
1
Whole Health System Approach
to Long COVID
Patient-Aligned Care Team (PACT) Guide
U.S. Department of Veterans Affairs
August 1, 2022

2
EXECUTIVE SUMMARY
The U.S. Department of Veterans Affairs (VA) Veterans Health Administration (VHA) is leading an effort to
equip health care providers with a Veteran-centered Whole Health System approach to caring for Veterans
with Long COVID, also known as post-COVID-19 conditions (PCC). Whole Health is an evidence-informed,
multi-disciplinary, personalized, Veteran-driven approach that empowers and equips Veterans to take charge
of their health and well-being, and to live life to the fullest.
Organizations across the world have defined Long COVID with differing parameters. Diagnosing and defining
Long COVID is complicated as there are many signs, symptoms, and conditions that are associated with the
syndrome. Additionally, it is important to separate three things: pre-existing symptoms or conditions, those
that have worsened, and those that are new since an initial COVID-19 diagnosis. Risk factors for developing
Long COVID signs and symptoms include female sex (Pelà G, 2022) (Fernández-de-Las-Peñas C, 2022)
,
respiratory symptoms at the onset, and the severity of the illness (Asadi-Pooya AA, 2021). At the time of this
writing, it is estimated that 4-7% of those diagnosed with COVID-19, or 2% of the U.S. population, will develop
Long COVID (Xie Y, 2021)
. Based on approximately 600,000 known Veterans with a diagnosis of COVID-19,
this equates to 24,000-42,000 Veterans. However, these numbers have the potential to be much higher, as
the VA has more than 6 million Veterans in care.
VA’s Office of Research and Development, the Long COVID Community of Practice, and the Long COVID
Integrated Project Team are working to organize, support, and report on the development of a national
program to help all Veterans who have Long COVID. They collaborated to produce this document for health
care providers to better facilitate defining, assessing, referring, and managing common Long COVID signs,
symptoms, and potential subsequent conditions using a Whole Health System approach. It is not intended to
replace clinical judgment. Rather, it provides suggestions for health care providers as they engage in shared
health care decision-making with Veterans who have this syndrome. The information available on Long
COVID is ever changing. This document will be periodically updated and republished as the scientific
community learns more about Long COVID.
Definition of Long COVID, Post-COVID-19 Conditions and Post-Acute
Sequalae of SARS-CoV-2 Infection
As mentioned above, organizations have defined Long COVID with differing parameters. The Centers for
Disease Control and Prevention (CDC) and National Institutes of Health (NIH) define Long COVID as “new or
worsening symptoms” from “4 weeks after first being infected” with COVID-19. According to the CDC, the
term “post-COVID conditions” is an umbrella term for the wide range of physical and mental health
consequences that are present four or more weeks after SARS-CoV-2 infection, including by patients who
initially had mild or asymptomatic COVID-19. NIH employs the term, Post-Acute Sequalae of SARS-CoV-2
infection (PASC), the result of the direct effects of the virus. The World Health Organization (WHO) defines
Long COVID as symptoms “lasting greater than 2 months, starting within 3 months from the onset” of COVID-
19.
Signs and symptoms associated with Long COVID vary widely and can last for weeks, months, or years. In
some individuals, signs and symptoms may resolve over time without treatment. Common
signs and
symptoms include tiredness or fatigue that interferes with daily life, signs and symptoms that get worse after
physical or mental effort (post-exertional malaise), respiratory symptoms, cardiac symptoms, neurologic
symptoms, digestive symptoms, joint or muscle pain, rash, changes in menstrual cycles, and others. The
presentation of signs, symptoms and severity range widely making them difficult to diagnose. This guide
highlights some of the more common Long COVID signs, symptoms, and potential subsequent conditions.
3
Prepared by
The VHA Long COVID Integrated Project Team Workstream 1:
Strategies and Best Practices
With support from
The VHA Long COVID Integrated Project Team
The VHA Long COVID Community of Practice
The VHA Office of Primary Care
The VHA Office of Healthcare Innovation and Learning
The VA Office of Information & Technology, Office of the Chief
Technology Officer
The VHA Office of Healthcare Transformation
The VHA Office of Patient Connected Care and Cultural Transformation
The VHA National Center for Health Promotion and Disease Prevention
VHA Pharmacy Benefits Management Services
The San Francisco VA HCS Office of Diversity, Equity, and Inclusion
4
DIRECTORY OF SIGNS, SYMPTOMS, AND OTHER POTENTIAL
CONDITIONS
One-page guides are provided for signs, symptoms, and other potential subsequent conditions. Each guide is
hyperlinked below and includes the following details: things to keep in mind, evaluation with labs and tests,
PACT management, and consult suggestions.
Quick Guides
• ANOSMIA AND DYSGEUSIA 7
•
AUTONOMIC NERVOUS SYSTEM DYSREGULATION 8
•
CHEST PAIN 9
•
COGNITIVE IMPAIRMENT 10
•
COUGH 11
•
DYSPNEA 12
•
FATIGUE AND ACTIVITY INTOLERANCE 13
•
HEADACHES 14
•
MENTAL HEALTH (ANXIETY, DEPRESSION, PTSD) 15
•
OTHER POTENTIAL CONDITIONS: CARDIOMETABOLIC AND AUTOIMMUNE 16
Quick Links
• APPENDIX A: OLFACTORY TRAINING 17
•
APPENDIX B: FATIGUE AND ACTIVITY INTOLERANCE 18
•
APPENDIX C: 30 SECOND SIT TO STAND TEST 20
•
APPENDIX D: COMPOSITE AUTONOMIC SYMPTOM SCORE (COMPASS 31) 21
•
RESOURCES 26
•
ADDITIONAL REFERENCES 27
5
INTRODUCTION
VA’s Office of Research and Development, the Long COVID Community of Practice, and the Long COVID
Integrated Project Team are working to organize, support, and report on the development of a national
program to help all Veterans who have Long COVID. They collaborated to produce this document for health
care providers to better facilitate defining, assessing, referring, and managing common Long COVID signs,
symptoms, and potential subsequent conditions using a Whole Health System approach. Whole Health is an
evidence-informed, multi-disciplinary, personalized, Veteran-driven approach that empowers and equips
Veterans to take charge of their health and well-being, and to live life to the fullest. (Gaudet T, 2019) (Krejci L,
2014)
As one of the largest health care systems in the United States, VHA is leading the charge to deliver care to
Veterans with Long COVID whether post-COVID-19 conditions (PCC) (direct and indirect effects of the virus)
and the subset Post-Acute Sequelae of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2)
infection (PASC) (direct effects of the virus), hereafter referred to as Long COVID. At the time of this writing, it
is estimated that 4-7% (Xie Y, 2021) of those diagnosed with COVID-19, or 2% of the U.S. population, will
develop Long COVID. Based on approximately 600,000 known Veterans with a diagnosis of COVID-19, this
equates to 24,000-42,000 Veterans. However, these numbers have the potential to be much higher, as the
VA has more than 6 million Veterans in care.
Organizations have defined Long COVID with differing parameters. The Centers for Disease Control and
Prevention (CDC) and National Institutes of Health (NIH) define Long COVID as “new or worsening
symptoms” from “4 weeks after first being infected” with COVID-19. According to the CDC, the term “post-
COVID conditions” is an umbrella term for the wide range of physical and mental health consequences that
are present four or more weeks after SARS-CoV-2 infection, including by patients who initially had mild or
asymptomatic COVID-19. NIH employs the term, Post-Acute Sequalae of SARS-CoV-2 infection (PASC), the
result of the direct effects of the virus. The World Health Organization (WHO) defines Long COVID as
symptoms “lasting greater than 2 months, starting within 3 months from the onset” of COVID-19.
A challenge for many health care providers is diagnosing Long COVID because there are several signs and
symptoms associated with the syndrome, some of which may resolve without treatment over time in certain
individuals. It is important to separate pre-existing signs and symptoms from those that have worsened or
those that are new since a COVID-19 diagnosis. This document is not intended to replace clinical judgment.
Rather, it provides suggestions for health care providers as they engage in shared health care decision-
making with Veterans who have this syndrome.
This guide is broken into several sections: an Executive Summary including a navigation guide, a primer on
the Whole Health System approach, and quick reference guides for Veterans’ care. Long COVID research is
in its infancy and the information available on Long COVID is ever changing. For example, there is minimal
evidence to-date on Long COVID and special populations such as racial and ethnic minorities and
transgender people. This document will be periodically updated and republished as the scientific community
learns more about Long COVID.
6
Whole Health System Approach to Long COVID Care
Whole Health is an evidence-based, multi-disciplinary, personalized, Veteran-driven approach that empowers
and equips Veterans to take charge of their health and well-being, and to live life to the fullest. The VA has
adopted the Whole Health System approach across many health sectors.
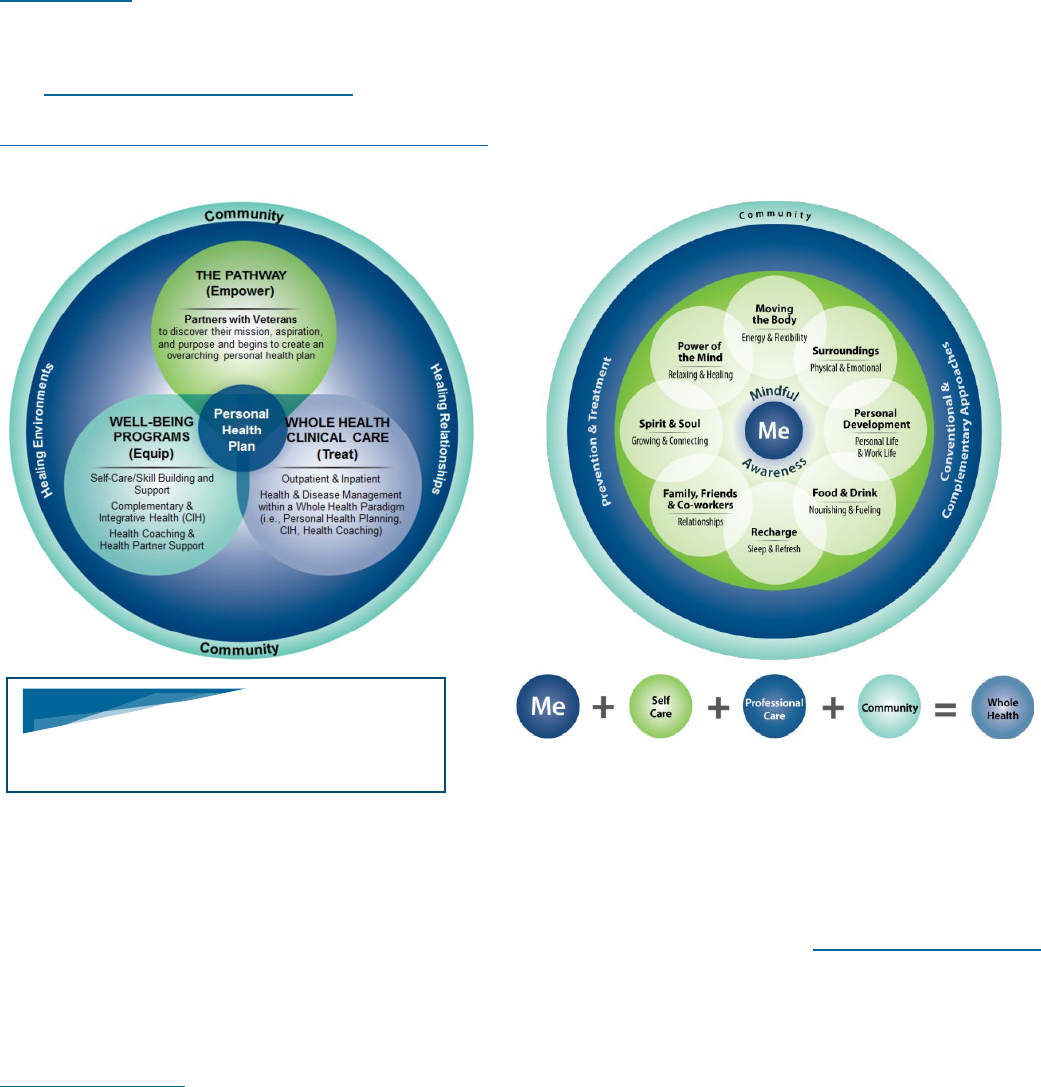
The Whole Health System approach consists of the following three components: The Pathway, Well-Being
Programs, and Whole Health Clinical Care. Included in the Whole Health System are health coaching,
complementary and integrative health approaches such as acupuncture and yoga, alongside conventional
care.
Discussing what is most important to the Veteran ensures that the Veteran and their unique circumstance is
at the center of health care, not just their signs and symptoms. This encourages and emphasizes the
Veteran’s ability to shape their health and well-being through self-care and self-management.
As part of this care, Veterans conclude their visit with a Personalized Health Plan that typically includes at
least one specific, measurable, attainable, realistic, and time-bound (SMART) goal. Building a SMART goal
with a provider injects the care and expertise of professional care for prevention and treatment aligned with
the Veteran’s personal health plan. A SMART goal considers a Veteran’s needs and environment, the
community of support a Veteran has, as well as those who rely on the Veteran for support, social
determinants of health, and other important factors that affect a Veteran’s everyday life. These and other
Whole Health tools help to ensure a Veteran-focused visit that empowers the Veteran to be an active
participant in their health goals.
In the following pages, we delineate an evidence-informed Whole Health System approach to Long COVID
care. Importantly, the Whole Health System of care is not solely a separate and standalone consult service or
program, rather it is a system-wide approach. This document is intended to be a broad approach, leaving
room for clinical judgment, individual circumstances, medical resources, and pre-existing referral patterns. As
the knowledge around Long COVID evolves, additional iterations of this guide will become available.
WHAT IS MOST IMPORTANT TO YOU
TO DISCUSS IN THE VISIT TODAY?

