolled in TANF.
CMS does not consider administrative costs when approving any
demonstrations—including those with work requirements—though these
costs can be significant. The agency has recently taken steps to obtain
more information about demonstration administrative costs. However, we
identified various weaknesses in CMS’s oversight of administrative costs
that could result in states receiving federal funds for costs to administer
work requirements that are not allowable.
CMS’s demonstration approval process does not take into account the
extent to which demonstrations, including those establishing work
requirements, will increase a state’s administrative costs. CMS policy
does not require states to provide projections of administrative costs in
their demonstration applications or include administrative costs in their
demonstration cost projections used by CMS to assess budget neutrality.
CMS officials explained that in the past demonstrations had generally not
led to increases in administrative costs, and as such, the agency had not
seen a need to separately consider these costs.
However, the officials told us and have acknowledged in approval letters
for demonstrations with work requirements, that demonstrations may
increase administrative costs. Kentucky provides an example of this,
reporting to us estimated administrative costs of approximately $270
million—including about $200 million in federal funds—to implement the
demonstration over 2 years. However, neither Kentucky nor the other four
selected states provided estimates of their administrative costs in their
applications to CMS, and CMS officials confirmed that no additional
42
As of June 2019, information on the status of this waiver application was not available
from the Arkansas officials we spoke with.
Weaknesses Exist in
CMS’s Oversight of
Administrative Costs
of Demonstrations
with Work
Requirements
CMS’s Approval Process
Does Not Take into
Account How a
Demonstration Will Affect
Administrative Costs

Page 26 GAO-20-149 Medicaid Demonstration Administrative Costs
information on administrative costs was provided by the states while their
demonstration applications were being reviewed.
By not considering administrative costs in its demonstration approval
process, CMS’s actions are counter to two key objectives of the
demonstration approval process: transparency and budget neutrality.
• Transparency. CMS’s transparency requirements are aimed at
ensuring that demonstration proposals provide sufficient information
to ensure meaningful public input. However, CMS officials told us that
they do not require the information states provide on the expected
changes in demonstration expenditures in their applications to
account for administrative costs. This information would likely have
been of interest in our selected states, because public commenters in
each state expressed concerns about the potential administrative
costs of these demonstrations. In prior work, we reported on
weaknesses in CMS’s policies for ensuring transparency in
demonstration approvals.
43
• Budget neutrality. The aim of CMS’s budget neutrality policy is to
limit federal fiscal liability resulting from demonstrations, and CMS is
responsible for determining that a demonstration will not increase
federal Medicaid expenditures above what they would have been
without the demonstration. However, CMS does not consider
administrative costs when assessing budget neutrality. For three of
our five selected states, the demonstration special terms and
conditions specify that administrative costs will not be counted against
the budget neutrality limit.
Even though demonstrations’ administrative costs can be significant,
CMS officials said the agency has no plans to revise its approval
process—either to (1) require states to provide information on expected
administrative costs to CMS or the public, or to (2) account for these
costs when the agency assesses whether a demonstration is budget
neutral. CMS officials explained that the agency needs more experience
43
In 2019, we reported that CMS’s approach to ensuring public transparency had
weaknesses when states proposed making major changes to their demonstrations
through amendments or major changes to pending applications. For example, we found
that enrollment information was not disclosed when Arkansas and New Hampshire each
sought to amend their demonstrations to add a work requirement. We made
recommendations, with which CMS concurred, for the agency to develop policies to
improve transparency when states propose major changes. See GAO, Medicaid
Demonstrations: Approvals of Major Changes Need Increased Transparency,
GAO-19-315 (Washington, D.C.: Apr. 17, 2019).

