______________________________________________________________________________
Page 1 of 38
PRODUCT MONOGRAPH
Pr
Alembic-Lacosamide
(Lacosamide Tablets)
50 mg, 100 mg, 150 mg and 200 mg film-coated tablets
Antiepileptic Agent
Manufactured by:
Alembic Pharmaceuticals Limited
Alembic Road,
Vadodara – 390003,
Gujarat, India
Canadian Importer and Distributor:
Alembic Pharmaceuticals Canada Ltd.
2680, Matheson Blvd. East, Unit 102
Mississauga, Ontario
L4W 0A5, Canada
Submission Control No: 222570 Date of Preparation: December 19, 2018
______________________________________________________________________________
Page 2 of 38
Table of Contents
PART I: HEALTH PROFESSIONAL INFORMATION.......................................................3
SUMMARY PRODUCT INFORMATION.....................................................................3
INDICATIONS AND CLINICAL USE...........................................................................3
CONTRAINDICATIONS................................................................................................4
WARNINGS AND PRECAUTIONS..............................................................................4
ADVERSE REACTIONS................................................................................................9
DRUG INTERACTIONS................................................................................................17
DOSAGE AND ADMINISTRATION............................................................................19
OVERDOSAGE...............................................................................................................21
ACTION AND CLINICAL PHARMACOLOGY...........................................................22
STORAGE AND STABILITY........................................................................................25
DOSAGE FORMS, COMPOSITION AND PACKAGING...........................................26
PART II: SCIENTIFIC INFORMATION...............................................................................27
PHARMACEUTICAL INFORMATION........................................................................27
CLINICAL TRIALS........................................................................................................27
DETAILED PHARMACOLOGY...................................................................................31
TOXICOLOGY...............................................................................................................32
REFERENCES................................................................................................................34
PART III: CONSUMER INFORMATION............................................................................35

______________________________________________________________________________
Page 3 of 38
Pr
Alembic-Lacosamide
(Lacosamide Tablets)
PART I: HEALTH PROFESSIONAL INFORMATION
SUMMARY PRODUCT INFORMATION
Route of
Administration
Dosage Form /
Strength
Nonmedicinal Ingredients
Oral Film-coated tablets /
50 mg, 100 mg, 150
mg and 200 mg
microcrystalline cellulose, crospovidone,
hydroxypropyl cellulose, low-substituted
hydroxypropyl cellulose, colloidal silicon dioxide,
magnesium stearate, hypromellose, polyethylene
glycol, talc, titanium dioxide, and dye pigments:
50 mg tablets: FD&C Blue #2 aluminum lake, iron
oxide red, iron oxide black
100 mg tablets: iron oxide yellow
150 mg tablets: iron oxide yellow, iron oxide red,
iron oxide black
200 mg tablets: FD&C Blue #2 aluminum lake
INDICATIONS AND CLINICAL USE
Adults (≥18 years of age)
Alembic-Lacosamide is indicated as:
Monotherapy in the management of partial-onset seizures in adult patients with epilepsy.
All patients who participated in the monotherapy trial were newly or recently diagnosed
with epilepsy (see CLINICAL TRIALS).
Adjunctive therapy in the management of partial-onset seizures in adult patients with
epilepsy who are not satisfactorily controlled with conventional therapy.
Geriatrics (≥ 65 years of age)
The clinical experience with lacosamide tablets in elderly patients with epilepsy is limited.
Caution should be exercised during dose titration and age-associated decreased renal clearance
should be considered in elderly patients (see WARNINGS AND PRECAUTIONS, Special
Populations, Geriatrics, DOSAGE AND ADMINISTRATION and ACTION AND
CLINICAL PHARMACOLOGY, Special Populations and Conditions, Geriatrics).
Pediatrics (<18 years of age)

______________________________________________________________________________
Page 4 of 38
The safety and efficacy of lacosamide tablets in pediatric patients (<18 years of age) have not
been established and its use in this patient population is not indicated (see WARNINGS AND
PRECAUTIONS, Special Populations, Pediatrics).
