
Hospital Price Transparency Frequently Asked Questions
(FAQs)
1
This document is designed as a resource for Hospital Price Transparency frequently asked
questions (FAQs).
All FAQs presented in this document are current as of June 6, 2024.
Table of Contents
General Provisions ......................................................................................................................................................... 2
Definitions ............................................................................................................................................................. 6
Public Disclosure Requirements .................................................................................................................................... 9
Machine-Readable File ......................................................................................................................................... 13
Consumer-friendly Display of Shoppable Services ................................................................................................ 19
Monitoring and Penalties for Noncompliance ............................................................................................................. 23
Appeals of Civil Monetary Penalties ............................................................................................................................ 28

Hospital Price Transparency Frequently Asked Questions
(FAQs)
2
General Provisions
What is the legal basis for the Hospital Price Transparency requirements?
Section 1001 of the Patient Protection and Affordable Care Act (Pub. L. 111-148), as amended
by Section 10101 of the Health Care and Education Reconciliation Act of 2010 (Pub. L. 111-152),
amended Title XXVII of the Public Health Service Act (the PHS Act), in part, by adding a new
section 2718(e). Section 2718 of the PHS Act, titled “Bringing Down the Cost of Health Care
Coverage,” requires each hospital operating within the United States (U.S.) for each year to
establish and update and make public a list of the hospital’s standard charges for items and
services provided by the hospital, including for diagnosis-related groups (DRGs) established
under section 1886(d)(4) of the Social Security Act (the Act). Section 2718(b)(3) of the PHS Act
requires the Secretary of the Department of Health and Human Services (Secretary) to
promulgate regulations to enforce the provisions of section 2718 of the PHS Act, and, in so
doing, the Secretary may provide for appropriate penalties. Please refer the discussion starting
at 84 FR 65525.
How does the Secretary require hospitals to make public their standard
charges? What is the intent of this disclosure?
Hospitals are required to make public their standard charges in two ways: (1) as a
comprehensive machine-readable file (MRF); and (2) in a consumer-friendly format. We
codified these requirements at 45 CFR part 180. We believe these two different methods of
making hospital standard charges public are necessary to ensure that such data are available to
consumers of healthcare where and when they are needed, including through data aggregation
methods (for example, via integration into price transparency tools, electronic health records
(EHRs), and consumer apps), and direct availability to healthcare consumers searching for
hospital-specific charge information. Additionally, data can be used specifically by employers,
researchers, and policy officials, and other members of the public to drive competition and help
bring more value to healthcare. Please refer to the discussion starting at 84 FR 65527.
Updated- What changes did CMS make to the Hospital Price Transparency (HPT)
requirements in the CY 2024 OPPS/ASC Final Rule?
In the CY2024 OPPS/ASC final rule with comment period, we finalized proposals to revise
several HPT requirements to advance the agency’s commitment to increasing price
transparency and enforcing compliance. These policies strengthen and streamline our
monitoring and enforcement capabilities; improve access to, and the usability of, hospital
standard charge information; standardize the way hospital’s standard charges are presented;
reducing the compliance burden on hospitals by providing technical guidance for display of
hospital standard charge information; align, where feasible, certain HPT requirements and
processes with requirements and processes we have implemented in the Transparency in

Hospital Price Transparency Frequently Asked Questions
(FAQs)
3
Coverage initiative; and make other modifications to our monitoring and enforcement
capabilities that will, among other things, increase the transparency to the public. Please refer
to 88 FR 81545. Details can be found in the CY 2024 OPPS/ASC HPT Fact Sheet:
https://www.cms.gov/newsroom/fact-sheets/hospital-price-transparency-fact-sheet
Updated- Did CMS make any changes to the shoppable services display
requirements in the CY 2024 OPPS/ASC Final Rule?
No. CMS did not make any changes to the shoppable services display requirements in the CY
2024 OPPS/ASC Final Rule.
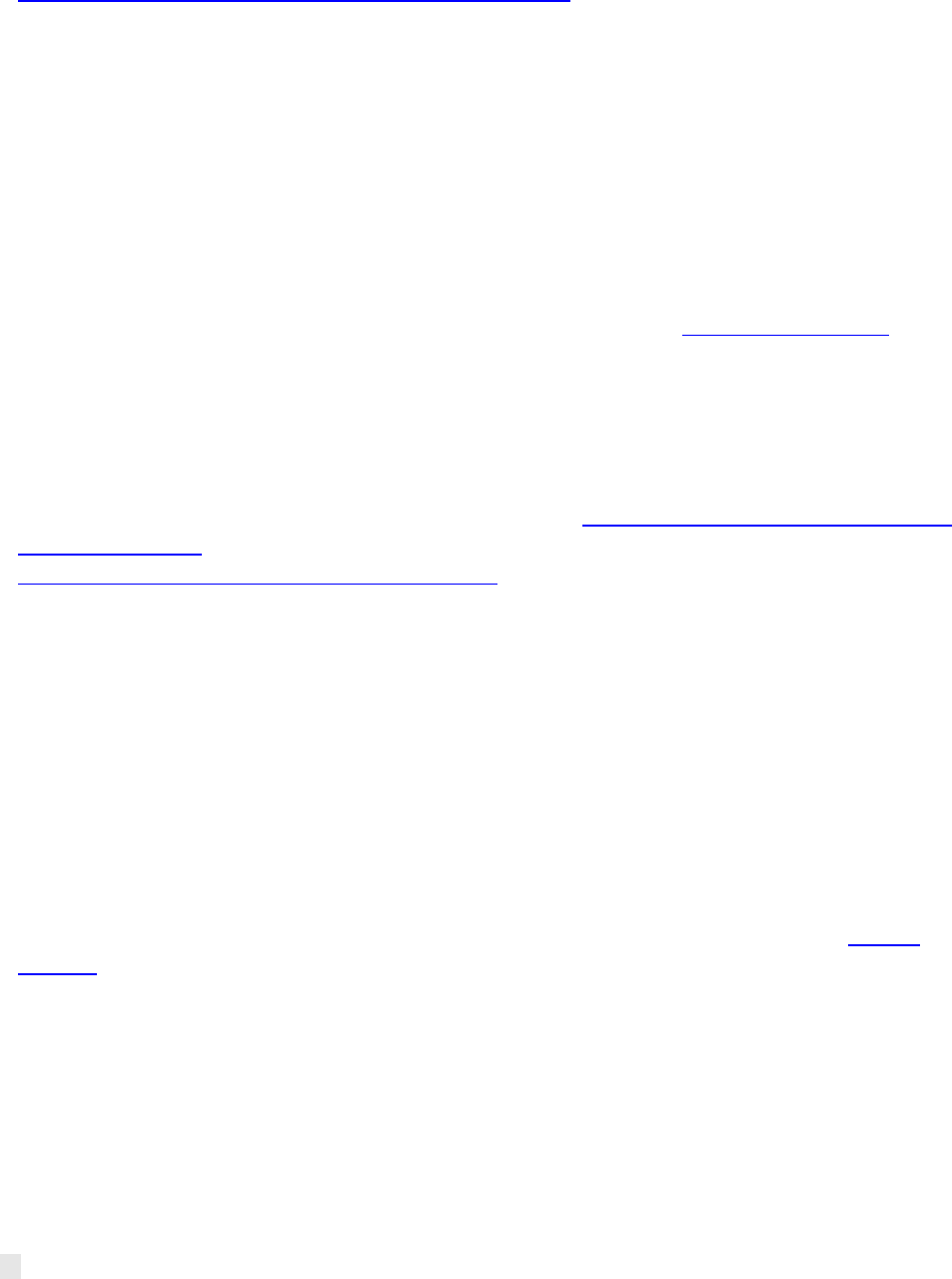
Updated- What is the implementation timeline for the new Hospital Price
Transparency requirements in the CY 2024 OPPS/ASC Final Rule?
CMS established a phased implementation timeline with respect to the hospital price
transparency requirements finalized in the CY 2024 OPPS/ASC Final Rule. The effective date for
hospitals to comply with all the changes to the hospital price transparency regulations at 45 CFR
Part 180 is January 1, 2024. However, we specified a phased approach by which hospitals must
be in compliance with these new requirements. Please refer to the discussion at 88 FR 82109-
82111. Implementation dates for each requirement are detailed in the tables below:
Implementation Timeline for CMS Template Adoption and Encoding Data Elements
Requirement
Regulation cite
Implementation
(Compliance) Date
MACHINE-READBLE FILE INFORMATION
Machine-Readable File Date
45 CFR § 180.50 (b)(2)(i)(B)
July 1, 2024
CMS Template Version
45 CFR § 180.50 (b)(2)(i)(B)
July 1, 2024
HOSPITAL INFORMATION
Hospital Name
45 CFR § 180.50 (b)(2)(i)(A)
July 1, 2024
Hospital Location(s)
45 CFR § 180.50 (b)(2)(i)(A)
July 1, 2024
Hospital Address(es)
45 CFR § 180.50(b)(2)(i)(A)
July 1, 2024
Hospital Licensure Information
45 CFR § 180.50 (b)(2)(i)(A)
July 1, 2024
STANDARD CHARGES
Gross Charge
45 CFR § 180.50 (b)(2)(ii)
July 1, 2024
Discounted Cash
45 CFR § 180.50 (b)(2)(ii)
July 1, 2024
Payer Name
45 CFR § 180.50 (b)(2)(ii)(A)
July 1, 2024
Plan Name
45 CFR § 180.50 (b)(2)(ii)(A)
July 1, 2024
Standard Charge Method
45 CFR § 180.50 (b)(2)(ii)(B)
July 1, 2024
Payer-Specific Negotiated Charge –Dollar Amount
45 CFR § 180.50 (b)(2)(ii)(C)
July 1, 2024
Payer-Specific Negotiated Charge –Percentage
45 CFR § 180.50 (b)(2)(ii)(C)
July 1, 2024
Payer-Specific Negotiated Charge –Algorithm
45 CFR § 180.50 (b)(2)(ii)(C)
July 1, 2024
Estimated Allowed Amount
45 CFR § 180.50 (b)(2)(ii)(C)
January 1, 2025