Page 27 GAO-20-149 Medicaid Demonstration Administrative Costs
with policies that require administrative changes under a demonstration
before making any revisions to its processes. Without requiring states to
submit projections of administrative costs in their demonstration
applications, and by not considering the implications of these costs for
federal spending, CMS puts its goals of transparency and budget
neutrality at risk. This is inconsistent with federal internal control
standards that call for agencies to identify, analyze, and respond to risks
related to achieving program objectives.
44
CMS recently implemented procedures that may provide additional
information on demonstrations’ administrative costs. These included
implementing new procedures to identify costs specific to demonstrations
when approving federal matching funds for states’ planned IT costs and
issuing guidance on monitoring and evaluating demonstrations. However,
it is unclear whether these efforts will result in data that improve CMS’s
oversight. (See table 4.)
Table 4: CMS Initiatives that May Provide the Agency with Information on Demonstration Administrative Costs
CMS initiative
Description and limitations
New procedures for IT
funding approvals
Description: CMS officials told us that in 2018 the agency began requiring states to identify funding
amounts specific to demonstrations in their information technology (IT) funding requests.
Limitations:
• CMS has not consistently applied this requirement. For example, Arkansas did not identify in its IT
funding request the amounts specific to its demonstration, which the state reported to us exceeded
$20 million; however, in February 2019 CMS approved the request without this information.
• How states decide which IT costs are associated with their demonstrations is unclear. CMS officials
said that states work with CMS analysts on their requests, but otherwise the agency had not
provided guidance to states on how to break out these costs.
New monitoring guidance
Description: In March 2019, CMS issued guidance recommending that states implementing work
requirements and other changes to eligibility and coverage annually report on trends in their
demonstrations’ administrative costs, including explaining increases or decreases in costs of greater
than 2 percent.
Limitation: Annual reporting is recommended, but not required.
44
See GAO-14-704G.
CMS Has Taken Steps to
Collect New Information
on Administrative Costs,
yet Risks May Remain of
CMS Providing Federal
Funds for Work
Requirement Costs that
Are Not Allowable

Page 28 GAO-20-149 Medicaid Demonstration Administrative Costs
CMS initiative
Description and limitations
New evaluation guidance
Description: In March 2019, CMS issued guidance directing states implementing work requirements
and other changes to eligibility and coverage to evaluate the effects of the policy on the sustainability of
the Medicaid program, which includes determining demonstration startup and ongoing administrative
costs.
Limitation: Evaluation findings for demonstrations with work requirements will not be available for
several years, with the first evaluation report due in Indiana in June 2022.
Source: GAO analysis of information from the Centers for Medicare & Medicaid Services (CMS). | GAO-20-149
In addition to these new initiatives, states’ quarterly expenditure reports
provide CMS with some information on their demonstration administrative
costs, but this information also has limitations. States are required to
separately track and report administrative expenditures attributable to
their demonstrations in their quarterly expenditure reports. However, CMS
officials told us that states typically use the same resources, such as staff,
to administer their demonstrations and their regular Medicaid program,
which can affect the demonstration costs states report. We found that
about a quarter of states with demonstration expenditures in fiscal year
2017 reported no administrative expenditures related to their
demonstrations. CMS officials acknowledged that the data states submit
in their quarterly expenditure reports may not provide a meaningful
measure of states’ demonstration-related administrative costs.
45
CMS’s recently implemented procedures may provide more information
on the amounts states are spending on demonstration administrative
costs, but they do not address weaknesses we found in CMS’s oversight
of administrative costs. In four of the five selected states, we identified
examples of states requesting federal matching funds for costs to
administer work requirements that do not appear to be allowable, or at
higher matching rates than appropriate under CMS guidance. In some
cases, states received CMS approval for planned administrative costs
while in others it was unclear whether CMS would have identified the
issues through their oversight procedures. Areas of risk included funds for
45
In the past, we reported on CMS’s oversight of demonstration spending and found that
states were not always complying with reporting requirements for demonstration
expenditures, and CMS was not consistently enforcing these requirements. For example,
CMS did not consistently require selected states to report the information needed to
assess compliance with demonstration spending limits. We recommended that CMS
develop standard operating procedures for sufficient reporting requirements and to require
consistent monitoring. HHS agreed with this recommendation and in 2018 reported that
the agency had developed draft guidance, including a standard reporting tool for states, to
better ensure consistent reporting of the elements needed to assess compliance with
demonstration spending limits. See GAO, Medicaid Demonstrations: Federal Action
Needed to Improve Oversight of Spending, GAO-17-312 (Washington, D.C.: Apr. 3, 2017).
Page 29 GAO-20-149 Medicaid Demonstration Administrative Costs
planned IT costs, funds for beneficiary supports, and funds provided
under managed care contracts.
Federal funds for planned IT costs that may not be allowable or
eligible for higher matching rates. Three of our five selected states
requested and received funding approval for planned IT costs to
implement their demonstrations that did not appear to be allowable or at
higher matching rates than appropriate under CMS guidance.
46
• Kentucky and Indiana requested and received funding approval for
planned IT costs that do not appear to be allowable under CMS
guidance.
47
Kentucky requested and received CMS approval for funds
(at the 90 percent federal matching rate) for a contract that included
activities to assist Medicaid beneficiaries obtain employment. (See
text box.) However, CMS’s 2018 guidance states that Medicaid
funding is not available to finance beneficiary supports, such as job
training or other employment services.
48
CMS officials said that the
agency did not review the contract and approved the request based
on Kentucky’s assertion that these costs were specific to technology.
Indiana received approval to receive IT funds to develop a website
that provides beneficiaries access to information and tools to seek,
acquire, and retain employment, costs that also appear related to
beneficiary supports.
49
46
An evaluation of whether states received federal funds under these approvals and the
extent to which the underlying costs complied with relevant statutes and regulations
regarding allowable federal expenditures and appropriate matching rates was outside the
scope of our review. We are referring these matters to the HHS Office of Inspector
General for review and any action deemed appropriate.
47
To request federal funds for state planned IT activities, states prepare and submit
advance planning documents to CMS. Advance planning documents include preliminary
cost estimates for the activities that states plan to undertake. According to CMS officials,
the amounts approved in states’ advance planning documents serve as a limit on the
amounts states can ultimately spend on IT costs.
48
In its guidance, CMS indicates that states will be required, as part of their demonstration
applications, to describe strategies to assist beneficiaries in meeting work requirements
and to link beneficiaries to additional resources, such as job training or other employment
services, which are broadly described as beneficiary supports. The guidance clarifies that,
despite that expectation, CMS will not provide authority to use Medicaid funds to finance
those services. See CMS, SMD: 18-002.
49
In June 2019, CMS officials told us that the agency’s view is that the costs in Indiana as
well as Kentucky were allowable on the basis that the activities enabled systems
development. We are including CMS’s position in our referral to the HHS Office of
Inspector General.