CONTRAINDICATIONS
Patients who are hypersensitive to the active substance or to any of the excipients. For a
complete listing, see the DOSAGE FORMS, COMPOSITION AND PACKAGING
section of the product monograph.
Patients with a history of, or presence of, second- or third-degree atrioventricular (AV)
block.
WARNINGS AND PRECAUTIONS
General
Withdrawal of Antiepileptic Drugs (AEDs)
As with all AEDs, lacosamide should be withdrawn gradually (over a minimum of 1 week) to
minimize the potential of increased seizure frequency (see DOSAGE AND
ADMINISTRATION, Recommended Dose and Dosage Adjustment).
Cardiac Rhythm and Conduction Abnormalities
PR Interval Prolongation
In post-marketing experience, AV block (including second degree or higher AV block) has been
reported. In patients with proarrhythmic conditions, ventricular tachyarrhythmia has been rarely
reported. In rare cases, these events have led to asystole, cardiac arrest and death in patients with
underlying proarrhythmic conditions.
Patients should be made aware of the symptoms of cardiac arrhythmia (e.g. slow, rapid or
irregular pulse, palpitations, shortness of breath, feeling of lightheaded, fainting), and told to
seek immediate medical advice if these symptoms occur.
In patients who develop serious cardiac arrhythmia, lacosamide should be discontinued and a
thorough clinical benefit/risk assessment should be performed before possibly restarting therapy.
Lacosamide should be used with caution in patients with underlying proarrhythmic conditions
such as patients with known cardiac conduction problems [e.g. marked first-degree
atrioventricular (AV) block, sick sinus syndrome without pacemaker], or severe cardiac disease
(e.g. myocardial ischemia/ infraction, heart failure, structural heart disease, or cardiac sodium
channelopathies) or patients treated with medicinal products affecting cardiac conduction (see
DRUG INTERACTIONS). In such patients, obtaining an ECG before beginning lacosamide,
and after lacosamide is titrated to steady-state, is recommended.
Caution should especially be exerted when treating elderly patients as they may be at increased
risk of cardiac disorder or when lacosamide is given with other drugs that prolong the PR
interval (e.g. sodium channel blocking antiepileptic drugs, pregabalin, or beta-blockers), as

______________________________________________________________________________
Page 5 of 38
further PR prolongation is possible (see ADVERSE REACTIONS, Cardiac and DRUG
INTERACTIONS). In these patients it should be considered to perform an ECG before a
lacosamide dose increase above 400mg/day and after lacosamide is titrated to steady-state.
In clinical trials of healthy subjects and patients with epilepsy, lacosamide treatment was
associated with PR interval prolongation in a dose-dependent manner (see ACTION AND
CLINICAL PHARMACOLOGY, Pharmacodynamics). Patients with significant
electrocardiographic (ECG) abnormalities were systematically excluded from these trials. The
mean PR interval increase (at t
max
) in a clinical pharmacology ECG trial of healthy subjects was
13.6ms for the 400mg/day lacosamide group, 18.2ms for the 800mg/day lacosamide group, and
6.3ms for the placebo group. The mean increase in PR interval at the end of 12 weeks
maintenance treatment for patients with partial-onset seizures who participated in the controlled
adjunctive therapy trials was 1.4ms, 4.4ms, and 6.6ms for the lacosamide 200, 400, and
600mg/day groups, respectively, and -0.3ms for the placebo group. The mean maximum increase
in PR interval in these controlled trials was 12.7ms, 14.3ms, and 15.7ms in the lacosamide 200,
400, and 600mg/day groups and 11.2ms in the placebo group. Among patients who participated
in these controlled trials, asymptomatic first-degree atrioventricular (AV) block was detected on
ECG and reported as an adverse reaction for 0.4% (4/944 patients) in the lacosamide group and
0% (0/364 patients) in the placebo group (see ADVERSE REACTIONS).