Hospital Price Transparency Frequently Asked Questions
(FAQs)
4
De-identified Minimum Negotiated Charge
45 CFR § 180.50(b)(2)(ii)
July 1, 2024
De-identified Maximum Negotiated Charge
45 CFR § 180.50(b)(2)(ii)
July 1, 2024
ITEM & SERVICE INFORMATION
General Description
45 CFR § 180.50 (b)(2)(iii)(A)
July 1, 2024
Setting
45 CFR § 180.50 (b)(2)(iii)(B)
July 1, 2024
Drug Unit of Measurement
45 CFR § 180.50 (b)(2)(iii)(C)
January 1, 2025
Drug Type of Measurement
45 CFR § 180.50 (b)(2)(iii)(C)
January 1, 2025
CODING INFORMATION
Billing/Accounting Code
45 CFR § 180.50 (b)(2)(iv)(A)
July 1, 2024
Code Type
45 CFR § 180.50 (b)(2)(iv)(B)
July 1, 2024
Modifiers
45 CFR § 180.50 (b)(2)(iv)(C)
January 1, 2025
Implementation Timeline for Other New Hospital Price Transparency Requirements
Requirement
Regulation cite
Implementation
(Compliance) Date
Good faith effort
45 CFR § 180.50 (a)(3)(i)
January 1, 2024
Affirmation in the machine-readable file
45 CFR § 180.50 (a)(3)(ii)
July 1, 2024
Txt file
45 CFR § 180.50 (d)(6)(i)
January 1, 2024
Footer link
45 CFR § 180.50 (d)(6)(ii)
January 1, 2024
Updated - How does the hospital price transparency initiative support
consumers of healthcare services?
We believe the policies requiring public release of hospital standard charge information are a
necessary and important first step in ensuring transparency in prices of healthcare services for
consumers, however, we recognize that the release of hospital standard charge information is
not itself sufficient to achieve our ultimate price transparency goals. The regulations are
designed to begin to address some of the barriers that limit price transparency, with a goal of
increasing competition among healthcare providers to bring down costs. Competition in the
healthcare industry benefits consumers because it helps contain costs, improve quality, expand
choice, and encourage innovation. Please refer to the discussion at 88 FR 82080 for more
information.
Updated- Where can I find information about other federal price transparency
initiatives?
The hospital price transparency regulations are one tool to address barriers that limit price
transparency. In addition to the hospital price transparency regulations, CMS is also providing
consumers with the tools to access pricing information through their health insurance plans
through the Transparency in Coverage Final Rules (TiC Final Rules). Under the TiC Final Rules,
plans and issuers must make price comparison information available through an internet-based
self-service tool and in paper form, upon request. Under the TiC Final Rules, plans and issuers

Hospital Price Transparency Frequently Asked Questions
(FAQs)
5
must also post pricing information for covered items and services. This pricing information can
be used by third parties, such as researchers and app developers to help consumers better
understand the costs associated with their health care. More information about the
Transparency in Coverage Final Rules can be found at https://www.cms.gov/priorities/key-
initiatives/healthplan-price-transparency.
In addition, the No Surprises Act (NSA) includes additional requirements that relate to price
transparency and protect uninsured and self-pay individuals from unexpectedly large medical
bills. The NSA requires providers and facilities, upon an individual’s scheduling of items or
services, or upon request, to provide a good faith estimate of the expected charges for
furnishing the scheduled item or service and any items or services reasonably expected to be
provided in conjunction with those items and services. Should that estimate be off by more
than $400, patients may be able to dispute the charge through the patient-provider dispute
resolution process. Once implemented, upon receiving a good faith estimate plans and issuers
will be required to send an Advanced Explanation of Benefits to the participant, beneficiary, or
enrollee.
To help consumers understand their rights and protections under the NSA, CMS updated
information and resources on CMS.gov. These updates give consumers who receive unexpected
or high medical bills information on the protections they have and may not be aware of. New
sections help consumers identify what actions are appropriate to their billing situation and
provide tools for them to take next steps. The consumer content can be found at
https://www.cms.gov/medical-bill-rights.
Updated- Does the Hospital Price Transparency regulation require hospitals to
tell me the cost of services prior to receiving care?
The Hospital Price Transparency regulation requires hospitals to make standard charge
information available to the public online in two ways: a machine-readable file and a consumer-
friendly list for a limited set of shoppable services. Although critical for determining an
individual’s out-of-pocket obligation, hospital standard charges do not represent either an
individual’s out-of-pocket obligation or a “guaranteed price.” However, we note that
individualized estimates in dollars may be obtained directly, in many circumstances, from
providers and payers through other Federal price transparency efforts such as those
implementing the No Surprises Act and Transparency in Coverage requirements. As such, we
strongly encourage individual consumers to utilize hospital and payer price estimator and
comparison tools, and to request ‘good faith estimates’ from hospitals and providers to provide
up-front pricing that can be used to dispute final charges that are substantially in excess of the
up-front amounts. Please refer to the discussion at 88 FR 82081.
Updated- I received a hospital bill that doesn’t match the hospital’s standard
charges posted online or what the hospital billing department told me. Can the
CMS Hospital Price Transparency program help me?

Hospital Price Transparency Frequently Asked Questions
(FAQs)
6
Hospital standard charges do not represent either an individual’s out-of-pocket obligation or a
guaranteed price, as they do not factor individual circumstances for each patient. As such, we
strongly encourage individual consumers to utilize hospital and payer price estimator and
comparison tools, and to request ‘good faith estimates’ from hospitals and providers which
may provide up-front pricing that can be used to dispute final charges. Please refer to the
discussion at 88 FR 82081. Learn more about the protections that apply to you or find an action
plan for your medical bill at https://www.cms.gov/medical-bill-rights.
Will hospitals be able to apply for a hardship waiver or exception to meeting the
Hospital Price Transparency requirements?
No. The Hospital Price Transparency Final Rule contains no provisions that address waivers or
hardship exemptions.
Definitions
How is a hospital defined under the Hospital Price Transparency Final Rule?
Does the rule apply to Critical Access Hospitals (CAHs), other small or rural
hospitals, state owned/operated institutions, Rural Emergency Hospitals (REHs),
and non- acute hospitals such as inpatient psychiatric hospitals and inpatient
rehabilitation facilities (IRFs)?
Under 45 CFR § 180.20, hospital means an institution, in any State in which State or applicable
local law provides for the licensing of hospitals, which is licensed as a hospital pursuant to such
law or is approved, by the agency of such State or locality responsible for licensing hospitals, as
meeting the standards established for such licensing. For purposes of this definition, a State
includes each of the several States, the District of Columbia, Puerto Rico, the Virgin Islands,
Guam, American Samoa, and the Northern Mariana Islands. All hospital location(s) operating
under the same hospital license (or approval), such as a hospital’s outpatient department
located at an off-campus location (from the main hospital location) operating under the
hospital’s license, are subject to the requirements in this rule. This definition includes all
Medicare-enrolled institutions that are licensed as hospitals (or approved as meeting licensing
requirements) as well as any non-Medicare enrolled institutions that are licensed as a hospital
(or approved as meeting licensing requirements). Given this definition, this rule applies to every
institution that meets the definition of ‘hospital’ established by the Hospital Price Transparency
Final Rule including institutions such as critical access hospitals, specialty hospitals, and state
owned or operated facilities other than those deemed compliant.
Federally owned or operated hospitals (for example, hospitals operated by an Indian Health
Program, the U.S. Department of Veterans Affairs, or the U.S. Department of Defense) that do
not treat the general public, except for emergency services, and whose rates are not subject to