Page 30 GAO-20-149 Medicaid Demonstration Administrative Costs
Kentucky Received Approval of Information Technology Funding for Activities
Aimed at Helping Beneficiaries Obtain Employment
In 2018, in an update to its information technology budget request, Kentucky included
costs for a contract with the state’s Department of Workforce Services to assist Medicaid
beneficiaries in developing skills needed to obtain and retain employment. The
contracted services included activities such as
• assessing beneficiaries’ eligibility for non-Medicaid programs,
• providing services to beneficiaries at career assistance centers, and
• making referrals to other agencies and programs.
Kentucky budgeted $21 million for this contract at a 90 percent federal matching rate
($18.9 million in federal funds) for fiscal year 2019 and another $21 million at a 75
percent matching rate ($15.8 million in federal funds) for fiscal year 2020. CMS approved
Kentucky’s budget request without reviewing the contract.
Source: GAO analysis of documentation from the Centers for Medicare & Medicaid Services (CMS) and Kentucky Department for
Medicaid Services. | GAO-20-149.
• Indiana and New Hampshire received funding approval for federal IT
funds at the 90 percent matching rate for costs that do not appear
eligible for that rate. In 2018, CMS approved Indiana’s request for a
90 percent match rate to pay $500,000 in consulting fees to develop
work requirement policies, despite CMS guidance indicating that
policy research and development activities should be matched at 50
percent.
50
New Hampshire requested and received CMS approval in
2018 for federal funds at a 90 percent matching rate for $180,000 in
costs to educate beneficiaries about work requirements, including
costs to place outreach calls through an existing contracted call
50
CMS’s guidance related to funding for IT systems details activities eligible for enhanced
matching rates and also includes a list of activities that are to receive a 50 percent match
rate. That list includes the costs for policy research and development. See CMS, State
Medicaid Director Letter, Re: Mechanized Claims Processing and Information Retrieval
Systems-Enhanced Funding, SMD: 16-004 (Baltimore, Md.: Mar. 31, 2016).
In June 2019, CMS officials told us that it is the agency’s view that the 90 percent match
rate approved was appropriate because Indiana’s policy development activities affected IT
systems development. We are including CMS’s position in our referral to the HHS Office
of Inspector General.