Atrial Fibrillation and Atrial Flutter
Lacosamide administration may predispose to atrial arrhythmias (atrial fibrillation or flutter),
especially in patients with diabetic neuropathy and/or cardiovascular disease. Patients should be
made aware of the symptoms of atrial fibrillation and flutter (e.g. palpitations, rapid or irregular
pulse, shortness of breath) and told to contact their physician should any of these symptoms
occur.
Atrial fibrillation and flutter have been reported in open-label epilepsy trials and in post-
marketing experience. No cases occurred in the short-term investigational trials of lacosamide in
epilepsy patients. In patients with diabetic neuropathy, 0.6% of patients treated with lacosamide
experienced an adverse reaction of atrial fibrillation or atrial flutter, compared to 0% of placebo-
treated patients.
Syncope
In the short-term controlled adjunctive therapy trials of lacosamide in epilepsy patients with no
significant system illnesses, there was no increase in syncope compared to placebo. In the short-
term controlled trials of lacosamide in patients with diabetic neuropathy, 1.0% of patients who
were treated with lacosamide reported an adverse reaction of syncope or loss of consciousness,
compared to 0% of placebo-treated patients with diabetic neuropathy. Most of the cases of
syncope were observed in patients receiving doses above 400 mg/day. The cause of syncope was
not determined in most cases. However, several were associated with either changes in
orthostatic blood pressure, atrial flutter/fibrillation (and associated tachycardia), or bradycardia.
In the controlled monotherapy trial, seven patients (1.6%) reported syncope in the lacosamide-
treated group during the treatment period (see ADVERSE REACTIONS, Intravenous Adverse
Reactions).

______________________________________________________________________________
Page 6 of 38
Carcinogenesis and Mutagenesis
See Product Monograph Part II: TOXICOLOGY, Carcinogenicity and Mutagenicity for
discussion on animal data.
Hepatic/Biliary/Pancreatic
Rare post-marketing reports of severe liver injury, including acute liver failure, have been
reported in patients treated with lacosamide. Some of the cases were considered clinically
significant and possibly or probably related to lacosamide therapy. Laboratory testing to
determine liver enzyme levels should be done upon the first symptom or sign of liver
dysfunction (e.g., pruritus, dark urine, jaundice, right upper quadrant tenderness, or unexplained
"flu-like" symptoms). Lacosamide Tablets should be discontinued in patients with jaundice or
laboratory evidence of liver injury and alternative therapy should be considered (see Post-
Market Adverse Drug Reactions, Hepatic/Biliary/Pancreatic).
Hypersensitivity
Multiorgan hypersensitivity reactions (including Drug Reaction with Eosinophilia and Systemic
Symptoms, or DRESS), Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis
(TEN) have been reported with anticonvulsants, including lacosamide.
Typically, although not exclusively, DRESS presents with fever and rash associated with other
organ system involvement, that may or may not include eosinophilia, hepatitis, nephritis,
lymphadenopathy, and/or myocarditis. Because these disorders are variable in their expression,
other organ system signs and symptoms not noted here may also occur. If any of these
hypersensitivity reactions are suspected, lacosamide should be discontinued and alternative
treatment started.
One case of symptomatic hepatitis and nephritis was observed among 4011 subjects exposed to
lacosamide during clinical development. The event occurred in a healthy volunteer, 10 days after
stopping lacosamide treatment. The subject was not taking any concomitant medication and
potential known viral etiologies for hepatitis were ruled out. The subject fully recovered within a
month, without specific treatment. The case is consistent with a delayed multiorgan
hypersensitivity reaction. Additional potential cases included 2 with rash and elevated liver
enzymes and 1 with myocarditis and hepatitis of uncertain etiology.
SJS has been reported very rarely in post-marketing experience during treatment with lacosamide
in combination with other antiepileptic drugs. A causal relationship between SJS and lacosamide
treatment cannot be excluded. SJS was not reported during clinical development.