Hospital Price Transparency Frequently Asked Questions
(FAQs)
7
negotiation, are deemed to be in compliance with the requirements for making public standard
charges because their charges for hospital provided services are publicized to their patients in
advance (for example, through the Federal Register). In addition, beginning January 1, 2022,
state forensic hospitals that provide treatment exclusively to individuals who are in the custody
of penal authorities are deemed to be in compliance with 45 CFR Part 180 because such
hospitals are wholly funded through state general funds and treat patients who are not
responsible for the cost of their care in such hospitals. Please refer to the discussion at 86 FR
63950.
Does the Hospital Price Transparency Final Rule apply to hospitals in the State of
Maryland that are subject to global payments set by the Maryland Health
Services Cost Review Commission?
Yes. If your institution meets the definition of ‘hospital’ as defined by the Hospital Price
Transparency Final Rule, then your institution must comply. However, some required standard
charge information may not be applicable to your hospital. For example, under the Hospital
Price Transparency Final Rule, your hospital is obligated to make public the payer-specific
negotiated charges as applicable for each item and service your hospital provides. The term
“payer- specific negotiated charge” is defined as the charge that the hospital has negotiated
with a third-party payer for an item or service. The term “third-party payer” means an entity
that is, by statute, contract, or agreement, legally responsible for payment of a claim for a
healthcare item or service. If your hospital has not negotiated a charge with a third-party payer
for an item or service your hospital provides, then your hospital would not have a “payer-
specific negotiated charge” to display for that item or service.
What standard charges must hospitals make public?
A standard charge means the regular rate established by the hospital for an item or service
provided to a specific group of paying patients. For purposes of complying with the Hospital
Price Transparency Final Rule, this includes five types of standard charges:
1. The gross charge (the charge for an individual item or service that is reflected on a
hospital’s chargemaster, absent any discounts).
2. The discounted cash price (the charge that applies to an individual who pays cash, or
cash equivalent, for a hospital item or service).
3. The payer-specific negotiated charge (the charge that a hospital has negotiated with a
third-party payer for an item or service).
4. The de-identified minimum negotiated charge (the lowest charge that a hospital has
negotiated with all third-party payers for an item or service).
5. The de-identified maximum negotiated charge (the highest charge that a hospital has
negotiated with all third-party payers for an item or service).
Please refer to 45 CFR §180.20.
Hospital Price Transparency Frequently Asked Questions
(FAQs)
8
What hospital “items and services” are included by the Hospital Price
Transparency Final Rule? What is a “service package”?
For purposes of complying with the hospital price transparency requirements, items and
services are all items and services, including individual items and services and service packages,
that could be provided by a hospital to a patient in connection with an inpatient admission or
an outpatient department visit for which a hospital has established a standard charge.
Examples include supplies and procedures, room and board, and use of the facility and other
items (generally described as facility fees), services of employed physicians and non-physician
practitioners (generally reflected as professional charges), and any other item or service for
which a hospital has established a standard charge. Please refer to 45 CFR §180.20.
A service package is an aggregation of individual items and services into a single service for
which the hospital has a single standard charge. “Service packages” may have charges
established on, for example, the basis of a common procedure or patient characteristic, or may
have an established per diem rate that includes all individual items and services furnished
during an inpatient stay. Please refer to 45 CFR §180.20.
The definition of “items and services” includes services of employed physicians
and non-physician practitioners. How does CMS define “employment”?
Given the variation and complexity in employment models and possible contracting
relationships that may exist between hospitals and physicians, we believe it is important to
preserve flexibility for hospitals to identify employed physicians or non-physician practitioners
under their organizational structure, and, for this reason, we declined to codify a definition of
“employment” in the Hospital Price Transparency Final Rule. Please refer to the discussion at
84 FR 65535. One resource that hospitals could consider reviewing for purposes of determining
whether or not a physician or non-physician practitioner is employed by the hospital is:
https://www.irs.gov/newsroom/understanding-employee-vs-contractor-designation.
Do these requirements apply to non-employed physicians and other
practitioners who provide and bill for the same services at the hospital?
No. Services provided by physicians and non-physician practitioners who are not employed by
the hospital are practitioners that are practicing independently, establish their own charges for
services, and receive the payment for their services. Such services, therefore, are not services
“provided by the hospital.”
Do these requirements apply to the services of employed practitioners whose
charges are not found in the hospital chargemaster?

Hospital Price Transparency Frequently Asked Questions
(FAQs)
9
Yes. The Hospital Price Transparency Final Rule does not limit the requirements to only hospital
standard charges that are found within the hospital chargemaster, including standard charges
for items and services provided by practitioners employed by the hospital. The requirements
apply to such charges that may be located elsewhere within the hospital accounting and billing
system, or, in the case of payer-specific negotiated charges, in contracts and rate sheets that are
specific to a particular third-party payer. Please refer to the discussion at 84 FR 65535.
Do the standard charges for services performed by physicians and/or non-
physician practitioners outside the scope of their employment by the hospital
need to be included in the hospital’s display of standard charges?
No, the Hospital Price Transparency Final Rule requires hospitals to post their standard charges
for the items and services they provide. Items and services include, but are not limited to, the
services of employed physicians and non-physician practitioners (generally reflected as
professional charges). They do not include the services that physicians and non-physician
practitioners perform outside the scope of their employment by the hospital.
Public Disclosure Requirements
Updated- Where can I look to find a hospital’s standard charges? Can CMS
provide me with the standard charges for a particular hospital?
Effective January 1, 2024, hospitals must ensure the public website that hosts the machine-
readable file includes a link in the footer on its website, including but not limited to the
homepage, that is labeled “Price Transparency” and links directly to the publicly available web
page that hosts the link to the machine-readable file. Please refer to the discussion at 88 FR
82111. Hospitals’ consumer-friendly displays may be located on the same web page that hosts
the machine-readable file.
We did not propose, nor did we finalize, any requirement for hospitals to submit or upload a
link to their standard charge information to a CMS-specified centralized website. At this time,
we believe such an effort could be unnecessarily duplicative of ongoing State and private sector
efforts to centralize hospital pricing information and potentially confuse consumers who may
reasonably look to a hospital website directly for charge information. Please refer to the
discussion at 84 FR 65561.
Can hospitals choose between displaying standard charges in a machine-
readable format and displaying standard charges for shoppable services in a
consumer-friendly format?
No. Hospitals must make public both of the following: (1) A machine-readable file containing a

Hospital Price Transparency Frequently Asked Questions
(FAQs)
10
list of all standard charges for all items and services as provided in 45 CFR §180.50 and (2) a
consumer- friendly list of standard charges for a limited set of shoppable services as provided in
45 CFR §180.60. Please note that CMS will deem a hospital as having met the second of these
two requirements if the hospital maintains an internet-based price estimator tool that meets
the requirements provided in 45 CFR § 180.60(a)(2).
Updated- Our hospital does not provide a discounted cash price for items and
services. How should we reflect this in the display of standard charge
information in our machine-readable file?
Some hospitals may not have established a discounted cash price for self-pay consumers for the
items and services it provides. In the machine-readable file (MRF), if the hospital has not
established a discounted cash price, the hospital must include the required “standard charge |
discounted cash” data element in their MRF but would not be required to encode any standard
charge information for that data element. If a hospital has established other types of discounts,
such as a financial aid policy for a subset of consumers, the hospital may elect to include
optional data elements, for example, “hospital financial aid policy”, in the CMS MRF template
and encode a hyper link to the policy. For more guidance on how to display and encode an
optional data element, please refer to the technical instructions available at the CMS Hospital
Price Transparency - Data Dictionary GitHub repository at https://github.com/CMSgov/hospital-
price-transparency.
Updated- Some of the hospital items or services we offer do not have an
associated HCPCS or CPT code. Are we required to list such services? If so, what
should be indicated next to the item or service?
Yes. The Hospital Price Transparency Final Rule requires hospitals to disclose the standard
charges for each item or service it provides, therefore, all hospital items and services for which
the hospital has established a standard charge must be listed regardless of whether all the
required corresponding data element values are available. Corresponding common billing and
accounting codes must be included. Please refer to the technical instructions available at the
CMS Hospital Price Transparency - Data Dictionary GitHub repository at
https://github.com/CMSgov/hospital-price-transparency.
Is there a limitation on the number of third-party payers for which we must
make negotiated charges public? For example, does this requirement apply to
contracts with our top payers only?
No. Hospitals are required to list their standard charges, as applicable, including all payer-
specific standard charges, for all items and services with respect to all third-party payers. Please
refer to the discussion at 84 FR 65551.