7
ANOSMIA AND DYSGEUSIA
This provides suggestions as you engage in shared health care decision-making with Veterans. It is not
intended to replace clinical judgement.
Up to 46% of patients reported anosmia at greater than 4 weeks post-COVID-19
1
(NICE, 2021), and
specifically 16% of non-hospitalized patients reported anosmia at 60- or 90-days post-COVID-19 onset.
2
(Yoo S, 2022)
Things to Keep in Mind
May need to prompt Veteran, as this may not be the primary complaint
May be associated with cognitive changes
3
(Douaud G, 2022), neurologic changes
4
(Premraj L, 2022),
phantosmia (smells that are not present) and dysosmia (altered sense of smell/taste such as excessive
chemical, salty or sour sensations)
Assess for possible contributors such as sinus disease and rhinitis
Assess the effect on food choices and quality of life
Hypertension (HTN) after anosmia and dysgeusia may occur due to increased salt placed on food
Educate on safety considerations (e.g., strategies to avoid spoiled food, increase vigilance to monitor
safety detectors in the home, etc.)
Assess pregnancy/lactation status, review teratogenic medications
Evaluation
Labs to Consider Tests to Consider
None None
PACT Management to Consider
Consults to Consider
ICD-10 Code: U09.9, Post-COVID-19 condition,
unspecified
Intranasal steroids may be used if other nasal signs
and symptoms with anosmia like congestion or rhinitis
are present; no strong data that steroids (oral or
intranasal) are significantly beneficial for isolated
post-COVID-19 anosmia
Recommend against antibiotics and Vitamin A drops
5
(Addison A, 2021)
6
(Hopkins C, 2021)
Smell/olfactory retraining and advice (Appendix A):
• The act of regularly sniffing or exposing oneself to
robust aromas with the intention of regaining a
sense of smell
Speech Language Pathology or
Occupational Therapy: olfactory
retraining, as well as additional
education and implementation
strategies to support safety
considerations related to impaired
smell
Ear, Nose, Throat (ENT) or Speech
Language Pathology: concurrent
dysphonia or dysphagia
Neurology: previous head injury or
neurologic signs and symptoms
Whole Health System approach:
Whole Health Coaching
1
National Institute for Health and Care Excellence (NICE) UK, https://www.nice.org.uk/guidance/ng188
2
Yoo S. Factors Associated with Post-Acute Sequelae of SARS-CoV-2 (PASC) After Diagnosis of Symptomatic COVID-19 in the Inpatient and
Outpatient Setting in a Diverse Cohort. J Gen Intern Med. 2022 Jun;37(8):1988-1995. doi: 10.1007/s11606-022-07523-3.
3
Douaud G. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature. 2022 Apr;604(7907):697-707. doi: 10.1038/s41586-022-
04569-5
4
Premraj L. Mid and long-term neurological and neuropsychiatric manifestations of post-COVID-19 syndrome: A meta-analysis. J Neurol Sci. 2022 Mar
15;434:120162. doi: 10.1016/j.jns.2022.120162
5
Addison A. Clinical Olfactory Working Group consensus statement on the treatment of postinfectious olfactory dysfunction. J Allergy Clin Immunol.
2021 May;147(5):1704-1719. doi: 10.1016/j.jaci.2020.12.641
6
Hopkins C. Management of new onset loss of sense of smell during the COVID-19 pandemic - BRS Consensus Guidelines. Clin Otolaryngol. 2021
Jan;46(1):16-22. doi: 10.1111/coa.13636.

8
AUTONOMIC NERVOUS SYSTEM DYSREGULATION
This provides suggestions as you engage in shared health care decision-making with Veterans. It is not intended to
replace clinical judgement.
Autonomic nervous system dysregulation may be present even after mild cases of COVID-19. Up to 48% of patients
reported dizziness or light headedness greater than 4 weeks post-COVID-19.
7
(NICE, 2021) Of 180 post-COVID-19
patients, 7.2% experienced dizziness and 61% of patients had autonomic dysfunction.
8
(Stella A, 2022)
Things to Keep in Mind
Signs and symptoms may manifest as palpitations, lightheadedness, dizziness, fatigue, blurry vision, falling,
presyncope and decreased exercise tolerance
Consider systemic conditions such as deconditioning, dehydration, anemia, hypoxia, anxiety, Parkinson’s Disease,
persistent fever, lung disease, and cardiac disease, including sinus node dysfunction, myocarditis, and heart failure
Consider orthostatic hypotension versus orthostatic tachycardia
Review medications such as diuretics, antidepressants, certain beta blockers
Assess pregnancy/lactation status, review teratogenic medications
Evaluation
Labs to Consider
Tests to Consider
Comprehensive
Metabolic Panel
(CMP)
Glucose
(hypoglycemia)
Complete Blood
Count (CBC)
(anemia)
Electrocardiogram (EKG) (arrythmia)
Evaluate for orthostatic blood pressure (lying, standing) for up to 10 minutes:
• Have patient lie down for 5 minutes and then measure blood pressure (BP) and
heart rate (HR). Have patient stand up and measure BP and HR after every 2
minutes for 10 minutes
• If there is a drop of systolic blood pressure (SBP) by 20 points or diastolic blood
pressure (DBP) by 10 points, then it is considered positive for orthostatic
hypotension
• If the HR increases by >30 BPM without hypotension, then it is positive for
orthostatic tachycardia
PACT Management to Consider
Consults to Consider
ICD-10 Code: U09.9, Post-COVID-19 condition, unspecified
Post-Acute Sequelae of COVID-19 and Cardiovascular Autonomic Dysfunction:
What Do We Know?
Consider using Composite Autonomic Symptom Score (COMPASS 31)
9
(Sletten DM, 2012) for evaluating symptom trends (Appendix D)
Hydration immediately; for postural orthostatic tachycardia syndrome (POTS)
consider 64 ounces of water intake daily
Avoid or limit alcohol intake as it can worsen or precipitate orthostatic
hypotension
Use of salt with caution especially if there is history of left ventricular
dysfunction (LVD); POTS recommendation is 3000-5000 mg per day
Avoid strenuous activity in hot weather
Start with recumbent or semi-recumbent exercise (rowing, swimming, cycling)
with gradual transition to upright exercise (walking, jogging, elliptical) as
orthostatic intolerance improves
Titrated return to activity program (Appendix B)
Lifestyle modification including slowly getting out of bed before standing and
use of compression stockings
Frequent, small, balanced meals with whole foods, protein, vegetables, and
fruits, and high fiber for POTS
Biofeedback
Cardiology:
• If assessment is
negative but high
clinical suspicion for
POTS
Physical Therapy:
• Titrated return to
individualized activity
program (Appendix B)
and energy
conservation
techniques
Occupational Therapy:
• Energy conservation
techniques
• Activities of daily
living (ADLs)
Whole Health System
approach:
• Biofeedback, yoga,
health coaching
Nutrition
7
National Institute for Health and Care Excellence (NICE) UK, https://www.nice.org.uk/guidance/ng188
8
Stella A. Autonomic dysfunction in post-COVID patients with and without neurological symptoms: a prospective multidomain observational study. Journal of
Neurology. 2022 Feb;269(2):587-596. doi: 10.1007/s00415-021-10735-y
9
Sletten DM. COMPASS 31: a refined and abbreviated Composite Autonomic Symptom Score. Mayo Clin Proc. 2012 Dec;87(12):1196-201. doi:
10.1016/j.mayocp.2012.10.013. PMID: 23218087; PMCID: PMC3541923