Page 31 GAO-20-149 Medicaid Demonstration Administrative Costs
center.
51
CMS guidance indicates that these costs should receive
funding at a lower matching rate.
52
Federal funds for beneficiary supports that are not allowable.
Wisconsin requested and planned to seek federal funds for beneficiary
support costs that are not allowable until our work identified the issue for
CMS. Wisconsin officials told us that it was their understanding during the
planning phase of the demonstration that administrative costs incurred by
state programs providing such services were eligible for federal matching
funds. State officials said that CMS officials told them on multiple
occasions that the state could receive a 50 percent federal match for
these costs. Based on this, the state requested budget authority from its
legislature for $51.2 million for employment and training services, of
which it anticipated $23.1 million would come from federal Medicaid
funds. CMS officials told us that such costs are not eligible for federal
matching funds and maintained that the agency’s guidance—which
indicates that beneficiary support costs are not eligible for federal
51
The state’s contract with the vendor administering the call center describes over 50,000
calls to be conducted in four phases: an initial outreach call to those subject to the
requirement (i.e., mandatory population) who are not in another work program, a second
call to the frail population urging them to apply for an exemption, a call to the mandatory
population to remind them to report hours, and a call to non-compliant members “urging”
them to take steps to prevent suspension.
52
According to CMS guidance, call center activities related to general beneficiary
education, among other topics, can receive a 50 percent federal matching rate, and call
center activities related to the receipt of data required for eligibility determination or on-
going case maintenance can receive a 75 percent match. See CMS, SMD: 16-004.
In June 2019, CMS officials told us that the 90 percent matching rate approved for the
New Hampshire request was appropriate because the state was developing and testing
call center functionality, which is a development cost. We are including CMS’s position in
our referral to the HHS Office of Inspector General.

Page 32 GAO-20-149 Medicaid Demonstration Administrative Costs
matching funds—was clear.
53
In response to our inquiries, the agency
contacted the state in April 2019 and clarified this with officials.
54
Federal funds for costs to administer work requirements provided
through managed care contracts, which may not be allowable. As
noted earlier, three of the five selected states (Indiana, Kentucky, and
New Hampshire) required or planned to require MCOs to perform a
number of activities to implement work requirements.
55
These activities
included, for example, providing information on options to satisfy work
requirements, assisting beneficiaries with reporting compliance with work
requirements, and providing referrals to state work requirement
resources. To fund these activities, officials in these states said that they
plan to increase their capitation payments. States will receive at least a
90 percent federal matching rate for most of these payments, because
the payments are largely for beneficiaries who are newly eligible under
PPACA. It is unclear, however, whether including these activities in
capitation payments is allowable. CMS regulations provide that states
may only include administrative costs that are related to the provision of
covered health care services in their MCO capitation payments.
56
In
addition, CMS guidance notes that implementing work requirements will
not change the types of expenditures that are allowable. We provided
CMS with specific examples of activities states delegated or planned to
delegate to MCOs and asked if these types of activities met CMS’s
53
See CMS, SMD: 18-002.
54
CMS officials also noted that Wisconsin’s reported administrative expenditures would be
subject to CMS review and the state would only receive federal matching funds for
allowable expenditures. However, in past work, we found that CMS was not sufficiently
targeting risk in its oversight of Medicaid expenditures, potentially allowing errors—
including for expenditures that are not allowable—to go undetected. We recommended
that CMS improve its risk-based targeting of oversight efforts and resources. CMS agreed
with this recommendation and planned to complete a national risk assessment and
identify opportunities to increase resources and determine the appropriate allocation of
staff. See GAO, Medicaid: CMS Needs to Better Target Risks to Improve Oversight of
Expenditures, GAO-18-564 (Washington, D.C.: Aug. 6, 2018).
55
In addition, Arkansas is relying on qualified health plans to perform activities to
administer work requirements in its demonstration. For example, according to officials
from one qualified health plan, the plan sent 270,000 letters to beneficiaries at a cost of
$25,000 and issued $30 rewards cards to 600 beneficiaries for attesting to meeting work
requirements for three consecutive months.
56
42 C.F.R. § 438.3(c)(1)(ii) (2018)