Hospital Price Transparency Frequently Asked Questions
(FAQs)
11
What is a “base rate” for a service package?
The base rate is the payer-specific charge the hospital has negotiated for a service package.
Base rates for service packages are typically not found in the hospital chargemaster but can be
found in other parts of the hospital’s billing and accounting systems, or in what are known as
‘rate sheets’ found in hospital in-network contracts with their third-party payers. The base rate
is not the final payment or reimbursement rate for the service package received by the hospital
for individual patients.
Updated- My hospital has established a gross charge for an individual item or
service (as found in our chargemaster) but it has not established a payer-specific
negotiated charge for that same item or service. In this case, is my hospital
required to establish a payer-specific negotiated charge for that item or service?
No. The Hospital Price Transparency regulations require hospitals to make public a list of the
standard charges the hospital has established for the items and services it provides and to make
this standard charge information available in a single machine-readable file, as applicable. We
recognize that a hospital may have established one type of standard charge (for example a
gross charge) for a particular item or service without having established other types of standard
charges (for example, a payer-specific negotiated charge with a particular payer/plan) for the
same item or service. Hospitals must ensure each required data element is included in its
machine-readable file and leave blanks where there is no applicable standard charge
information to encode. Follow the technical instructions available at the CMS Hospital Price
Transparency - Data Dictionary GitHub repository at https://github.com/CMSgov/hospital-
price-transparency.
Updated- My hospital has not established or negotiated a standard charge for an
item or service. How should I display items and services for which there is no
standard charge?
Your hospital should only include an item or service in its machine-readable file if your hospital
has established one or more standard charges for it. For more guidance on how to display and
encode your data in the MRF, please refer to the technical instructions available at the CMS
Hospital Price Transparency - Data Dictionary GitHub repository at
https://github.com/CMSgov/hospital-price-transparency.
Updated- My hospital has negotiated a standard charge of $0 for a subset of
items and services, how should I encode charges for the “payer-specific
standard charge: dollar amount” data element in the machine-readable file?
The valid values for the “payer-specific standard charge: dollar amount” data element must be
Hospital Price Transparency Frequently Asked Questions
(FAQs)
12
indicated as a numeric value. the Data Dictionary indicates that all "Numeric" data elements
must be positive numbers. Entering a negative number or "0" will generate a deficiency. If your
hospital has negotiated a $0 dollar amount for a hospital item or service, you should not
encode data in the “payer-specific standard charge: dollar amount” data element and provide
additional context in either the “additional payer notes” or “additional notes” data element,
depending on which CMS Template layout you choose to adopt. For more guidance on how to
display and encode your data in the MRF, please refer to the technical instructions available at
the CMS Hospital Price Transparency - Data Dictionary GitHub repository at
https://github.com/CMSgov/hospital-price-transparency.
If a hospital has not provided a service in the previous 12 months, is it required
to post the standard charge for that service?
Yes. CMS finalized the proposal to define hospital “items and services” to mean all items and
services, including individual items and services and service packages, that could be provided by
a hospital to a patient in connection with an inpatient admission or an outpatient department
visit for which the hospital has established a standard charge. In other words, hospitals must
post the standard charge (as applicable) for each item/service for which the hospital has
established a standard charge. Refer to 45 CFR § 180.20.
Should Medicaid plan rates be considered part of the de-identified minimum
charge and payer-specific charge if a state is a fully managed care Medicaid
state?
Hospitals are required to make public the payer-specific negotiated charges that they have
negotiated with third-party payers, including charges negotiated by third-party payer managed
care plans such as Medicare Advantage plans, Medicaid MCOs, and other Medicaid managed
care plans. Therefore, a state’s Medicaid managed care contracts may fall within this
description, if such managed care contracts include rates negotiated with the hospital. Please
refer to 84 FR 65551 where we finalized our definition of ‘‘third-party payer’’ as an entity that,
by statute, contract, or agreement, is legally responsible for payment of a claim for a healthcare
item or service.
In cases where the hospital has negotiated a payer-specific negotiated charge
based on the Medicare or Medicaid FFS rate, can the hospital simply indicate
that the price of the hospital item/service is set to the Medicare or Medicaid
rate instead of reporting a specific dollar value?
No. The payer-specific negotiated charge is defined for purposes of the Hospital Price
Transparency Final Rule as the charge that a hospital has negotiated with a third-party payer for
an item or service, including a service package, and the hospital should list that standard
charge. For example, if your hospital has negotiated a payer-specific negotiated charge for a

Hospital Price Transparency Frequently Asked Questions
(FAQs)
13
service package that equals 200% of the Medicare FFS reimbursement rate for MS-DRG 123,
then your hospital should determine the Medicare reimbursement rate for DRG 123, multiply it
by 2 and indicate the resulting amount as its payer-specific negotiated charge for that service
package.
We believe displaying payer-specific negotiated rates publicly would violate the
confidentiality clause of the hospital’s contract with our third-party payers. Has
CMS addressed this issue?
Even if a contract between a hospital and a payer contained a provision prohibiting the public
disclosure of its terms, it is our understanding that such contracts typically include exceptions
where a particular disclosure is required by Federal law. Please refer to the discussion at 84 FR
65544.
Machine-Readable File
Updated- What is a ‘machine-readable’ file? What formats are hospitals allowed
to post their machine-readable files in? Are hospitals allowed to post their
machine-readable files in a format other than the ones made available through
the CMS template layout, such as Microsoft Excel, .XML, PDF?
A machine-readable file is a single digital file that is in a machine-readable format. Beginning on
July 1, 2024, the hospital’s machine-readable file must conform to a CMS template layout, data
specifications, and data dictionary. CMS has made the CMS template available in three non-
proprietary formats: CSV “tall”, CSV “wide”, and JSON. Hospitals must make their file available
in one of these templates. Files in Microsoft Excel, .XML, or PDF are not compliant. CMS
strongly recommends hospitals start with one of the template layouts to create your machine-
readable files as opposed to trying to convert an existing machine-readable file to one of the
templates. Refer to 45 CFR § 180.20, 45 CFR § 180.50(c), and the technical instructions available
at the CMS Hospital Price Transparency - Data Dictionary GitHub repository at GitHub -
CMSgov/hospital-price-transparency.
Updated-Where can I find the required CMS templates or more information on
how to encode my hospital’s standard charge information and each of the
required data elements?
CMS has created a GitHub repository to house the required CMS templates, in a CSV “tall”, CSV
“wide” and JSON format, and provides the data dictionary, or technical instruction, on how
hospitals must encode standard charge information into machine-readable files for each
required data element. The CMS Hospital Price Transparency - Data Dictionary GitHub
repository is available at https://github.com/CMSgov/hospital-price-transparency.

Hospital Price Transparency Frequently Asked Questions
(FAQs)
14
Updated- Will changing the order of the CSV headers or JSON attributes in the
CMS templates result in a deficiency or cause my MRF to be considered
noncompliant with the form and manner prescribed by CMS for encoding
standard charge information?
Changing the order of the CSV headers or JSON attributes in the CMS template layouts will not
generate a deficiency. Please refer to the documentation and examples on the CMS Hospital
Price Transparency - Data Dictionary GitHub repository for more information at
https://github.com/CMSgov/hospital-price-transparency.
Updated- My hospital’s machine-readable file update occurs between
publication of the CY 2024 OPPS/ASC Final Rule and July 1, 2024, when use of
the new CMS template is required. Am I required to update my hospital’s
machine-readable file now and again in the new CMS template as of July 1,
2024?
As nalized in the CY2024 OPPS/ASC nal rule, beginning July 1, 2024, all hospitals must adopt a
CMS template and encode in it the hospital’s standard charge informaon in the form and
manner nalized in the CMS Hospital Price Transparency - Data Dictionary GitHub repository
available here https://github.com/CMSgov/hospital-price-transparency. CMS will enforce these
requirements beginning on July 1, 2024.
What updates did CMS make to the accessibility requirements of the machine-
readable file in the CY 2022 OPPS/ASC Final Rule?
As of January 1, 2022, CMS requires that the machine-readable file must be accessible to
automated searches and direct downloads through a link posted on a publicly available website
(45 CFR § 180.50 (d)(3)(iv)). Specific examples of barriers to automated searches and direct
downloads that CMS identified include, but are not limited to, lack of a link for downloading a
single machine-readable file, using ‘‘blocking codes’’ or CAPTCHA, and requiring the user to
agree to terms and conditions or submit other information prior to access. Refer to the
discussion at 86 FR 63951.
Updated- How can my hospital ensure that its machine-readable file is
“prominently displayed”? What requirements must hospitals adopt to improve
automated access to machine-readable files because of the CY 2024
amendments to the Hospital Price Transparency Final Rule?
In the CY 2024 OPPS/ASC Final Rule, CMS finalized the following accessibility requirements,
effective January 1, 2024, the hospital must ensure that the public website it selects to host its