9
CHEST PAIN
This provides suggestions as you engage in shared health care decision-making with Veterans. It is not
intended to replace clinical judgement.
Chest pain is a common symptom with almost 5% of those diagnosed with COVID-19 reporting chest pain
>12 weeks after initial illness.
10
(Whitaker M, 2022) The usual conditions are considered in the differential for
recurrent chest pain.
11
(Gluckman T, 2022) In particular after COVID-19, cardiovascular conditions
including myocardial infarction (MI) and myocarditis were noted to be higher compared to those without
COVID-19, even in younger patients.
12
(Xie Y, 2022) The reason is unclear but may be related to virally
mediated vascular endothelial injury or indirectly from the immune response.
13
(Bellan M, 2021)
Furthermore, there seems to be a number of people with atypical chest pain that may be part of a post-
COVID-19 pain syndrome.
Things to Keep in Mind
The evaluation is similar to routine evaluation for chest pain
Maintain a high degree of suspicion for coronary artery disease (CAD), myocarditis/pericarditis, and
venous thromboembolism (VTE) given elevated risk after COVID-19 infection
Assess pregnancy/lactation status, review teratogenic medications
Evaluation
Labs to Consider
Tests to Consider
None
Additional testing as indicated by history and
exam
PACT Management to Consider
Consults to Consider
ICD-10 Code: U09.9, Post-COVID-19
condition, unspecified
For pleuritic pain or costochondritis:
• Diaphragmatic breathing
• Stretching
• 1 or 2 weeks of low dose non-steroidal
anti-inflammatory drugs (NSAID)
• If signs and symptoms worsen,
consider gastrointestinal causes like
esophagitis or esophageal spasm
Cardiology: if no improvement with initial therapies
described, or concern for underlying cardiac
disease or complications (myocarditis, heart
failure, ischemia/CAD, arrhythmia)
Physical Therapy: for accessory muscle usage/rib
excursion after ruling out cardiac issues
Chiropractic Care
Whole Health System approach: health coaching,
acupuncture
10
Whitaker M. Persistent COVID-19 symptoms in a community study of 606,434 people in England. Nature Communications 13, 1957 (2022).
https://doi.org/10.1038/s41467-022-29521-z
11
Gluckman T. 2022 ACC Expert Consensus Decision Pathway on Cardiovascular Sequelae of COVID-19 in Adults: Myocarditis and Other Myocardial
Involvement, Post-Acute Sequelae of SARS-CoV-2 Infection and Return to Play. J American College Cardiology. 2022 May, 79 (17) 1717–1756.
https://doi.org/10.1016/j.jacc.2022.02.003
12
Xie Y. Long-term cardiovascular outcomes of COVID-19. Nature Medicine 28, 583–590 (2022).https://doi.org/10.1038/s41591-022-01689-3
13
Bellan M. Respiratory and Psychophysical Sequelae Among Patients With COVID-19 Four Months After Hospital Discharge. JAMA Network Open.
2021;4(1):e2036142. doi:10.1001/jamanetworkopen.2020.36142

10
COGNITIVE IMPAIRMENT
This provides suggestions as you engage in shared health care decision-making with Veterans. It is not intended to
replace clinical judgement.
Cognitive impairment is found in up to 60% of patients greater than 4 weeks after COVID-19. In some studies, 23% of
patients reported persistent signs and symptoms more than 8 months after COVID-19.
14
(NICE, 2021)
Things to Keep in Mind
Patient signs and symptoms
15
(AAPM&R, 2022)
• Attention - Brain fog, lost train of thought, concentration problems
• Processing Speed - Slowed thoughts
• Motor Function - Slowed movements
• Language - Word finding problems, reduced fluency
• Memory - Poor recall, forgetting tasks
• Mental Fatigue - Exhaustion, brain fog
• Executive Function - Poor multitasking and/or planning
• Visuospatial - Blurred vision, neglect
Perform a workup aiming to address reversible causes of dementia or cognitive impairment
Consider screenings for mental health, substance use and sleep disturbances
Assess pregnancy/lactation status, review teratogenic medications
Evaluation
Labs to Consider
Tests to Consider
B12
Thyroid stimulating hormone (TSH)
Glucose
Rapid plasma reagin (RPR)
For purely cognitive impairment without other
neurologic signs and symptoms, magnetic
resonance imaging (MRI) or head computed
tomography (CT) is not routinely indicated
PACT Management to
Consider
Consults to Consider
ICD-10 Code: U09.9, Post-
COVID-19 condition,
unspecified
Medication reconciliation
Diaphragmatic breathing
Occupational Therapy, Speech Language Pathology or Primary Care
Mental Health Integration (PCMHI): perform Montreal Cognitive
Assessment (MOCA), Mini-Mental State Exam (MMSE), or Saint
Louis University Mental Status (SLUMS)
Occupational Therapy and Speech Language Pathology: perform
cognitive assessment, cognitive rehabilitation, functional assessment
and evaluate impact upon activities of daily living (ADLs), work,
school, and hobbies
PCMHI: address mental health concerns associated with coping with
new signs and symptoms, and provide cognitive behavioral therapy
for insomnia (CBT-I)
Nutrition: Nutrition optimization, food diary, and glucose regulation
Whole Health System approach: mindfulness/meditation, Tai Chi,
acupuncture, health coaching
Neurology: At initial visit if there are focal signs and symptoms or “red
flags” to suggest a systemic disease, OR potentially after 12-24
weeks if signs and symptoms worsen or persist, affecting daily
function and quality of life despite cognitive rehabilitation
14
National Institute for Health and Care Excellence (NICE) UK, https://www.nice.org.uk/guidance/ng188
15
American Academy of Physical Medicine and Rehabilitation. https://www.aapmr.org/members-publications/covid-19/pasc-guidance

11
COUGH
This provides suggestions as you engage in shared health care decision-making with Veterans. It is not
intended to replace clinical judgement.
Cough appears to be more common and duration may be longer after COVID-19.
16
(NICE, 2021) Cough
often persists for weeks to months after resolution of initial illness with 5-30% of patients reporting cough at 3
months.
17
(Jutant EM, 2022)
18
(Goërtz YMJ, 2020) There are likely multiple reasons potentially related to
development of fibrosis and underlying conditions such as asthma. For many people the cause is a post-
infectious cough, which is often managed like cough-variant asthma. The evaluation will be similar to
subacute and chronic cough for which the typical time courses are 3-8 weeks and >8 weeks, respectively.
Things to Keep in Mind
Post-infectious cough is likely a common cause which means it should resolve with time
Worsening cough could suggest secondary bacterial pneumonia or organizing pneumonia, which are
uncommon, so always correlate with dyspnea and hypoxia
Assess classic contributors such as gastroesophageal reflux disease (GERD), post-nasal drip, and
pulmonary fibrosis
Assess pregnancy/lactation status, review teratogenic medications
Evaluation
Labs to Consider
Tests to Consider
None
If greater than 8 weeks post COVID-19,
consider:
• Chest X-Ray
• Pulmonary Function Test (including pre-/post-
bronchodilator)
• Chest CT
PACT Management to Consider
Consults to Consider
ICD-10 Code: U09.9, Post-COVID-19 condition,
unspecified
Medication reconciliation to rule out iatrogenic causes
such as angiotensin-converting enzyme inhibitors
(ACE-i)
Similar to cough-variant asthma with albuterol as
needed, inhaled corticosteroid (ICS), and ICS/long-
acting beta-agonist (LABA) for progressively severe or
more frequent episodes
Should limit to 2–3-month empiric trial and re-evaluate
if not resolved
Sputum management using hydration, expectorants,
and airway clearance devices
Diaphragmatic Breathing
Pulmonary: if continued cough
>12 weeks despite initial
treatment
Whole Health System approach:
biofeedback, mind body skills,
health coaching, yoga, Tai Chi
16
National Institute for Health and Care Excellence (NICE) UK, https://www.nice.org.uk/guidance/ng188
17
Jutant EM. Respiratory symptoms and radiological findings in post-acute COVID-19 syndrome. ERJ Open Res 2022;8. 10.1183/23120541.00479-
2021
18
Goërtz YMJ. Persistent symptoms 3 months after a SARS-CoV-2 infection: the post-COVID-19 syndrome? ERJ Open Res. 2020 Oct 26;6(4). doi:
10.1183/23120541.00542-2020.