Page 33 GAO-20-149 Medicaid Demonstration Administrative Costs
criteria to be included under capitation payments.
57
CMS officials told us
that federal review of the related managed care contracts in Indiana and
New Hampshire had not been completed as of June 2019 and could not
make a definitive statement.
58
While CMS guidance requires states to carry out a range of activities to
implement work requirements—some of which are not eligible for federal
Medicaid funds—agency officials told us that CMS has not updated any
procedures for the various reviewers of these costs. Further, CMS has
not completed a risk assessment to determine whether current
procedures for overseeing administrative costs are sufficient, and agency
officials told us that there were no plans to do so.
59
According to federal
internal control standards, agencies should identify, analyze, and respond
to risks related to achieving program objectives (in this case, ensuring
that administrative expenditures under demonstrations are allowable and
matched at the correct rate).
60
Without identifying, assessing, and
addressing the risks posed by demonstrations that may increase
administrative costs, CMS may be providing federal funds for costs that
are not allowed or at inappropriately high matching rates.
57
States are required to submit managed care contracts and capitation rates to CMS for
review and approval.
58
Although CMS officials could not comment on specific examples, in general, they said
certain types of MCO activities could be allowable, such as training customer service staff
about work requirements. With regard to MCOs helping beneficiaries report compliance
with work requirements, CMS officials cited 42 C.F.R § 438.608(a)(3), which requires
MCOs to promptly notify the state when it receives information about a beneficiary’s
circumstances that may affect eligibility, such as a change in residence or death. In July
2019, CMS approved Kentucky’s contracts with MCOs for the period July 2018 through
June 2019 and related capitation rates for July 2018 through March 2019. These rates
included a $17 million overall increase for MCOs’ costs to administer the demonstration.
According to officials, CMS approved this rate increase for MCOs’ costs to prepare to
meet new requirements under the demonstration and to notify beneficiaries of new
requirements. Officials said that CMS’s approval did not address the use of federal funds
for other MCO activities to administer work requirements that were outlined in the contract,
such as referring beneficiaries to resources related to work requirements, so it remains
unclear whether capitation payments for those costs are allowable.
59
CMS officials said that the agency had no plans to conduct a risk assessment of its
oversight procedures until it gained more experience with work requirement policies to
determine if any mid-course correction is needed.
60
See GAO-14-704G.

Page 34 GAO-20-149 Medicaid Demonstration Administrative Costs
A third of states have sought approval to implement work requirements in
their Medicaid programs. CMS has acknowledged that demonstrations,
including those with work requirements, may increase Medicaid
administrative costs—and therefore overall Medicaid spending. Yet, CMS
is not factoring these costs into its approval decisions, which is counter to
the agency’s goals of transparency and budget neutrality. Further, the
agency has not taken steps to assess and respond to risks of federal
funds being spent for administrative costs that are not allowable or
matched at rates higher than what is appropriate, risks we found in four of
the five demonstrations we reviewed. While administrative costs are a
relatively small portion of states’ Medicaid spending, the weaknesses in
CMS’s oversight of these costs could take on increased importance as
more states seek and receive approval to implement work requirements.
We are making the following three recommendations to CMS:
The Administrator of CMS should require states to submit and make
public projections of administrative costs when seeking approval of
demonstrations, including those with work requirements and all other
demonstrations. (Recommendation 1)
The Administrator of CMS should account for the administrative costs of
demonstrations, including those with work requirements and all other
demonstrations, when assessing whether demonstrations are budget
neutral. (Recommendation 2)
The Administrator of CMS should assess the risks of providing federal
funds for costs to administer work requirements that are not allowable
and should respond to risks by improving oversight procedures, as
warranted. This assessment should consider risks related to costs for
information systems, beneficiary supports, and managed care.
(Recommendation 3)
We provided a draft of this report to HHS for comments and its comments
are reproduced in appendix II. HHS also provided us with technical
comments, which we incorporated in the report as appropriate. HHS did
not concur with our recommendations. In general, HHS commented that it
expects administrative costs to represent a relatively small proportion of
total Medicaid spending and that its current approach to overseeing
administrative costs—including those incurred under Medicaid
demonstrations—is appropriate given the level of financial risk. HHS
Conclusions
Recommendation for
Executive Action
Agency Comments
and Our Evaluation