Hospital Price Transparency Frequently Asked Questions
(FAQs)
15
machine-readable file establishes and maintains, in the form and manner specified by CMS:
• A .txt file in the root folder that includes a standardized set of fields including the
hospital location name that corresponds to the machine-readable file, the source
page URL that hosts the machine-readable file, a direct link to the machine-readable
file (the machine-readable file URL), and hospital point of contact information. For
more information, access the Hospital Price Transparency TXT File Frequently Asked
Questions (FAQs).
• A link in the footer on its website, including but not limited to the homepage, that is
labeled “Price Transparency” and links directly to the publicly available web page
that hosts the link to the machine-readable file.
In addition, we recommend that hospitals review and use, as applicable, the HHS Web Standards
and Usability Guidelines (available at https://webstandards.hhs.gov/), which are research-
based and are intended to provide best practices over a broad range of web design and digital
communications issues.
What naming convention should hospitals use when making public the machine-
readable file? How can I find the EIN and associated hospital legal name?
Hospitals must use the following CMS naming convention as specified in the regulations at 45
CFR § 180.50(d)(5) for the machine-readable file:
<ein>_<hospital- name>_standardcharges.[json| |csv] in which the EIN is the Employer
Identification Number of the hospital, followed by the hospital name, followed by
“standardcharges” followed by the hospital’s chosen file format (84 FR 65562).
It is important that you follow the rule’s naming convention. Specifically, hospitals must use the
following schema:
• Write out “standardcharges” as a single word, without capitalization.
• Finish by using. json or .csv as applicable to the CMS Template you have selected.
• Separate the EIN, hospital name, and “standardcharges” by using an underscore:
12345678_example-hospital-name_standardcharges.csv
In addition, hospitals may do the following:
• Exclude dashes from the EIN (use “12345678”, not “12-345678”)
• Use the legal name of the hospital without capitalization and include dashes between
words (use “example-hospital-name”, not “Example Hospital Name”)
• Hospital EINs and legal names can be found using lookups hosted by the IRS
(https://apps.irs.gov/app/eos/) and SEC (https://www.sec.gov/edgar/search/)
We have multiple facilities and locations, each with its own list of standard

Hospital Price Transparency Frequently Asked Questions
(FAQs)
16
charges, functioning under the same EIN and legal name. CMS regulations
require that “Each hospital location operating under a single hospital license (or
approval) that has a different set of standard charges than the other location(s)
operating under the same hospital license (or approval) must separately make
public the standard charges applicable to that location.” In this case, what
naming convention should we use for these machine-readable files?
Hospitals must use the CMS naming convention as specified in the regulations at 45 CFR §
180.50(d)(5) but may also add “-<NPI>” following the EIN (where “#” is the National Provider
Identifier that corresponds to the hospital location). NPIs and hospital names can be found
using this lookup: https://npiregistry.cms.hhs.gov/. For example, “Example Hospital Name”
with EIN of 12345678 has two locations with NPIs of “1011121314” and “1516171819”, each
with its own set of standard charges. This hospital could name its two csv-formatted machine-
readable files as “12345678-1011121314_example-hospital-name_standardcharges.csv” and
“12345678- 1516171819_example-hospital-name_standardcharges.csv”, respectively.
Updated- My hospital establishes the same set of standard charges across all
our 30 locations. Must I list each location in the machine-readable file when
using the CMS Template (effective July 1, 2024)?
Beginning July 1, 2024, hospitals are required to encode the name(s) and address(es) of each
hospital inpatient location and each standalone emergency department in the machine-
readable file. While strongly encouraged, it is not required to encode all outpatient locations.
We note, however, that even though we are making this practical accommodation, hospitals
must still include all standard charge information in the machine-readable file, including
standard charge information for outpatient locations not encoded for this data element. In
other words, this accommodation should not be interpreted to mean that hospitals need not
include the standard charges that apply to outpatient locations that operate under the single
hospital license but whose location names and addresses are not required to be encoded.
Please refer to the discussion at 88 FR 82092.
In the machine-readable file, are hospitals required only to display the payer-
specific negotiated charges for each item/service that is found in the hospital
chargemaster, even when the hospital has negotiated rates with some payers
based on ‘service packages’?
The machine-readable file posted online by the hospital should include not only the items and
services listed in the chargemaster but also list any service packages for which the hospital may
have established a standard charge. For example, some payer-specific negotiated rates are for
‘service packages’ (for example, per diem or based on a procedure). Such ‘service packages’ are
not typically found in the hospital chargemaster which is a list of itemized items and services,

Hospital Price Transparency Frequently Asked Questions
(FAQs)
17
but a hospital is still required to display the payer-specific negotiated charge (and all other
standard charges applicable) for which the hospital has established a standard charge
regardless of whether it appears in the chargemaster. Please refer to 84 CFR 65534 for further
discussion.
Updated- If my hospital contracted for the same payer-specific standard charges
across all a payer’s plans, does my hospital need to list each individual plan in
the machine-readable file?
As a result of a better understanding of hospital and commercial payer contracting, we finalized
in the CY 2024 OPPS/ASC final rule that hospitals may indicate plan(s) as categories (such as “all
PPO plans”) for a particular payer when the established payer-specific negotiated charges are
applicable to each plan in the indicated category. We believe this exception is necessary to
ensure that hospitals are not penalized for displaying information that is consistent with their
contracting practices. Moreover, we believe that this practice could improve access to machine-
readable file data by avoiding repetition of standard charge information that would
unnecessarily increase file size. Please refer to the discussion at 88 FR 82093.
Updated- What should I do if my hospital contracts using algorithms that are
too complex and lengthy to encode in the machine-readable file?
Although we believe that a detailed algorithm provides a better understanding of the hospital’s
payer-specific negotiated charge, at this time, in the interest of reducing burden and complexity
of files, we will allow hospitals to provide a description of the algorithm that includes any
conditions that may alter the total reimbursement, rather than attempting to insert the
detailed algorithm itself in the machine-readable file. For example, if a payer-specific
negotiated charge is negotiated using a common “hybrid” algorithm, such as the MS-DRG, then
a hospital would indicate the adjusted base rate (in dollars) for an individual rather than
inserting the algorithm formula itself (88 FR 82097). Please refer to the technical instructions
available at the CMS Hospital Price Transparency - Data Dictionary GitHub repository at
https://github.com/CMSgov/hospital-price-transparency.
Updated- Should the de-identified minimum negotiated charge and the de-
identified maximum negotiated charge be based on the “Payer-specific
Negotiated Charge: Dollar Amount”, “Payer-Specific Negotiated Charge
Algorithm”, or the “Payer-specific Negotiated Charge Percentage”?
At 45 CFR § 180.20 we defined the “de-identified minimum negotiated charge” to mean the
lowest charge that a hospital has negotiated with all third-party payers for an item or service
and the ‘‘de-identified maximum negotiated charge’’ to mean the highest charge that a hospital
has negotiated with all third-party payers for an item or service. In the CMS Template(s) the