12
DYSPNEA
This provides suggestions as you engage in shared health care decision-making with Veterans. It is not intended to
replace clinical judgement.
Post-COVID-19 dyspnea is common with multiple etiologies including cardiac, pulmonary, and neuromuscular issues.
Prevalence is likely proportional to initial severity with dyspnea reported in ~5-10% of mild (outpatient) cases,
19
(Sudre
CH, 2021)
20
(Nehme M, 2021) but up to 15-50% of those hospitalized.
21
(Carfi A, 2020)
22
(Froidure A, 2021)
23
(Jutant
EM, 2022) Patients who initially had mild COVID-19, and did not experience hypoxemia or require hospitalization, are
less likely to have post-acute pulmonary function or imaging abnormalities.
24
(AAPM&R, 2022)
Things to Keep in Mind
A functional assessment evaluating ADLs and recovery time after activity is helpful for triaging severity and creating
a titrated return to individualized activity program (Appendix B)
Differentiate between dyspnea at rest (forgetting to breathe), dyspnea with movement (bending forward), dyspnea
with exertion with or without hypoxemia, and post-exertional malaise (disproportionately long recovery time after
exertion)
Consider evaluation for pulmonary embolism (PE)
25
(Li P, 2021), coronary artery disease (CAD)
26
(Xie Y, 2022),
interstitial lung disease and myocarditis
27
(Puntmann VO, 2020)
28
(Daniels CJ, 2021) if clinically indicated given
higher rates after COVID-19
Assess pregnancy/lactation status, review teratogenic medications
Evaluation
Labs to Consider
Tests to Consider
Complete blood count (CBC)
If on oral contraceptive pill (OCP) with relevant
Wells or modified Geneva score, consider D-dimer
to screen for pulmonary thrombosis
Troponin if suspicious for myocarditis
Assess oxygen saturation at rest and with exertion
If lasting more than 8 weeks, consider:
• 2-view chest x-ray (CXR)
• Electrocardiogram (EKG)
• Pulmonary function tests (PFT)
PACT Management to Consider
Consults to Consider
ICD-10 Code: U09.9, Post-COVID-19
condition, unspecified
Supplemental oxygen
Pharmacologic therapies, including oral
corticosteroids, inhaled bronchodilators,
and inhaled corticosteroids, are not
routinely recommended for breathing
discomfort in the absence of a specific
diagnosis such as asthma
Heart healthy diet
Stress management
Diaphragmatic Breathing
Pulmonary: Persistent hypoxia at 6 weeks or abnormal work-up;
otherwise >12 weeks with persistent symptoms
Cardiology: Abnormal EKG, stress test, or highly suspicious for
cardiac etiology
Pulmonary rehabilitation: After prerequisite clinical assessment
for CAD, hypoxia, and participation (orthostatic hypotension)
while excluding post-exertional malaise
Ear, Nose, Throat (ENT) or Speech Language Pathology:
concurrent dysphonia or dysphagia
Physical Therapy: titrated return to individualized activity
program (Appendix B) if no post-exertional malaise
Occupational Therapy: regulated breathing during daily task
engagement in home and the community
Whole Health System approach: health coaching
19
Sudre CH. Attributes and predictors of long COVID. Nature Medicine. 2021 Apr;27(4):626-631. doi: 10.1038/s41591-021-01292-y
20
Nehme M, CoviCare Study T. Prevalence of Symptoms More Than Seven Months After Diagnosis of Symptomatic COVID-19 in an Outpatient Setting. Annals
of Internal Medicine 2021;174:1252-60. doi: 10.7326/M21-0878.
21
Carfi A. Persistent Symptoms in Patients After Acute COVID-19. JAMA 2020;324:603-5.
22
Froidure A, Mahsouli A, Liistro G, et al. Integrative respiratory follow-up of severe COVID-19 reveals common functional and lung imaging sequelae.
Respiratory Medicine 2021;181:106383. doi: 10.1016/j.rmed.2021.106383.
23
Jutant EM. Respiratory symptoms and radiological findings in post-acute COVID-19 syndrome. European Respiratory Journal Open Res 2022;8 (2):00479-
2021. doi: 10.1183/23120541.00479-2021.
24
American Academy of Physical Medicine and Rehabilitation (AAPM&R). https://www.aapmr.org/members-publications/covid-19/pasc-guidance
25
Li P. Factors Associated With Risk of Postdischarge Thrombosis in Patients With COVID-19. JAMA Network Open. 2021 Nov 1;4(11):e2135397. doi:
10.1001/jamanetworkopen.2021.35397
26
Xie Y. Long-term cardiovascular outcomes of COVID-19. Nat Med 28, 583–590 (2022). https://doi.org/10.1038/s41591-022-01689-3
27
Puntmann VO. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19).
JAMA Cardiology. 2020 Nov 1;5(11):1265-1273. doi: 10.1001/jamacardio.2020.3557
28
Daniels CJ. Prevalence of Clinical and Subclinical Myocarditis in Competitive Athletes With Recent SARS-CoV-2 Infection: Results From the Big Ten COVID-
19 Cardiac Registry. JAMA Cardiology. 2021;6(9):1078–1087. doi:10.1001/jamacardio.2021.2065

13
FATIGUE AND ACTIVITY INTOLERANCE
This provides suggestions as you engage in shared health care decision-making with Veterans. It is not intended
to replace clinical judgement.
Fatigue is one of the most common Long COVID related signs and symptoms in multiple studies, with an
incidence of 63% in those hospitalized
29
(AAPM&R, 2022) and 46% in those not hospitalized.
30
(Stavem K, 2021)
Things to Keep in Mind
Assess the Veteran’s prior level of function (independence with activities of daily living (ADLs), working
hobbies, exercising), current level of function, and recovery time from activities
Veteran may experience post-exertional malaise, making a titrated return to individualized activity (Appendix
B) important
Screen for mental health, substance disorder, sleep disturbances
Medication reconciliation
Women more likely to experience fatigue at 6 months
31
(Xiong Q, 2021)
Assess pregnancy/lactation status, review teratogenic medications
Evaluation
Labs to Consider
Tests to Consider
Complete blood count (CBC)
Thyroid stimulating hormone (TSH)
B12
Vitamin D
Comprehensive Metabolic Panel (CMP)
Hemoglobin A1C
Consider:
• Human immunodeficiency virus (HIV)
• Hepatitis C virus (HCV)
Ambulatory pulse oximetry
30 second sit to stand to evaluate functional
lower extremity strength and endurance, and
provide information about fall risk, activity
tolerance, activity endurance, and functional
mobility (Appendix C)
29
(AAPM&R, 2022)
Evaluate other organ systems that may have
been affected by COVID-19 that impact exercise
participation (e.g., cardiac, pulmonary)
PACT Management to Consider
Consults to Consider
ICD-10 Code: U09.9, Post-COVID-19
condition, unspecified
Titrated return to individualized activity
program (Appendix B)
Diaphragmatic Breathing
Cognitive Behavioral Therapy (CBT) for
Insomnia
Replete B12 if low
Replete Vitamin D if low
Consider Fish oil – 1000mg (500mg
DHA/EPA) capsule combined
eicosapentaenoic acid (EPA) and
docosahexaenoic acid (DHA) daily with food
(avoid if on blood thinners or experiencing
gastroesophageal reflux disease (GERD))
Occupational Therapy for a titrated return to
individualized activity program (Appendix B) and
energy conservation techniques
Physical Therapy for titrated return to individualized
activity program (Appendix B)
Physical Medicine & Rehabilitation (PM&R)
Cardiology
Pulmonology
Mental Health
Nutrition to discuss an anti-inflammatory lifestyle
and diet history.
Whole Health System approach: mindfulness,
health coaching, yoga, Tai Chi, biofeedback
29
American Academy of Physical Medicine and Rehabilitation (AAPM&R). https://www.aapmr.org/members-publications/covid-19/pasc-guidance
30
Stavem K. Prevalence and Determinants of Fatigue after COVID-19 in Non-Hospitalized Subjects: A Population-Based Study. Int J Environ Res Public
Health. 2021 Feb 19;18(4):2030. doi: 10.3390/ijerph18042030
31
Xiong Q. Clinical sequelae of COVID-19 survivors in Wuhan, China: a single-centre longitudinal study. Clin Microbiol Infect. 2021 Jan;27(1):89-95. doi:
10.1016/j.cmi.2020.09.023

14
HEADACHES
This provides suggestions as you engage in shared health care decision-making with Veterans. It is not
intended to replace clinical judgement.
Up to 79% of patients reported headache at greater than 4 weeks post-COVID-19
32
(NICE, 2022), though
this improved with time and 10.6% reported ongoing headaches at 90 days, and 8.4% ≥180 days after
symptom onset/hospital discharge.
33
(Fernández-de-Las-Peñas C, 2021)
Things to Keep in Mind
Consider screening for mental health, substance use disorder, sleep disturbances, traumatic brain
injury (TBI)
Neurological examination warranted
Medication reconciliation
Consider the following:
• Pre-COVID-19 episodic migraine now chronic post-COVID-19
• Delayed onset COVID-19 headache
• Persistent headache with migraine features onset with COVID-19
• Sinus congestion
• Cervical and upper back muscle tightness
• Increased stress level
• Medication rebound headache
Assess pregnancy/lactation status, review teratogenic medications
Evaluation
Labs to Consider
Tests to Consider
None
No recommendations for imaging if headache only
PACT Management to Consider
Consults to Consider
ICD-10 Code: U09.9, Post-COVID-19 condition,
unspecified
Treating Headaches Handout for Patients
Over the counter (OTC) and prescription
analgesic review
Lifestyle management and evaluation (sleep,
exercise, nutrition, headache diary)
Consider Riboflavin 400mg every morning with
food
Consider Magnesium Oxide 420mg every
evening
Regulate glucose levels
Recommend 64 ounces of water daily
Diaphragmatic Breathing
Neurology: if no improvement despite
initial management or if abnormal
neurological examination present
Nutrition: to discuss an anti-
inflammatory diet and headache
elimination diet
Whole Health System approach:
biofeedback, mindfulness, health
coaching, yoga, acupuncture, Tai Chi
Chiropractic Care
Osteopathy
32
NICE https://www.nice.org.uk/guidance/ng188/resources/covid19-rapid-guideline-managing-the-longterm-effects-of-covid19-pdf-51035515742
33
Fernández-de-Las-Peñas C. Headache as an acute and post-COVID-19 symptom in COVID-19 survivors: A meta-analysis of the current literature.
Eur J Neurol. 2021 Nov;28(11):3820-3825. doi: 10.1111/ene.15040.