Page 35 GAO-20-149 Medicaid Demonstration Administrative Costs
commented that administrative costs were approximately 5 percent of
Medicaid expenditures. While these cost may represent a relatively small
share of total spending, CMS projected them to be $18 billion in federal
funds in fiscal year 2019—and this does not include all administrative
spending. In particular, it does not include amounts paid to MCOs for
administrative costs, which are likely considerable given that managed
care payments now represent about half of all Medicaid spending.
Further, demonstrations may represent a heightened financial risk given
our finding that they can result in additional administrative costs that
would not otherwise occur.
Regarding our first recommendation to require states to submit and make
public projections of administrative costs, HHS commented that its
experience suggests that demonstration administrative costs will be a
relatively small portion of total costs and therefore HHS believes making
information about these costs available would provide stakeholders little
to no value. As noted, Medicaid is a significant component of federal and
state budgets. In each of the five states we reviewed, public commenters
expressed concerns about the potential administrative costs of Medicaid
demonstrations with work requirements, suggesting stakeholders would
value information about these costs. We maintain that requiring states to
make public information about administrative costs would help to ensure
that demonstration proposals provide sufficient information to ensure
meaningful public input.
Regarding our second recommendation to account for administrative
costs when assessing whether demonstrations are budget neutral, HHS
again commented that its experience suggests that demonstration
administrative costs will be a relatively small portion of total costs and that
it believed that its current approach is appropriate for the level of financial
risk. However, we found that demonstration administrative costs could be
significant and HHS’s current policy of not considering these costs in its
assessments of budget neutrality could increase federal fiscal liability. For
example, in Kentucky, we found estimated administrative costs for
implementing the demonstration exceeded $270 million over about 2
years. We maintain that including administrative costs in its assessments
will help HHS ensure that demonstrations are budget neutral.
Regarding our third recommendation to assess and respond to risks of
providing federal funds for costs to administer work requirements that are
not allowable, HHS commented that (1) all states’ requests for federal
Medicaid funding are subject to the same federal regulations and
requirements; (2) the expenditures reported by states to GAO had not

Page 36 GAO-20-149 Medicaid Demonstration Administrative Costs
been reviewed against federal requirements or certified by states to be
accurate and permissible; and (3) HHS believes its existing approach is
appropriate for the low level of risk that administrative expenditures
represent. Our findings indicate that CMS’s oversight procedures—which
are designed to prevent state spending on costs that do not meet federal
requirements—have vulnerabilities, particularly given the types of
administrative activities associated with work requirements. Four of the
five states we reviewed were planning to seek federal funds for costs (1)
that did not appear allowable, or (2) at higher matching rates than appear
appropriate, and three states succeeded in gaining CMS approval to do
so. We agree with HHS that CMS may also identify inappropriate
expenditures during its reviews of state-reported expenditures. However,
our past work has identified weaknesses in that review process.
61
In
2018, we reported that CMS officials indicated that resource constraints
have limited the agency’s ability to target risk during such reviews,
potentially allowing errors to go undetected. Finally, the basis for HHS’s
conclusion that its current approach is appropriate for the risks posed by
these administrative expenditures is unclear. As we note in our report,
CMS officials told us that they had not assessed whether current
procedures sufficiently address risks posed by administrative costs for
work requirements and had no plans to do so. We maintain that
assessing these risks of providing federal funds for costs that are not
allowable and improving oversight, as warranted, would help HHS to
ensure the integrity of the Medicaid program.
As agreed with your offices, unless you publicly announce the contents of
this report earlier, we plan no further distribution until 30 days from the
report date. At that time, we will send copies of this report to the
Secretary of Health and Human Services, the appropriate congressional
committees, and other interested parties. In addition, this report is
available at no charge on the GAO website at http://www.gao.gov.
61
See GAO-18-564.