Hospital Price Transparency Frequently Asked Questions
(FAQs)
18
values for these data elements should be derived from the “Payer-specific Negotiated Charge:
Dollar Amount” data element. Please see the examples provided on the CMS Hospital Price
Transparency – Data Dictionary GitHub Repository at https://github.com/CMSgov/hospital-
price-transparency for how to encode your data in one of the three required CMS Templates.
Updated- What is an “estimated allowed amount” and when is it required in the
machine-readable file?
At 45 CFR § 180.20 we defined “estimated allowed amount” as the average dollar amount that
the hospital has historically received from a third-party payer for an item or service. Beginning
on January 1, 2025, hospitals are required to encode a dollar value for the “estimated allowed
amount” data element, when a payer-specific negotiated charge can only be expressed as an
algorithm or percentage. This includes: hybrid scenarios where the standard charge dollar is a
base rate and there is an algorithm that accounts for additional individualized charges; where
the standard charge is a percent that cannot be calculated as a dollar figure; and where the
standard charge is an algorithm (88 FR 82100). Please refer to the technical instructions
available at the CMS Hospital Price Transparency - Data Dictionary GitHub repository at
https://github.com/CMSgov/hospital-price-transparency.
Updated- How do I calculate the “estimated allowed amount”?
In the CY 2024 OPPS/ASC Final Rule we stated that we believed hospitals should retain
flexibility, in the interest of reducing burden, to determine the best data source for calculating
the estimated allowed amount. We declined at the time to be prescriptive, but indicated that
using information from the EDI 835 electronic remittance advice (ERA) transaction, the
electronic transaction that provides claim payment information, including any adjustments
made to the claim, such as denials, reductions, or increases in payment, would appear to meet
this requirement as the data in the 835 form is used by hospitals to track and analyze their
claims and reimbursement patterns (88 FR 82101). We will continue to work with hospitals and
other interested parties to better understand how hospitals are developing the estimated
allowed amount and we may provide additional guidance through future notice and comment
rulemaking.
Updated- My hospital just negotiated contracts based on the percentage of
billed charges with several new payers and does not have enough historical
claims to derive the estimated allowed amount for specific services. What
should we do?
CMS recommends that your hospital encode 999999999 (nine 9s) as the data element value to
indicate that there is not sufficient historic claims history to derive the estimated allowed
amount, and then update the file when sufficient history is available. Additionally, if your
hospital wishes to provide further context for the lack of data, your hospital can do so in the
Hospital Price Transparency Frequently Asked Questions
(FAQs)
19
appropriate additional notes field. Please refer to the technical instructions available at the
CMS Hospital Price Transparency - Data Dictionary GitHub repository at
https://github.com/CMSgov/hospital-price-transparency.
Updated- Can CMS advise me on how to encode specific standard charge
information for my hospital?
As explained in the CY2024 OPPS/ASC final rule, hospitals use different methods to establish
standard charges for items and services, resulting in charge/item and charge/service
combinations that are often unique to that hospital. Therefore, although CMS has recently
taken steps toward standardization, each hospital will continue to have some discretion related
to how it chooses to encode its standard charge information (including information related to
payer-specific negotiated charges) within its machine-readable file, so long as the file conforms
to the CMS template layouts and data specifications as described at 45 CFR § 180.50(c)(2).
Updated- I would like to propose additional valid values for the CMS machine-
readable file template, how do I do that?
You may propose additional valid values by creating a new discussion post on the CMS Hospital
Price Transparency - Data Dictionary GitHub repository at https://github.com/CMSgov/hospital-
price-transparency, or by emailing the CMS Hospital Price Transparency team at
Consumer-friendly Display of Shoppable Services
What is a shoppable service? Are medications considered shoppable services?
A shoppable service means a service that can be scheduled by a healthcare consumer in
advance. Procedures such as joint replacements and services such as physical therapy are
examples of shoppable services. Hospital administration of a medication could be considered a
shoppable service if it can be scheduled in advance. Examples of administration of a medication
that could be considered a shoppable service are the administration of flu shots or medication
infusions for chronic conditions. The definition of ‘shoppable service’ can be found at 45 CFR
§180.20.
What if a hospital does not provide one or more of the 70 CMS-specified
shoppable services or provides less than 300 shoppable services in total? How
can the requirements of this regulation be met?
If a hospital does not provide one or more of the 70 CMS-specified shoppable services, the
hospital must select additional shoppable services such that the total number of shoppable

Hospital Price Transparency Frequently Asked Questions
(FAQs)
20
services is at least 300. If a hospital does not provide 300 shoppable services, the hospital must
list as many shoppable services as they provide. The hospital must clearly indicate any CMS-
specified shoppable service that it does not provide. The hospital may use “N/A” for the
corresponding charge or use another appropriate indicator to communicate to the public that
the shoppable service is not provided by the hospital. Refer to 84 FR 65569 and 84 FR 65574 for
further discussion.
What is an ‘ancillary item and service’?
Ancillary services, defined at 45 CFR §180.20, are any item or service a hospital customarily
provides as part of, or in conjunction with, a shoppable primary service and may include
laboratory, radiology, drugs, delivery room (including maternity labor room), operating room
(including post-anesthesia and postoperative recovery rooms), therapy services (physical,
speech, occupational), hospital fees, room and board charges, and charges for employed
professional services. Ancillary services may also include other special items and services for
which charges are customarily made in addition to a routine service charge. For example, an
outpatient procedure may include many services that are provided by the hospital, for example,
local and/or global anesthesia, services of employed professionals, supplies, facility and/or
ancillary facility fees, imaging services, lab services and pre- and post-op follow up. To the
extent that a hospital customarily provides (and bills for) such ancillary services as a part of, or in
conjunction with, the primary service, the hospital should group the ancillary service charges
along with the other standard charges that are displayed for the shoppable service.
For further discussion of ancillary services refer to 84 FR 65564.
How should a hospital display charges for shoppable services in a consumer-
friendly manner when the hospital offers them as a service package or when the
hospital already includes all ancillary services as part of the service package
charge?
To the extent that a hospital includes in its public display a shoppable service that it commonly
provides as a service package, the hospital must display the charge the hospital has established
for the service package as a whole. In other words, if the hospital has established a standard
charge for a service package, the hospital must display that standard charge as opposed to
displaying a manufactured charge for each of the individual items and services that make up the
service package. For example, when displaying the charge for a shoppable service identified by a
DRG, the hospital would display the payer-specific negotiated charge (the “base rate”)
negotiated with a third-party payer for the DRG. To be consumer friendly, the hospital may
elect to communicate the individual items and services included in the standard charge for the
service package, but this is not required under the Hospital Price Transparency Final Rule.
However, should a hospital customarily provide any items or services beyond those already
included in a service package, the rule does require hospitals to list any such additional ancillary
services the hospital customarily provides with the shoppable service. In other words, the
hospital must provide a description of the ancillary service along with its standard charge(s) and

Hospital Price Transparency Frequently Asked Questions
(FAQs)
21
other required data elements, as applicable.
What does CMS consider to be a plain-language description for purposes of the
consumer-friendly display?
The regulations at 45 CFR § 180.60(b)(1) require hospitals to include a plain-language
description for each of the 70 CMS-specified and 230 hospital-selected shoppable services in its
consumer-friendly display. We invite hospitals to review the Federal plain language guidelines
that can be found here: https://plainlanguage.gov/guidelines/. Refer to 84 FR 65573.
Examples that we would consider plain-language descriptions:
• Direct Admission to the Hospital from Observation Status
• CT of the Head or Brain with Contrast
• MRI of Orbit, Face, or Neck with and without Contrast
Examples that we would not consider plain-language descriptions:
• OBSRV ASMT DIRECT ADMIT1
• CT HEAD/BRAIN W/CON 42
• MRI ORB/FACE/NK W/WO CON 43
Can a price estimator tool be used to meet the requirement to display
shoppable services in a consumer-friendly format? If yes, what requirements
must the price estimator tool meet?
Yes. In the Hospital Price Transparency Final Rule, we stated that we had been persuaded by
commenters’ suggestions that hospitals offering online price estimator tools that provide real-
time individualized out-of-pocket cost estimates should receive consideration. For further
discussion on the requirements of a price estimator tool, please see 45 CFR §180.60(a)(2).
Although we recognize that some hospital price estimator tools may not display consumer-
friendly standard charge information in the precise ways we are requiring under the rule, they
do appear to accomplish the goal and intent of ensuring such information is available in a
consumer-friendly manner by allowing individuals to directly determine their specific out-of-
pocket costs in advance of committing to a hospital service. We emphasize, however, that
hospitals must still publish their standard charges for the items and services they provide in a
comprehensive machine-readable file (45 CFR §180.50). In other words, offering a price
estimator tool can satisfy the requirement to post shoppable service information in a
consumer-friendly format but does not satisfy the requirement to display hospital standard
charges in a comprehensive machine-readable file.
Further, if a hospital chooses to exercise this option, the hospital Internet-based price estimator
tool must meet the following criteria to be deemed in compliance:
Hospital Price Transparency Frequently Asked Questions
(FAQs)
22
• Provide estimates for as many of the 70 CMS-specified shoppable services that are
provided by the hospital, and as many additional hospital-selected shoppable services
as is necessary for a combined total of at least 300 shoppable services.
• Allow healthcare consumers to, at the time they use the tool, obtain an estimate of
the amount they will be obligated to pay the hospital for the shoppable service.
• Is prominently displayed on the hospital’s website and accessible to the public
without charge and without having to register or establish a user account or
password.
Please refer to 84 FR 65577 for further discussion on this topic.
If a hospital chooses to use a price estimator tool as an alternative to meeting
the requirements for making public the standard charges for shoppable services
in a consumer-friendly manner, may hospitals collect patient insurance
information or other PII to generate a real-time out-of-pocket estimate for the
patient?
Yes. In the Hospital Price Transparency Final Rule, we specifically did not include a requirement
that no PII be collected because we recognize that insurance information may be necessary to
provide patients with real-time personalized out-of-pocket price estimates. To ensure there is
flexibility for the data elements, format, location, and accessibility of a price estimator tool that
would be considered to meet the requirements of 45 CFR §180.60, we established minimum
data and functionality requirements at 45 CFR §180.60(a)(2). Please refer to 84 FR 65577 for
further discussion on this topic.
For the price estimator tool, would a display of an estimated range across all
commercial payers for each of the 300 shoppable services meet the
requirements?
No. As clarified in the CY 2022 OPPS/ASC final rule, if a hospital chooses to offer a price
estimator tool in lieu of displaying standard charges in a consumer-friendly manner, the
hospital must ensure (among the other requirements at 45 CFR §180.60(a)(2)) that the tool
allows healthcare consumers to, at the time they use the tool, obtain an estimate of the
amount that the hospital anticipates the individual would be obligated to pay. This means that
the estimated amount is a personalized estimate of ‘‘the amount’’ the individual would be
obligated to pay and is therefore represented as a single out-of-pocket dollar amount that takes
into account the individual’s insurance status (86 FR 63954). We note, however, that Hospital
Price Transparency final rule is not prescriptive regarding the method by which a hospital’s
price estimator tool estimates the individual’s single out-of-pocket dollar amount, and nothing
in the rule prevents a hospital from developing an accurate and reliable cost estimate using
prior claims information or from providing additional information that may be useful to the