15
MENTAL HEALTH (ANXIETY, DEPRESSION, PTSD)
This provides suggestions as you engage in shared health care decision-making with Veterans. It is not
intended to replace clinical judgement.
Anxiety, depression, sleep disturbances and post-traumatic stress disorder (PTSD) have been reported in 30 -
40% of COVID-19 survivors, similar to survivors of other pathogenic coronaviruses.
34
(Nalbandian A, 2021)
These signs and symptoms may be exacerbated by specific COVID-19 related or pandemic-associated events
such as loneliness, job loss, childcare issues, lack of typical recreational activities, and relationship strain.
Things to Keep in Mind
Given the overall increase in suicides during the pandemic and the increased risk for mental health
symptoms following COVID-19, consider assessment for suicidality
Complete usual mental health screens and discern whether reported signs and symptoms are temporally
related to Long COVID (increase in previous or new signs and symptoms)
Normalize and validate signs and symptoms as appropriate
Assess contribution from sleep disturbances, physical function changes, substance use, and other lifestyle
changes that may affect mental health
Consider the following:
• Adjustment Disorder following change in health or role
• Generalized Anxiety Disorder
• Panic Disorder
• Obsessive Compulsive Disorder
• Depression
• Anxiety related to air hunger
• Acute Stress Disorder
• Post-Traumatic Stress Disorder
• Post Intensive Care Syndrome
• Sleep Disorders to include insomnia
• Substance Use Disorder
• Coping with stigma
• Survivor’s guilt
• Problems in relationship
Assess pregnancy/lactation status, review teratogenic medications
Evaluation
Labs to Consider
Tests to Consider
Routine labs for mental health evaluation
None
PACT Management to Consider
Consults to Consider
ICD-10 Code: U09.9, Post-COVID-19 condition, unspecified
Explore Veteran’s hope to address signs and symptoms using
Veteran's mission, aspiration, and purpose.
Primary Care Mental Health Integration (PCMHI)
Veterans Crisis Line – contact options:
• Dial 988 then Press 1
• Dial 800-273-8255 then press 1
• Text 838255
COVID-19 Coach App – Stress management
Insomnia Coach App - Path to better sleep
Diaphragmatic Breathing
Guided Meditation – Audio files
Consider antidepressant
Consider Fish oil – 1000mg (500mg DHA/EPA) capsule
combined eicosapentaenoic acid (EPA) and docosahexaenoic
acid (DHA) daily with food (avoid if on blood thinners or
experiencing gastroesophageal reflux disease (GERD))
Explore interest in Mental Health
follow up
• Mental Health consult for
high complexity
Long COVID Support Groups
Nutrition
Physical Therapy: titrated return
to individualized activity program
(Appendix B)
Peer Support Specialists
Whole Health System approach:
health coach, Tai Chi, yoga,
acupuncture/battlefield
acupuncture/national
acupuncture detox
Chaplain
34
Nalbandian A. Post-acute COVID-19 syndrome. Nat Med. 2021 Apr;27(4):601-615. doi: 10.1038/s41591-021-01283-z

16
OTHER POTENTIAL CONDITIONS:
CARDIOMETABOLIC AND AUTOIMMUNE
This provides suggestions as you engage in shared health care decision-making with Veterans. It is not intended to replace
clinical judgement.
Given evidence that COVID-19 may increase the risk for Diabetes, renal impairment, cardiovascular complications and
autoimmune conditions, a history of infection should be considered along with other factors in deciding who should be
screened for these conditions.
Cardiovascular
Increased risk of myocardial infarction (MI),
cardiovascular accident (CVA), congestive heart
failure (CHF), myocarditis
35
(Xie Y, 2022)
High awareness for cardiovascular complications
36
(Gluckman T, 2022)
Kidney Disease
Increased risk of significant decline in estimated
glomerular filtration rate (eGFR), proportional to
severity of disease, though present even in those
not admitted to the hospital
37
(Bowe B, 2021)
If not already assessed, evaluate kidney function glomerular
filtration rate (GFR) using creatine or cystatin C at 3-6
months after resolution of COVID-19
Compare results to pre-COVID-19 GFR if available
Diabetes
Compared with those who never had COVID-19,
Veterans who have had COVID-19 are at greater
risk of developing type 2 Diabetes up to a year later,
even after a mild SARS-CoV-2 infection.
38
(Xie Y,
2022)
39
(Wander P, 2022)
Ask all Veterans who had severe COVID-19 about signs and
symptoms of diabetes at every routine visit. Consider asking
Veterans who had mild or asymptomatic COVID-19.
A baseline A1c test should be done post-COVID-19 for all
Veterans
For symptomatic Veterans:
• Veterans experiencing post-COVID-19 signs and
symptoms with pre-existing diabetes should have an
additional A1c test at 6 months post-infection
• Veterans experiencing post-COVID-19 signs and
symptoms without pre-diabetes but with significant risk
factors for diabetes- such as strong family history and
obesity-can be considered for an A1c test at 6 months
post-infection
• Routine laboratory testing for other indications should
include a Fasting Blood Glucose (FBS) when possible
• If there has been a significant increase (>0.5%) in A1c
from baseline, obtain a repeat A1c or FBS earlier than 6
months post-infection
Autoimmune
Up to 25% may develop antinuclear antibody (ANA)
positivity, but the titers were low and deemed not
clinically significant.
40
(Lerma L, 2020) The serology
of 61 patients 5 weeks after COVID-19 had no
increased incidence of anti-cyclic citrullinated
peptides (CCP) positivity.
41
(Derksen V, 2021)
Coronaviruses seem to typically cause signs and symptoms
of arthralgia and myalgia.
42
(Zacharias H, 2021)
43
(Cui D,
2022) If a patient develops clinical features of inflammatory
arthritis following COVID-19, the diagnostic work-up should
be similar to a patient with new onset rheumatoid arthritis
(RA) in an infection naive patient.
44
(Sapkota H, 2022)
35
Xie Y. Long-term cardiovascular outcomes of COVID-19. Nat Med 28, 583–590 (2022). https://doi.org/10.1038/s41591-022-01689-3
36
Gluckman. ACC Expert Consensus Decision Pathway on Cardiovascular Sequelae of COVID-19 in Adults, 2022. doi: 10.1016/j.jacc.2022.02.003
37
Bowe B. JASN November 2021, 32 (11) 2851-2862; DOI: https://doi.org/10.1681/ASN.2021060734
38
Xie Y. Risks and burdens of incident diabetes in long COVID: a cohort study. Lancet Diabetes Endocrinol. 2022 May;10(5):311-321. doi: 10.1016/S2213-
8587(22)00044-4
39
Wander P. The Incidence of Diabetes Among 2,777,768 Veterans with and Without Recent SARS-CoV-2 Infection. Diabetes Care 1 April 2022; 45 (4): 782–788.
https://doi.org/10.2337/dc21-1686
40
Lerma L. Prevalence of autoantibody responses in acute coronavirus disease 2019 (COVID-19). J Transl Autoimmun, 2020. 10.1016/j.jtauto.2020.100073
41
Derksen V. Onset of rheumatoid arthritis after COVID-19: coincidence or connected? Ann Rheum Dis, 2021. http://dx.doi.org/10.1136/annrheumdis-2021-219859
42
Zacharias H. Rheumatological complications of Covid 19. Autoimmun Rev, 2021. 20(9): 10.1016/j.autrev.2021.102883
43
Cui D. Rheumatic Symptoms Following Coronavirus Disease 2019 (COVID-19): A Chronic Post–COVID-19 Condition, Open Forum Infectious Diseases, Volume
9, Issue 6, June 2022, ofac170, https://doi.org/10.1093/ofid/ofac170
44
Sapkota H. Long COVID from rheumatology perspective - a narrative review. Clin Rheumatol, 2022. 41(2): p. 337-348. 10.1007/s10067-021-06001-1
Epidemiology
Recommendation
17
APPENDIX A: OLFACTORY TRAINING
This section provides details about the Olfactory Training at the Veterans Affairs Otolaryngology
Department in Atlanta, GA
1. Actively smell or sniff
2. Four familiar scents
3. Think about your memory of the odor while smelling the odor
4. In random order, sniff for a total of 20-60 seconds for each odor
5. Rest for 30 seconds between each scent
6. Sniff the four scents, 2 to 4 times a day, each, for 24-36 weeks
7. Change the odorants used every 12 weeks
The stimulating smells used are often in commercially available smell kits are often selected from major
smell categories, such as aromatic, flowery, fruity, and resinous.