Page 37 GAO-20-149 Medicaid Demonstration Administrative Costs
If you or your staff members have any questions about this report, please
contact me at (202) 512-7144 or [email protected]. Contact points for our
Offices of Congressional Relations and Public Affairs may be found on
the last page of this report. Major contributors to this report are listed in
appendix III.
Carolyn L. Yocom
Director, Health Care

Appendix I: Other Beneficiary Requirements in
States with Approved Medicaid Work
Requirements
Page 38 GAO-20-149 Medicaid Demonstration Administrative Costs
Eight of the nine states that received approval for work requirements, as
of May 2019, also received approval under their demonstrations for other
beneficiary requirements, such as requiring beneficiaries to have
expenditure accounts.
1
Some of these beneficiary requirements preceded
work requirements, while others were newly introduced with the work
requirements. For example, Kentucky was developing and implementing
work requirements at the same time as other beneficiary requirements,
such as the requirement for beneficiaries to have two expenditure
accounts and make premium payments. (See table 5.)
Table 5: Other Beneficiary Requirements in States with Approved Medicaid Work Requirements, as of May 2019
State
Premium
payments
Beneficiary
expenditure
accounts
a
Reductions to
retroactive
eligibility
b
Non-eligibility
periods for non-
compliance
c
Healthy behavior
incentives
d
Arizona
✓
✓
✓
—
✓
Arkansas
✓
—
✓
✓
—
Indiana
✓
✓
✓
✓
✓
Kentucky
✓
✓
✓
✓
✓
Michigan
✓
✓
—
✓
✓
New Hampshire
—
—
✓
—
—
Ohio
—
—
—
—
—
Utah
✓
—
✓
—
—
Wisconsin
✓
—
—
✓
✓
Legend:
✓ = yes
— = not applicable
Source: Centers for Medicare & Medicaid Services (CMS) documentation. | GAO-20-149
Note: The U.S. District Court for the District of Columbia vacated CMS’s approvals of demonstrations
in Arkansas and Kentucky in March 2019, and in New Hampshire in July 2019. Gresham v. Azar, 363
F. Supp. 3d 165 (D.D.C. 2019); Stewart v. Azar, 366 F. Supp. 3d 125 (D.D.C. 2019); Philbrick v. Azar,
No. 19-773 (JEB) (D.D.C. July 29, 2019).
a
Beneficiary expenditure accounts are similar to health savings accounts where funds are used to pay
for health care expenses. In some states, beneficiary premium payments are credited to these
accounts.
b
Unless waived under section 1115(a), states are required to provide Medicaid coverage to enrollees
beginning 3 months prior to the month of their Medicaid application if the individual would have been
eligible during this time.
1
Beneficiary expenditure accounts are similar to health savings accounts where funds are
used to pay for health care expenses. Healthy behavior incentives can be direct financial
incentives (e.g., reduced or increased cost-sharing requirements) or additional health care
coverage for services that encourage beneficiaries to use certain health services, such as
primary care; participate in certain activities, such as consuming a healthy diet or
increasing physical activity; or cease unhealthy activities, such as smoking.
Appendix I: Other Beneficiary Requirements
in States with Approved Medicaid Work
Requirements

Appendix I: Other Beneficiary Requirements in
States with Approved Medicaid Work
Requirements
Page 39 GAO-20-149 Medicaid Demonstration Administrative Costs
c
A non-eligibility period is the length of time a beneficiary is restricted from reenrolling in the program
following a coverage termination due to noncompliance with certain beneficiary requirements.
d
Healthy behavior incentives can be direct financial incentives (e.g., reduced or increased cost-
sharing requirements) or additional health care coverage for services that encourage beneficiaries to
use certain health services, such as primary care; participate in certain activities, such as consuming
a healthy diet or increasing physical activity; or cease unhealthy activities, such as smoking.

Appendix II: Comments from the Department
of Health and Human Services
Page 40 GAO-20-149 Medicaid Demonstration Administrative Costs
Appendix II: Comments from the Department
of Health and Human Services
Appendix II: Comments from the Department
of Health and Human Services
Page 41 GAO-20-149 Medicaid Demonstration Administrative Costs
Appendix II: Comments from the Department
of Health and Human Services
Page 42 GAO-20-149 Medicaid Demonstration Administrative Costs

Appendix II: Comments from the Department
of Health and Human Services
Page 43 GAO-20-149 Medicaid Demonstration Administrative Costs