Hospital Price Transparency Frequently Asked Questions
(FAQs)
23
end-user, such as the range of out-of-pocket costs for the population to which the individual
belongs.
Does CMS have an example of disclaimer language that a hospital could use on
its price estimator tool?
No. Each hospital is unique and serves a unique patient population. We encourage, but do not
require, hospitals to provide disclaimers as applicable and appropriate in their price estimator
tools, including disclaimers acknowledging the limitation of the presented standard charge
information and advising the user to consult, as applicable, with his or her health insurer to
confirm individual payment responsibilities and remaining deductible balances.
Similarly, we encourage, but do not require, that hospital standard charge information include
the following:
• Notification of the availability of financial aid, multiple procedure discounts, payment
plans, and assistance in enrolling for Medicaid or a state program.
• An indicator for the quality of care in the healthcare setting.
• Making the standard charge information available in languages other than English, such
as Spanish and other languages that would meet the needs of the communities and
populations the hospital serves.
We discussed the flexibility to provide disclaimers in hospital price estimator tools at 84 FR
65578-65579.
Can CMS provide a list of internet-based price estimator tool vendors?
No, we do not have an available list of vendors who provide price estimator tool application
software.
Can hospitals provide additional consumer-friendly resources?
Yes. Hospitals are encouraged to embrace a patient-centered approach to care in all forms,
including providing consumer-friendly resources related to cost of care that will empower
patients with pricing information to help them make healthcare decisions that work best for
them.
Monitoring and Penalties for Noncompliance
What happens if a hospital does not comply with the Hospital Price Transparency
Final Rule?

Hospital Price Transparency Frequently Asked Questions
(FAQs)
24
CMS has the authority to monitor hospital compliance with section 2718(e) of the Public Health
Service Act, by evaluating complaints made by individuals or entities to CMS, reviewing
individuals’ or entities’ analysis of noncompliance, and auditing hospitals’ websites. Should CMS
conclude a hospital is noncompliant with one or more of the requirements to make public
standard charges, CMS may provide a warning notice to the hospital, request a corrective
action plan (CAP) from the hospital if its noncompliance constitutes a material violation of one
or more requirements, and may assess on a hospital a civil monetary penalty, and publicize the
penalty on a CMS website, should the hospital fail to respond to CMS’ request to submit, or
comply with the requirements, of a CAP. Please refer to amended 45 CFR § 180.90 for adjusted
penalty amounts under Subpart C- Monitoring and Penalties for Noncompliance.
Is CMS enforcing the Hospital Price Transparency rules?
Yes. CMS expects hospitals to comply with these legal requirements and is actively enforcing
these rules to ensure people know what a hospital charges for items and services. The public is
invited to submit a complaint to CMS if it appears that a hospital has not posted information
online.
Updated- I can’t find standard charges for a hospital where I have received or
will be receiving care. Should I file a complaint? What happens after I file a
complaint?
The hospital price transparency team is only able to address concerns related to the specific
requirements of the hospital price transparency initiative. If you are seeking a personalized
price for healthcare services you received or are scheduled to receive, we recommend you
contact the hospital. If you are looking for hospital standard charge information made public
online in a machine-readable file format but are unable to find it, you may submit a complaint
to CMS.
CMS does not respond to the original complaint. All publicly available enforcement activities
and actions can be found at https://data.cms.gov/provider-characteristics/hospitals-and-other-
facilities/hospital-price-transparency-enforcement-activities-and-outcomes, and
https://www.cms.gov/hospital-price-transparency/enforcement-actions.
What is CMS’ process for enforcing the Hospital Price Transparency rules?
The enforcement process is established in the Hospital Price Transparency regulations and
occurs in a phased manner. The process typically involves a comprehensive compliance review
in response to CMS audit or a complaint received through the Hospital Price Transparency
website. If CMS concludes a hospital is noncompliant with one or more of the requirements to
make public standard changes, CMS may take any of the following actions, which generally, but
not necessarily, will occur in the following order:

Hospital Price Transparency Frequently Asked Questions
(FAQs)
25
•
Provide a written warning notice to the hospital of the specific violation(s)
•
Request a Corrective Action Plan (CAP) if noncompliance constitutes a material violation of
one or more requirements
•
Impose a civil monetary penalty
In accordance with 45 CFR 180.80(c), if CMS issues a request for a hospital to submit a CAP, it
must be submitted by the date specified in the request and must specify the process the
hospital will take to address the deficiency(ies) identified by CMS and the timeframe by which
the hospital will complete the corrective action. A CAP is subject to CMS review and approval.
For reference, CMS has developed a CAP Response Sample as an optional format for submitting
a CAP. Should a hospital that CMS has identified as noncompliant fail to respond to CMS’
request to submit a CAP or comply with CAP requirements, CMS may impose a CMP in
accordance with 45 CFR §180.90(a). Once CMS issues a CMP, CMS will post the notice of
imposition of a CMP on a CMS website (45 CFR §180.90(e)).
How does CMS assess compliance?
During a comprehensive compliance review, CMS assesses whether the hospital’s disclosure of
standard charges meet the requirements specified at 45 CFR Part 180. Specifically, CMS
assesses whether the hospital has displayed standard charges in a machine-readable file in
accordance with the criteria established at 45 CFR §180.50 and shoppable services in a
consumer-friendly manner in accordance with the criteria established at 45 CFR §180.60.
What is CMS doing to educate hospitals and assist them with compliance?
CMS has, to date, engaged in several education and outreach activities to help prepare hospitals
for compliance:
• held several National Open Door Forums to review the requirements of the Hospital
Price Transparency final rule;
• established a dedicated hospital price transparency website at Hospital Price
Transparency | CMS with extensive FAQs, guides, webinar presentations and recordings
for hospitals;
• established a hospital price transparency tools website at Hospital Price Transparency -
Tools (cmsgov.github.io) with tools to support hospitals in meeting some of the
machine-readable file (MRF) requirements;
• established the Hospital Price Transparency- Data Dictionary GitHub repository which
houses the required CMS MRF templates, provides the data dictionary (or technical
instruction) on how hospitals must encode standard charge information into machine-
readable files starting July 1, 2024, and provides technical support; and
• established an inquiry email box ([email protected].gov) and