18
APPENDIX B: FATIGUE AND ACTIVITY INTOLERANCE
This section provides details on the titrated return to individualized activity program including baseline
activity tolerance and paced graded activity.
Titrated Return to Individualized Activity Program
Mild Fatigue: Patients should try to continue all household and community activities that have been
tolerated with a slow return to higher intensity activities and exercise. The “rule of tens” may be helpful.
Moderate Fatigue: It’s recommended to continue household and limited community activities that have
been tolerated. Patients should begin an activity or aerobic exercise program with exertion at sub-
maximal levels (rate of perceived exertion (RPE) 9–11/Very Light-Light).
Severe Fatigue: Severe fatigue or significant post-exertional malaise: Continue any house-hold
activities that have been tolerated without symptom exacerbation. Patients can begin a physical activity
program, which should initially consist of upper and lower extremity stretching and light muscle
strengthening before any targeted aerobic activity. Once tolerated, patients can begin an activity or
aerobic exercise program at submaximal levels, RPE 7–9/Extremely to Very Light.
Activities or exercise can be slowly advanced as the patient tolerates in all levels of fatigue. Harm can
be done if patients are pushed beyond what they can tolerate. If signs and symptoms worsen after
increasing activity level in any severity of fatigue (which may be delayed until the evening and/or days
after the activity/exercise session), patient should return to prior tolerated level of activity.
Baseline Activity Tolerance
Measure how long low intensity tasks such as walking, light exercises, and daily activities (e.g., self-
care tasks, light housework) can be engaged in without resulting in immediate or delayed fatigue. Do
this for both “good” and “bad” days for 3 days. Average the three trials and subtract a fifth. The result
with be your activity duration starting point.
Table 1: Activity Duration Baseline
Time 1
Time 2
Time 3
Average
4/5 Average
19 min
17 min
21 min
19 min
15 min
Paced Graded Activity
Start with low intensity daily activities. Keep in mind that patients with different symptom severity will be
able to tolerate different levels of activity. Transition over the course of days to months based on
response, with a 10-20% increase every 1-2 weeks being a common marker. Work to keep a consistent
schedule vs adapting day by day based on symptom levels or life demands. It is important to remember
to not try to over-exert oneself on days they are feeling well, as this may worsen signs and symptoms.
To increase activity level over time:
1. First focus on increasing the FREQUENCY of activity
2. Then work to increase the DURATION of activity
3. When able to engage reliably in low intensity activity consistently throughout the day without
flares of fatigue, then moderate and eventually higher INTENSITY activity can be added.

19
The following table gives an example of what this could look like in practice. Help your Veteran to set
their own starting point and progression based on their activity tolerance and response.
Table 2: Pace Graded Activity
Week
Intensity
Activity Duration (min)
Rest Duration (min)
1-2
Low
15
50
3-4
Low
15
40
5-6
Low
15
30
7-8
Low
20
30
9-10
Low
25
25
11-12
Low
30
20
13-14
Low
35
15
15-16
Low ; Moderate
30 ; 5
15
17-18
Low ; Moderate
25 ; 10
15
19-20
Low ; Moderate
20; 15
15

20
APPENDIX C: 30 SECOND SIT TO STAND TEST
The 30 second chair stand test (30CST) is a measurement that assess functional lower extremity
strength in older adults. It is part of the Fullerton Functional Fitness Test Battery. This test was
developed to overcome the floor effect of the 5 or 10 repetition sit to stand test in older adults.
Instructions
1. Instruct the patient:
a. Sit in the middle of the chair.
b. Place your hands on the opposite shoulder crossed, at the wrists.
c. Keep your feet flat on the floor.
d. Keep your back straight and keep your arms against your chest.
e. On “Go,” rise to a full standing position, then sit back down again.
f. Repeat this for 30 seconds.
2. On the word “Go,” begin timing. If the patient must use their arms to stand, stop the test. Record
“0” for the number and score.
3. Count the number of times the patient comes to a full standing position in 30 seconds. If the
patient is over halfway to a standing position when 30 seconds have elapsed, count it as a
stand.
4. Record the number of times the patient stands in 30 seconds.

21
APPENDIX D: COMPOSITE AUTONOMIC SYMPTOM
SCORE (COMPASS 31)
COMPASS 31 is a quantitative measure of autonomic symptoms.
Assessment
1. In the past year, have you ever felt faint, dizzy, “goofy”, or had difficulty thinking soon after standing
up from a sitting or lying position?
1 Yes
2 No (if you marked No, please skip to question 5)
2. When standing up, how frequently do you get these feelings or symptoms?
1 Rarely
2 Occasionally
3 Frequently
4 Almost Always
3. How would you rate the severity of these feelings or symptoms?
1 Mild
2 Moderate
3 Severe
4. In the past year, have these feelings or symptoms that you have experienced:
1 Gotten much worse
2 Gotten somewhat worse
3 Stayed about the same
4 Gotten somewhat better
5 Gotten much better
6 Completely gone
5. In the past year, have you ever noticed color changes in your skin, such as red, white, or purple?
1 Yes
2 No (if you marked No, please skip to question 8)
6. What parts of your body are affected by these color changes? (Check all that apply)
1 Hands
2 Feet
7. Are these changes in your skin color:
1 Getting much worse
2 Getting somewhat worse
3 Staying about the same
4 Getting somewhat better
5 Getting much better
6 Completely gone
8. In the past 5 years, what changes, if any, have occurred in your general body sweating?
1 I sweat much more than I used to
2 I sweat somewhat more than I used to
3 I haven’t noticed any changes in my sweating
4 I sweat somewhat less than I used to
5 I sweat much less than I used to
22
9. Do your eyes feel excessively dry?
1 Yes
2 No
10. Does your mouth feel excessively dry?
1 Yes
2 No
11. For the symptom of dry eyes or dry mouth that you have had for the longest period of time, is this
symptom:
1 I have not had any of these symptoms
2 Getting much worse
3 Getting somewhat worse
4 Staying about the same
5 Getting somewhat better
6 Getting much better
7 Completely gone
12. In the past year, have you noticed any changes in how quickly you get full when eating a meal?
1 I get full a lot more quickly now than I used to
2 I get full more quickly now than I used to
3 I haven’t noticed any change
4 I get full less quickly now than I used to
5 I get full a lot less quickly now than I used to
13. In the past year, have you felt excessively full or persistently full (bloated feeling) after a meal?
1 Never
2 Sometimes
3 A lot of the time
14. In the past year, have you vomited after a meal?
1 Never
2 Sometimes
3 A lot of the time
15. In the past year, have you had a cramping or colicky abdominal pain?
1 Never
2 Sometimes
3 A lot of the time
16. In the past year, have you had any bouts of diarrhea?
1 Yes
2 No (if you marked No, please skip to question 20)
17. How frequently does this occur?
1 Rarely
2 Occasionally
3 Frequently ____________ times per month
4 Constantly
18. How severe are these bouts of diarrhea?
1 Mild
2 Moderate
3 Severe
23
19. Are your bouts of diarrhea getting:
1 Much worse
2 Somewhat worse
3 Staying the same
4 Somewhat better
5 Much better
6 Completely gone
20. In the past year, have you been constipated?
1 Yes
2 No (if you marked No, please skip to question 24)
21. How frequently are you constipated?
1 Rarely
2 Occasionally
3 Frequently ____________ times per month
4 Constantly
22. How severe are these episodes of constipation?
1 Mild
2 Moderate
3 Severe
23. Is your constipation getting:
1 Much worse
2 Somewhat worse
3 Staying the same
4 Somewhat better
5 Much better
6 Completely gone
24. In the past year, have you ever lost control of your bladder function?
1 Never
2 Occasionally
3 Frequently ____________ times per month
4 Constantly
25. In the past year, have you had difficulty passing urine?
1 Never
2 Occasionally
3 Frequently ____________ times per month
4 Constantly
26. In the past year, have you had trouble completely emptying your bladder?
1 Never
2 Occasionally
3 Frequently ____________ times per month
4 Constantly
27. In the past year, without sunglasses or tinted glasses, has bright light bothered your eyes?
1 Never (if you marked Never, please skip to question 29)
2 Occasionally
3 Frequently
4 Constantly
24
28. How severe is this sensitivity to bright light?
1 Mild
2 Moderate
3 Severe
29. In the past year, have you had trouble focusing your eyes?
1 Never (if you marked Never, please skip to question 31)
2 Occasionally
3 Frequently
4 Constantly
30. How severe is this focusing problem?
1 Mild
2 Moderate
3 Severe
31. Is the most troublesome symptom with your eyes (i.e. sensitivity to bright light or trouble focusing)
getting:
1 I have not had any of these symptoms
2 Much worse
3 Somewhat worse
4 Staying about the same
5 Somewhat better
6 Much better
7 Completely gone

25
Raw Domain Scoring
The raw domain scores are derived by adding the points for the questions comprising each domain.
Where an answer to a question is not assigned a point, the score for that answer is zero.
Final Domain Scoring
The final domain scores are generated by multiplying the raw score with a weight index. The total score
is the sum of all domain scores.
Domains and Number of Questions Retained Based on Exploratory Factor Analysis and Clinical
Revisions as Used in the Final Instrument (COMPASS 31)
a
Domain
No. of
Questions
Max raw score
Weighting
factor
Max weighted
score
Cronbach
α
Orthostatic Intolerance
4
10
4.0
40
0.92
Vasomotor
3
6
0.8333333
5
0.91
Secretomotor
4
7
2.1428571
15
0.48
Gastrointestinal
b
12
28
0.8928571
25
0.78
Bladder
3
9
1.1111111
10
0.62
Pupillomotor
5
15
0.3333333
5
0.84
Total
31
75
100
a
Appropriate weighting factors for each domain result in appropriately balanced autonomic domains
and a total score between 0 and 100. Max = maximum.
b
Combines former constipation, diarrhea, and gastroparesis domains into one domain.