Appendix III: GAO Contact and Staff
Acknowledgments
Page 44 GAO-20-149 Medicaid Demonstration Administrative Costs
Carolyn L. Yocom, (202) 512-7114 or [email protected]
In addition to the contact named above, Susan Barnidge (Assistant
Director), Russell Voth (Analyst in Charge), Linda McIver, and Matt
Nattinger made key contributions to this report. Also contributing were
Giselle Hicks, Drew Long, Ethiene Salgado-Rodriguez, and Emily Wilson
Schwark.
Appendix III: GAO Contact and Staff
Acknowledgments
GAO Contact
Staff
Acknowledgments

Related GAO Reports
Page 45 GAO-20-149 Medicaid Demonstration Administrative Costs
Medicaid Demonstrations: Approvals of Major Changes Need Increased
Transparency. GAO-19-315. Washington, D.C.: April 17, 2019.
Medicaid: CMS Needs to Better Target Risks to Improve Oversight of
Expenditures. GAO-18-564. Washington, D.C.: August 6, 2018.
Medicaid Demonstrations: Evaluations Yielded Limited Results,
Underscoring Need for Changes to Federal Policies and Procedures.
GAO-18-220. Washington, D.C.: January 19, 2018.
Medicaid Demonstrations: Federal Action Needed to Improve Oversight
of Spending. GAO-17-312. Washington, D.C.: April 3, 2017.
Medicaid: Federal Funds Aid Eligibility IT System Changes, but
Implementation Challenges Persist. GAO-15-169. Washington, D.C.:
December 12, 2014.
Medicaid Demonstration Waivers: Approval Process Raises Cost
Concerns and Lacks Transparency. GAO-13-384. Washington, D.C.:
June 25, 2013.
Medicaid Demonstration Waivers: Recent HHS Approvals Continue to
Raise Cost and Oversight Concerns. GAO-08-87. Washington, D.C.:
January 31, 2008.
Related GAO Reports
(102982)

The Government Accountability Office, the audit, evaluation, and investigative
arm of Congress, exists to support Congress in meeting its constitutional
responsibilities and to help improve the performance and accountability of the
federal government for the American people. GAO examines the use of public
funds; evaluates federal programs and policies; and provides analyses,
recommendations, and other assistance to help Congress make informed
oversight, policy, and funding decisions. GAO’s commitment to good government
is reflected in its core values of accountability, integrity, and reliability.
The fastest and easiest way to obtain copies of GAO documents at no cost is
through GAO’s website (https://www.gao.gov). Each weekday afternoon, GAO
posts on its website newly released reports, testimony, and correspondence. To
have GAO e-mail you a list of newly posted products, go to https://www.gao.gov
and select “E-mail Updates.”
The price of each GAO publication reflects GAO’s actual cost of production and
distribution and depends on the number of pages in the publication and whether
the publication is printed in color or black and white. Pricing and ordering
information is posted on GAO’s website, https://www.gao.gov/ordering.htm.
Place orders by calling (202) 512-6000, toll free (866) 801-7077, or
TDD (202) 512-2537.
Orders may be paid for using American Express, Discover Card, MasterCard,
Visa, check, or money order. Call for additional information.
Connect with GAO on Facebook, Flickr, Twitter, and YouTube.
Subscribe to our RSS Feeds or E-mail Updates. Listen to our Podcasts.
Visit GAO on the web at https://www.gao.gov.
Contact FraudNet:
Website: https://www.gao.gov/fraudnet/fraudnet.htm
Automated answering system: (800) 424-5454 or (202) 512-7700
Orice Williams Brown, Managing Director, WilliamsO@gao.gov, (202) 512-4400,
U.S. Government Accountability Office, 441 G Street NW, Room 7125,
Washington, DC 20548
Chuck Young, Managing Director, youngc1@gao.gov, (202) 512-4800
U.S. Government Accountability Office, 441 G Street NW, Room 7149
Washington, DC 20548
James-Christian Blockwood, Managing Director, spe[email protected]ov, (202) 512-4707
U.S. Government Accountability Office, 441 G Street NW, Room 7814,
Washington, DC 20548
GAO’s Mission
Obtaining Copies of
GAO Reports and
Testimony
Order by Phone
Connect with GAO
To Report Fraud,
Waste, and Abuse in
Federal Programs
Congressional
Relations
Public Affairs
Strategic Planning and
External Liaison
Please Print on Recycled Paper.