Hospital Price Transparency Frequently Asked Questions
(FAQs)
26
(HPTCompliance@cms.hhs.gov).
Transcripts of National Open-Door Forums can be found here: https://www.cms.gov/Outreach-
and- Education/Outreach/OpenDoorForums/PodcastAndTranscripts.
My hospital received a warning notice from CMS. How do I contact CMS with
questions about the deficiencies outlined in the notice?
An authorized official from your hospital may contact CMS via email at:
[email protected]. When contacting CMS regarding the Hospital Price
Transparency warning letter your hospital received, please submit detailed questions in writing.
CMS cannot offer anything that could be construed as legal advice. We therefore recommend
that individuals consult with hospital counsel and/or compliance officials.
Updated- Do I need to respond to a warning notice my hospital received?
Yes. As indicated in the CY 2024 OPPS/ASC Final Rule, CMS requires a hospital to submit an
acknowledgement of receipt of the warning notice in the form and manner, and by the
deadline, specified in the notice of violation issued by CMS to the hospital. Please refer to the
discussion at 88 FR 82118.
Do I need to notify CMS when my hospital has corrected any deficiencies
identified in the warning notice?
No. CMS will review the hospital website after the close of the indicated period to determine if
the deficiencies have been remedied or if further compliance actions are warranted.
Updated- My hospital is part of a larger hospital system. What happens if one of
the hospitals in our health system received a warning notice from CMS outlining
deficiencies?
As indicated in the CY 2024 OPPS/ASC Final Rule, in the event CMS takes an action to address
hospital noncompliance and the hospital is determined by CMS to be part of a health system,
CMS may notify health system leadership of the action and may work with health system
leadership to address similar deficiencies for hospitals across the health system. Please refer to
the discussion at 88 FR 82119.
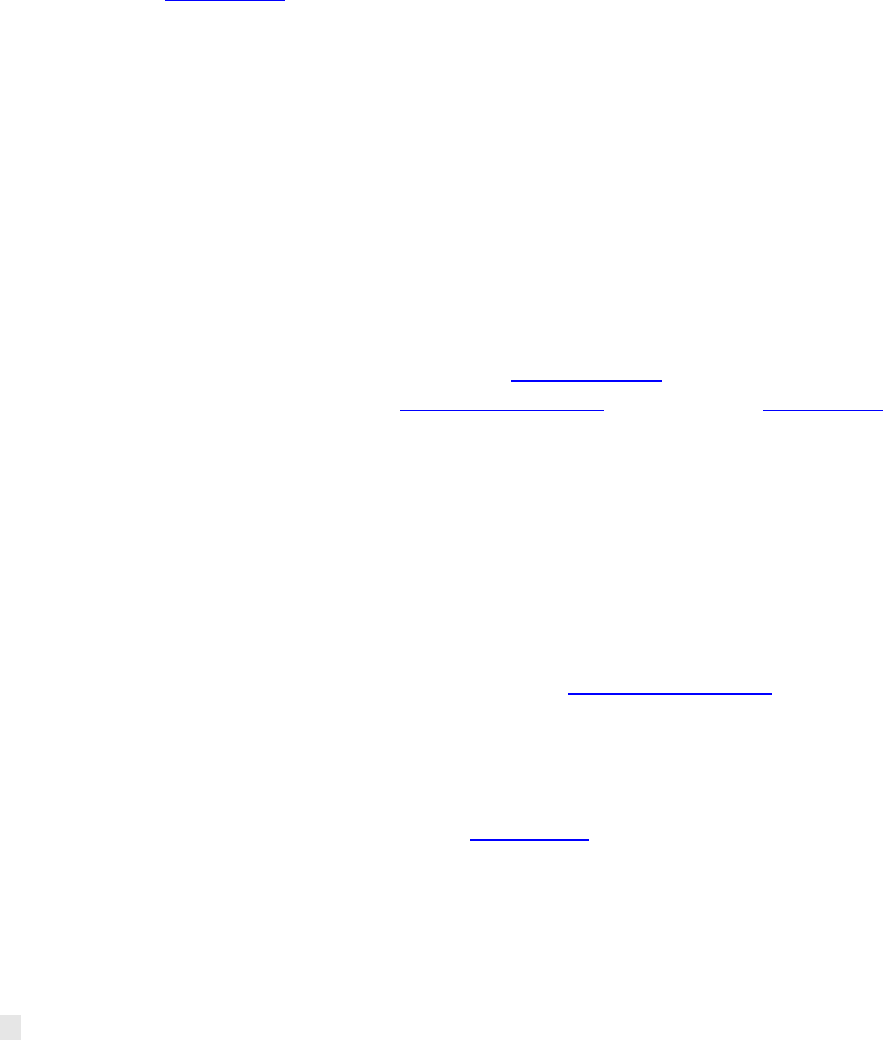
How will CMS calculate the Civil Monetary Penalty (CMP), beginning January 1,
2022, and with respect to that timeframe forward? What is the CMP
calculation?

Hospital Price Transparency Frequently Asked Questions
(FAQs)
27
The maximum daily CMP amount for hospitals with 30 or fewer beds is $300, even if the hospital
is in violation of multiple discrete requirements. The maximum daily CMP amount for hospitals
with at least 31 and up to 550 beds is the number of beds times $10. For hospitals with greater
than 550 beds, the maximum daily CMP amount is $5,500, even if the hospital is in violation of
multiple discrete requirements. Refer to 45 CFR §180.90(c)(2).
Ex. A noncompliant hospital with a bed count of 200 would be assessed a maximum daily CMP
of $2,000/day ($10*200/day) or $730,000/year.
Number of Beds
Maximum Penalty Applied Per Day
Total Maximum Penalty Amount
for full Calendar Year of
Noncompliance
30 or fewer
$300 per hospital
$109,500 per hospital
31 up to 550
$310 - $5,500 per hospital (number of
beds times $10)
$113,150 - $2,007,500 per hospital
>550
$5,500 per hospital
$2,007,500 per hospital
Note: In subsequent years, amounts will be adjusted according to 45 CFR 180.90(c)(3).
Why is a scaling factor being used?
A scaling factor is being used to address a trend towards a high rate of hospital noncompliance
identified by CMS through sampling and reviews to date, and the reported initial high rate of
hospital noncompliance with 45 CFR part 180. Several factors informed our decision to use a
scaling factor to determine the CMP, including: the ability to penalize based on a sliding scale
method that relates to the hospital’s characteristics, such as using the hospital’s number of
beds as a proxy for the size of the patient population; the use of scaling factors in other Federal
programs to determine CMP amounts; and the availability of a reliable source of data that can
be used to establish a CMP amount across most hospitals. We believe a scaling factor approach
strikes an appropriate balance and provides for the assessment of a CMP that is commensurate
with the level of severity of the potential violation. Please refer to the discussion at 86 FR
63948.
What is the source of data used to determine bed count for scaling the CMP and
where is that information located?
The scaling factor for the CMP amount uses hospital cost report data. This data is routinely
submitted by Medicare-enrolled hospitals, is certified by a hospital official, and is reviewed by a
Medicare Administrative Contractor (MAC) to determine acceptability and is submitted
annually. The cost report contains provider information such as facility characteristics and
financial statement data. CMS maintains the cost report data in the Healthcare Provider Cost
Reporting Information System (HCRIS). Further, the chief financial officer or administrator of
Hospital Price Transparency Frequently Asked Questions
(FAQs)
28
the provider certifies the content of the submitted cost report is true, correct, complete and
prepared from the books and records of the provider in accordance with applicable
instructions.
1
The website is available here: https://www.cms.gov/Research-Statistics-Data-and-
Systems/Downloadable-Public-Use-Files/Cost- Reports. Please refer to the discussion at 86 FR
63944.
How will CMS determine the bed count for a hospital that is not a Medicare-
enrolled hospital?
If the bed count information cannot be determined using Medicare hospital cost report data,
CMS will specify the conditions for CMS’ receipt of documentation from the hospital to
determine its number of beds, and if the hospital does not provide CMS with such
documentation (in the prescribed form and manner, and by the specified deadline), CMS will
impose a CMP on the hospital at the highest, maximum daily dollar amount ($5,500 per day).
Please refer to 45 CFR § 180.90(c)(2)(ii)(D)(2).
Is there a public list of non-compliant hospitals that have been assessed a civil
monetary penalty (CMP)?
The public list of non-compliant hospitals that have been assessed a CMP is located on the CMS
Price Transparency website: https://www.cms.gov/hospital-price-transparency/enforcement-
actions.
Appeals of Civil Monetary Penalties
Can a hospital appeal a civil monetary penalty related to hospital price
transparency?
Yes. A hospital upon which CMS has imposed a penalty may request a hearing before an
Administrative Law Judge (ALJ) in accordance with 45 CFR part 180, subpart D. In deciding
whether the amount of a civil monetary penalty is reasonable, the ALJ may only consider
evidence of record related to the following: hospital’s posting(s) of standard charges, if
available; material the hospital timely previously submitted to CMS (including with respect to
corrective actions and corrective action plans), and material CMS used to monitor and assess
the hospital’s compliance.
1
42 CFR 413.24(f)(4)(iv). See also, Form CMS-2552-10. Available at: https://www.cms.gov/Regulations-and-
Guidance/Guidance/Manuals/Paper-Based-Manuals-Items/CMS021935, Chapter 40-(T16)-- Hospital & Hospital
Health Care (Form CMS-2552-10) (ZIP), file “R16P240f.pdf”, Part II – Certification.

Hospital Price Transparency Frequently Asked Questions
(FAQs)
29
How long does a hospital have to request a hearing?
A hospital must request a hearing within 30 calendar days after the date of issuance of the
notice of imposition of a civil monetary penalty. The “date of issuance” is no more than five (5)
days after the filing date postmarked by the U.S. Postal Service, or deposited with a carrier for
commercial delivery, unless there is a showing that the document was received earlier. Please
refer to 45 CFR §150.401 and 45 CFR §150.405(a).
Can a hospital request an extension of time for filing a request for a hearing?
A request for an extension of time must be made promptly by written motion. The ALJ may
extend the time for filing a request for hearing only if the ALJ finds that the hospital was
prevented by events or circumstances beyond its control from filing its request within 30
calendar days after the date of issuance of the notice of imposition of a civil monetary penalty.
Please refer to 45 CFR §150.405(b).
What happens if a hospital does not request a hearing within the required
timeframe?
If a hospital does not request a hearing within 30 calendar days of the issuance of the notice of
imposition of a CMP, CMS may impose the CMP indicated in such notice and may impose
additional penalties pursuant to continuing violations according to 45 CFR §180.90(f) without
right of appeal. 45 CFR §180.110(b) provides that the hospital has no right to appeal a penalty
for which it has not requested a hearing in accordance with 45 CFR §150.405, unless the
hospital can show good cause, as determined at 45 CFR §150.405(b), for failing to timely
exercise its right to a hearing.