26
RESOURCES
Veteran Whole Health Library
https://www.va.gov/WHOLEHEALTHLIBRARY/
Veteran Whole Health Education Handouts
https://www.va.gov/WHOLEHEALTH/veteran-handouts/index.asp
Veterans Health Library
www.veteranshealthlibrary.va.gov
Veterans Crisis Line
https://www.veteranscrisisline.net
American Academy of Physical Medicine and Rehabilitation (AAPM&R)
https://www.aapmr.org/members-publications/covid-19/pasc-guidance
https://www.aapmr.org/members-publications/icd-10-codes
National Center for Health Promotion and Disease Prevention
www.prevention.va.gov
National Institute for Health and Care Excellence (NICE), UK
https://www.nice.org.uk/guidance/ng188
UW Integrative Health, Department of Family Medicine and Community Health
https://www.fammed.wisc.edu/integrative/resources/

27
ADDITIONAL REFERENCES
• Addison AB, Wong B, Ahmed T, Macchi A, Konstantinidis I, Huart C, et al. Clinical Olfactory
Working Group consensus statement on the treatment of postinfectious olfactory dysfunction. The
Journal of Allergy and Clinical Immunology, 2021 May;147(5):1704-1719. doi:
10.1016/j.jaci.2020.12.641
• Alaparthi GK, Augustine AJ, Anand R, Mahale A. Comparison of Diaphragmatic Breathing Exercise,
Volume and Flow Incentive Spirometry, on Diaphragm Excursion and Pulmonary Function in
Patients Undergoing Laparoscopic Surgery: A Randomized Controlled Trial. Journal of Minimally
Invasive Surgery. 2016;2016:1967532. doi: 10.1155/2016/1967532
• American Academy of Physical Medicine and Rehabilitation (AAPM&R) (2022). PASC Consensus
Guidance. https://www.aapmr.org/members-publications/covid-19/pasc-guidance
• Andres S, Pevny S, Ziegenhagen R, et al. Safety aspects of the use of quercetin as a dietary
supplement. Molecular Nutrition & Food Research. 2018;62(1). doi:10.1002/mnfr.201700447
• Anton SD, Embry C, Marsiske M, et al. Safety and metabolic outcomes of resveratrol
supplementation in older adults: results of a twelve-week, placebo-controlled pilot study.
Experimental Gerontology. 2014;57:181-187. doi:10.1016/j.exger.2014.05.015
• Asadi-Pooya AA, Akbari A, Emami A, Lotfi M, Rostamihosseinkhani M, Nemati H, Barzegar Z,
Kabiri M, Zeraatpisheh Z, Farjoud-Kouhanjani M, Jafari A, Sasannia F, Ashrafi S, Nazeri M, Nasiri
S, Shahisavandi M. Risk Factors Associated with Long COVID Syndrome: A Retrospective Study.
Iranian Journal of Medical Sciences. 2021 Nov;46(6):428-436. doi: 10.30476/ijms.2021.92080.2326
• Aziz M, Goyal H, Haghbin H, Lee-Smith WM, Gajendran M, Perisetti A. The Association of "Loss of
Smell" to COVID-19: A Systematic Review and Meta-Analysis. American Journal of the Medical
Sciences. 2021 Feb;361(2):216-225. doi: 10.1016/j.amjms.2020.09.017
• Bellan M, Soddu D, Balbo PE, Baricich A, Zeppegno P, Avanzi GC, et al. Respiratory and
Psychophysical Sequelae Among Patients With COVID-19 Four Months After Hospital Discharge.
JAMA Network Open. 2021 Jan 4;4(1): doi: 10.1001/jamanetworkopen.2020.36142
• Berman AY, Motechin RA, Wiesenfeld MY, Holz MK. The therapeutic potential of resveratrol: a
review of clinical trials. Precision Oncology - Nature. 2017;1:35. doi:10.1038/s41698-017-0038-6
• Bowe B, Xie Y, Xu E, Al-Aly Z. Kidney Outcomes in Long COVID. Journal of the American Society
of Nephrology. Nov 2021, 32 (11) 2851-2862; doi: 10.1681/ASN.2021060734
• Cavanaugh AM, Spicer KB, Thoroughman D, Glick C, Winter K. Reduced Risk of Reinfection with
SARS-CoV-2 After COVID-19 Vaccination — Kentucky, May–June 2021. Morbidity and Mortality
Weekly Report. 2021 Aug 13;70(32):1081-1083. doi: 10.15585/mmwr.mm7032e1
• Centers for Disease Control and Prevention (CDC). Long COVID or Post-COVID Conditions. July
11, 2022. https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html
• Chainani-Wu N. Safety and anti-inflammatory activity of curcumin: a component of tumeric
(Curcuma longa). Journal of Alternative and Complementary Medicine. 2003;9(1):161-168.
doi:10.1089/107555303321223035
• Cui D, Wang Y, Huang L, Gu X, Huang Z, Mu S, Wang C, Cao B. Rheumatic Symptoms Following
Coronavirus Disease 2019 (COVID-19): A Chronic Post–COVID-19 Condition, Open Forum
Infectious Diseases, Volume 9, Issue 6, June 2022, ofac170, https://doi.org/10.1093/ofid/ofac170

28
• Derksen VFAM, Kissel T, Lamers-Karnebeek FBG, et al. Onset of rheumatoid arthritis after COVID-
19: coincidence or connected? Annals of the Rheumatic Diseases 2021;80:1096-
1098.:http://dx.doi.org/10.1136/annrheumdis-2021-219859
• Douaud G, Lee S, Alfaro-Almagro F, Arthofer C, Wang C, McCarthy P, et al. SARS-CoV-2 is
associated with changes in brain structure in UK Biobank. Nature. 2022 Apr;604(7907):697-707.
doi: 10.1038/s41586-022-04569-5
• European Food Safety Authority, Panel on Dietetic Products, Nutrition and Allergies, 2016.
Scientific opinion on the safety of synthetic trans-resveratrol as a novel food pursuant to Regulation
(EC) No 258/97. EFSA Journal 2016;14(1):4368, 30 pp. doi:10.2903/j.efsa.2016.4368
• Favero G, Franceschetti L, Bonomini F, Rodella LF, Rezzani R. Melatonin as an anti-inflammatory
agent modulating inflammasome activation. International Journal of Endocrinology.
2017;2017:1835195. doi:10.1155/2017/1835195
• Fernández-de-Las-Peñas C, Navarro-Santana M, Gómez-Mayordomo V, Cuadrado ML, García-
Azorín D, Arendt-Nielsen L, Plaza-Manzano G. Headache as an acute and post-COVID-19
symptom in COVID-19 survivors: A meta-analysis of the current literature. European Journal of
Neurology. 2021 Nov;28(11):3820-3825. doi: 10.1111/ene.15040
• Fernández-de-Las-Peñas C, Martín-Guerrero JD, Pellicer-Valero ÓJ, Navarro-Pardo E, Gómez-
Mayordomo V, Cuadrado ML, Arias-Navalón JA, Cigarán-Méndez M, Hernández-Barrera V, Arendt-
Nielsen L. Female Sex Is a Risk Factor Associated with Long-Term Post-COVID Related-
Symptoms but Not with COVID-19 Symptoms: The LONG-COVID-EXP-CM Multicenter Study.
Journal of Clinical Medicine. 2022 Jan 14;11(2):413. doi: 10.3390/jcm11020413
• Gaudet T, Kligler B. Whole Health in the Whole System of the Veterans Administration: How Will
We Know We Have Reached This Future State? Journal of Alternative and Complementary
Medicine. 2019 Mar;25(S1):S7-S11. doi: 10.1089/acm.2018.29061.gau
• Gluckman TJ, Bhave NM, Allen LA, Chung EH, Spatz ES, Ammirati E, et al. 2022 ACC Expert
Consensus Decision Pathway on Cardiovascular Sequelae of COVID-19 in Adults: Myocarditis and
Other Myocardial Involvement, Post-Acute Sequelae of SARS-CoV-2 Infection, and Return to Play:
A Report of the American College of Cardiology Solution Set Oversight Committee. Journal of the
American College of Cardiology. 2022 May 3;79(17):1717-1756. doi: 10.1016/j.jacc.2022.02.003
• Goërtz YMJ, Van Herck M, Delbressine JM, Vaes AW, Meys R, Machado FVC, et al. Persistent
symptoms 3 months after a SARS-CoV-2 infection: the post-COVID-19 syndrome? European
Respiratory Society (ERS) Open Research. 2020 Oct 26;6(4):00542-2020.
doi:10.1183/23120541.00542-2020
• Hopkins C, Alanin M, Philpott C, et al. Management of new onset anosmia during the COVID
pandemic - BRS Consensus Guidelines. Authorea. May 22, 2020.
doi:10.22541/au.159015263.38072348
• Hu J, Webster D, Cao J, Shao A. The safety of green tea and green tea extract consumption in
adults – results of a systematic review. Regulatory Toxicology and Pharmacology. 2018;95:412-
433. doi:10.1016/j.yrtph.2018.03.019
• Hummel T, Heilmann S, Hüttenbriuk KB. Lipoic acid in the treatment of smell dysfunction following
viral infection of the upper respiratory tract. Laryngoscope. 2002 Nov;112(11):2076-80.
doi:10.1097/00005537-200211000-00031.

29
• Institute for Functional Medicine (IFM). COVID-19 Functional Medicine Resources: The Functional
Medicine Approach to COVID-19: Virus-Specific Nutraceutical and Botanical Agents. October 15,
2021. https://www.ifm.org/news-insights/the-functional-medicine-approach-to-COVID-19-virus-
specific-nutraceutical-and-botanical-agents/
• Isomura T, Suzuki S, Origasa H, et al. Liver-related safety assessment of green tea extracts in
humans: a systematic review of randomized controlled trials. Published correction appears in
European Journal of Clinical Nutrition. 2016;70(11):1340
• Jutant EM, Meyrignac O, Beurnier A, Jaïs X, Pham T, Morin L, et al. Respiratory symptoms and
radiological findings in post-acute COVID-19 syndrome. European Respiratory Society (ERS) Open
Research. 2022 Apr 19;8(2):00479-2021. doi: 10.1183/23120541.00479-2021
• Kattar N, Do TM, Unis GD, Migneron MR, Thomas AJ, McCoul ED. Olfactory Training for Postviral
Olfactory Dysfunction: Systematic Review and Meta-analysis. Otolaryngology–Head and Neck
Surgery. 2021 Feb;164(2):244-254. doi: 10.1177/0194599820943550
• Krejci, Laura P. MSW; Carter, Kennita MD; Gaudet, Tracy MD Whole Health, Medical Care:
December 2014 - Volume 52 - Issue - p S5-S8, doi: 10.1097/MLR.0000000000000226
• Kronenbuerger M, Pilgramm M. Olfactory Training. StatPearls; January 3, 2022.
https://www.ncbi.nlm.nih.gov/books/NBK567741/
• Kunnumakkara AB, Bordoloi D, Padmavathi G, et al. Curcumin, the golden nutraceutical:
multitargeting for multiple chronic diseases. British Journal of Pharmacology. 2017;174(11):1325-
1348. doi:10.1111/bph.13621
• Leite Pacheco R, de Oliveira Cruz Latorraca C, Adriano Leal Freitas da Costa A, Luiza Cabrera
Martimbianco A, Vianna Pachito D, Riera R. Melatonin for preventing primary headache: a
systematic review. International Journal of Clinical Practice. 2018;72 (7):e13203.
doi:10.1111/ijcp.13203
• Lerma LA, Chaudhary A, Bryan A, Morishima C, Wener MH, Fink SL. Prevalence of autoantibody
responses in acute coronavirus disease 2019 (COVID-19). Journal of Translational Autoimmunity.
2020;3:100073. doi: 10.1016/j.jtauto.2020.100073
• Mehrabani S, Askari G, Miraghajani M, Tavakoly R, Arab A. Effect of coenzyme Q10
supplementation on fatigue: A systematic review of interventional studies. Complementary
Therapies in Medicine. 2019 Apr;43:181-187. doi: 10.1016/j.ctim.2019.01.022
• McDermott MM, Leeuwenburgh C, Guralnik JM, et al. Effect of resveratrol on walking performance
in older people with peripheral artery disease: the RESTORE randomized clinical trial. JAMA
Cardiology. 2017;2(8):902-907. doi:10.1001/jamacardio.2017.0538
• Menegazzi M, Campagnari R, Bertoldi M, Crupi R, Di Paola R, Cuzzocrea S. Protective effect of
epigallocatechin-3-gallate (EGCG) in diseases with uncontrolled immune activation: could such a
scenario be helpful to counteract COVID-19? International Journal of Molecular Sciences.
2020;21(14):5171. doi:10.3390/ijms21145171
• Mytinger M, Nelson RK, Zuhl M. Exercise Prescription Guidelines for Cardiovascular Disease
Patients in the Absence of a Baseline Stress Test. Journal of Cardiovascular Development and
Disease. 2020 Apr 27;7(2):15. doi: 10.3390/jcdd7020015.
• Nalbandian, A., Sehgal, K., Gupta, A. et al. Post-acute COVID-19 syndrome. Nature Medicine 27,
601–615 (2021). https://doi.org/10.1038/s41591-021-01283-z

30
• National Institute for Health and Care Excellence (NICE). COVID-19 rapid guideline: managing the
longterm effects of COVID-19. January 3,2022.
https://www.nice.org.uk/guidance/ng188/resources/covid19-rapid-guideline-managing-the-longterm-
effects-of-covid19-pdf-51035515742
• Oketch-Rabah HA, Roe AL, Rider CV, et al. United States Pharmacopeia (USP) comprehensive
review of the hepatotoxicity of green tea extracts. Toxicology reports. 2020;7:386-402.
doi:10.1016/j.toxrep.2020.02.008
• Pelà G, Goldoni M, Solinas E, Cavalli C, Tagliaferri S, Ranzieri S, Frizzelli A, Marchi L, Mori PA,
Majori M, Aiello M, Corradi M, Chetta A. Sex-Related Differences in Long-COVID-19 Syndrome.
Journal of Womens Health (Larchmt). 2022 May;31(5):620-630. doi: 10.1089/jwh.2021.0411
• Premraj L, Kannapadi NV, Briggs J, Seal SM, Battaglini D, Fanning J, et al. Mid and long-term
neurological and neuropsychiatric manifestations of post-COVID-19 syndrome: A meta-analysis.
Journal of the Neurological Sciences. 2022 Mar 15;434:120162. doi: 10.1016/j.jns.2022.120162
• Saenger U, Fumal A, Magis D, Seidel L, Agosti RM, Schoenen J. Efficacy of coenzyme Q10 in
migraine prophylaxis: a randomized controlled trial. Neurology. 2005 Feb 22;64(4):713-5. doi:
10.1212/01.WNL.0000151975.03598.ED
• Sapkota, H. a. (2022). Long COVID from rheumatology perspective - a narrative review. Clinical
Rheumatology, 41(2). doi:10.1007/s10067-021-06001-1
• Sarma DN, Barrett ML, Chavez ML, et al. Safety of green tea extracts: a systematic review by the
US Pharmacopeia. Drug Safety. 2008;31(6):469-484. doi:10.2165/00002018-200831060-00003
• Shoskes DA, Zeitlin SI, Shahed A, Rajfer J. Quercetin in men with category III chronic prostatitis: a
preliminary prospective, double-blind, placebo-controlled trial. Urology. 1999;54(6):960-963.
doi:10.1016/s0090-4295(99)00358-1
• Sletten DM, Suarez GA, Low PA, Mandrekar J, Singer W. COMPASS 31: a refined and abbreviated
Composite Autonomic Symptom Score. Mayo Clinic Proceedings. 2012 Dec;87(12):1196-201. doi:
10.1016/j.mayocp.2012.10.013
• Sorokowska A, Drechsler E, Karwowski M, Hummel T (March 2017). "Effects of olfactory training: a
meta-analysis". Rhinology. 55 (1): 17–26. doi:10.4193/Rhin16.195
• Stavem K, G. W. (2021, Feb 19). Prevalence and Determinants of Fatigue after COVID-19 in Non-
Hospitalized Subjects: A Population-Based Study. International Journal of Environmental Research
and Public Health, 18(4). doi:10.3390/ijerph18042030
• Stella, A. B., Furlanis, G., Frezza, N. A., Valentinotti, R., Ajcevic, M., & Manganotti, P. (2022).
Autonomic dysfunction in post-COVID patients with and without neurological symptoms: a
prospective multidomain observational study. Journal of Neurology, 269(2), 587-596.
doi:10.1007/s00415-021-10735-y
• Taquet M, Luciano S, Geddes JR, Harrison PJ. Bidirectional associations betweenCOVID-19 and
psychiatric disorder: retrospective cohort studies of 62,354 COVID-19 cases in the USA. Lancet
Psychiatry. 2021 Feb;8(2):130-140. doi: 10.1016/S2215-0366(20)30462-4
• Turner RS, Thomas RG, Craft S, et al. A randomized, double-blind, placebo-controlled trial of
resveratrol for Alzheimer disease. Neurology. 2015;85(16):1383-1391.
doi:10.1212/WNL.0000000000002035

31
• Vehar S, Boushra M, Ntiamoah P, Biehl M. Update to post-acute sequelae of SARS-CoV-2
infection: Caring for the 'long-haulers'. Cleveland Clinic Journal of Medicine. 2021 Oct 8. doi:
10.3949/ccjm.88a.21010-up
• Wander P, Lowy E, Beste LA, Tulloch-Palomino L, Korpak A, Peterson AC, et al. The Incidence of
Diabetes Among 2,777,768 Veterans With and Without Recent SARS-CoV-2 Infection. Diabetes
Care 1 April 2022; 45 (4): 782–788. https://doi.org/10.2337/dc21-1686
• Whitaker, M., Elliott, J., Chadeau-Hyam, M. et al. Persistent COVID-19 symptoms in a community
study of 606,434 people in England. Nature Communication 13, 1957 (2022).
https://doi.org/10.1038/s41467-022-29521-z
• Wirtz PH, Spillmann M, Bärtschi C, Ehlert U, von Känel R. Oral melatonin reduces blood
coagulation activity: a placebo-controlled study in healthy young men. Journal of Pineal Research.
2008;44(2):127-133. doi:10.1111/j.1600-079X.2007.00499.x
• Xie, Y., Bowe, B. & Al-Aly, Z. Burdens of post-acute sequelae of COVID-19 by severity of acute
infection, demographics and health status. Nature Communication. 12, 6571 (2021).
https://doi.org/10.1038/s41467-021-26513-3
• Xie Y, Al-Aly Z. Risks and burdens of incident diabetes in long COVID: a cohort study. Lancet
Diabetes & Endocrinology. 2022 May;10(5):311-321. doi: 10.1016/S2213-8587(22)00044-4.
• Xie, Y., Xu, E., Bowe, B. et al. Long-term cardiovascular outcomes of COVID-19. Nature Medicine
28, 583–590 (2022). https://doi.org/10.1038/s41591-022-01689-3
• Yong MS, Lee HY, Lee YS. Effects of diaphragm breathing exercise and feedback breathing
exercise on pulmonary function in healthy adults. Journal of Physical Therapy Science. 2017
Jan;29(1):85-87. doi: 10.1589/jpts.29.85
• Yoo SM, Liu TC, Motwani Y, Sim MS, Viswanathan N, Samras N, et al. Factors Associated with
Post-Acute Sequelae of SARS-CoV-2 (PASC) After Diagnosis of Symptomatic COVID-19 in the
Inpatient and Outpatient Setting in a Diverse Cohort. Journal of General Internal Medicine. 2022
Jun;37(8):1988-1995. doi: 10.1007/s11606-022-07523-3
• Younes M, Aggett P, Aguilar F, et al. Scientific opinion on the safety of green tea catechins.
European Food Safety Authority Journal. 2018;16(4):e05239. doi:10.2903/j.efsa.2018.5239
• Zabetakis I, Lordan R, Norton C, Tsoupras A. COVID-19: The Inflammation Link and the Role of
Nutrition in Potential Mitigation. Nutrients. 2020 May 19;12 (5):1466. doi: 10.3390/nu12051466.
• Zacharias, H. e. (2021). Rheumatological complications of Covid 19. Autoimmunity Reviews, 20(9).
doi:10.1016/j.autrev.2021.102883
• Zhang Y, Mei T, Chen Y, Wang L, Jiang L, Liu K, et al. Smell disorders in COVID-19 patients: role
of olfactory training: A protocol for systematic review and meta-analysis. Medicine (Baltimore). 2021
Feb 26;100(8):e24862. doi: 10.1097/MD.0000000000024862