No cases of TEN were reported during clinical development. TEN has been reported very rarely
in post-marketing experience during treatment with lacosamide in combination with other drugs
including antiepileptic drugs. A causal relationship between TEN and lacosamide treatment
cannot be excluded.
Neurologic
Dizziness and Ataxia
Treatment with lacosamide has been associated with dizziness and ataxia which could increase
the occurrence of accidental injury or falls.

______________________________________________________________________________
Page 7 of 38
In controlled adjunctive therapy clinical trials, dizziness was experienced by 25% of patients
with partial-onset seizures taking 1 to 3 concomitant AEDs randomized to the recommended
doses (200 to 400 mg/day) of lacosamide (compared with 8% of placebo patients) and was the
adverse event most frequently leading to discontinuation (3%). Ataxia was experienced by 6% of
patients randomized to the recommended doses (200 to 400 mg/day) of lacosamide (compared to
2% of placebo patients) (see ADVERSE REACTIONS, Clinical Trial Adverse Drug
Reactions). There was a substantial increase in the frequency of occurrence of these events when
patients received lacosamide doses greater than 400 mg/day.
Accordingly, patients should be advised not to drive a car or to operate other complex machinery
or perform hazardous tasks until they are familiar with the effects of Alembic-Lacosamide on
their ability to perform such activities (see Part III: CONSUMER INFORMATION).
Ophthalmological Effects
In controlled adjunctive therapy trials in patients with partial-onset seizures, lacosamide
treatment was associated with vision-related adverse events such as blurred vision (lacosamide,
8%; placebo, 3%) and diplopia (lacosamide, 11%; placebo, 2%). Three percent of patients
randomized to lacosamide discontinued treatment due to vision-related adverse events (primarily
diplopia) (see ADVERSE REACTIONS).
Patients should be informed that if visual disturbances occur, they should notify their physician
promptly. If visual disturbance persists, further assessment, including dose reduction and
possible discontinuation of lacosamide, should be considered. More frequent assessments should
be considered for patients with known vision-related issues or those who are already routinely
monitored for ocular conditions.
Psychiatric
Suicidal Ideation and Behaviour
Suicidal ideation and behaviour have been reported in patients treated with antiepileptic agents in
several indications.
All patients treated with antiepileptic drugs, irrespective of indication, should be monitored for
signs of suicidal ideation and behaviour and appropriate treatment should be considered. Patients
(and caregivers of patients) should be advised to seek medical advice should signs of suicidal
ideation or behaviour emerge.
An FDA meta-analysis of randomized placebo controlled trials, in which antiepileptic drugs
were used for various indications, has shown a small increased risk of suicidal ideation and
behaviour in patients treated with these drugs. The mechanism of this risk is not known.
There were 43892 patients treated in the placebo controlled clinical trials that were included in
the meta-analysis. Approximately 75% of patients in these clinical trials were treated for
indications other than epilepsy and, for the majority of non-epilepsy indications the treatment
(antiepileptic drug or placebo) was administered as monotherapy. Patients with epilepsy
represented approximately 25% of the total number of patients treated in the placebo controlled
clinical trials and, for the majority of epilepsy patients, treatment (antiepileptic drug or placebo)

______________________________________________________________________________
Page 8 of 38
was administered as adjunct to other antiepileptic agents (i.e., patients in both treatment arms
were being treated with one or more antiepileptic drug). Therefore, the small increased risk of
suicidal ideation and behaviour reported from the meta-analysis (0.43% for patients on
antiepileptic drugs compared to 0.24% for patients on placebo) is based largely on patients that
received monotherapy treatment (antiepileptic drug or placebo) for non-epilepsy indications. The
study design does not allow an estimation of the risk of suicidal ideation and behaviour for
patients with epilepsy that are taking antiepileptic drugs, due both to this population being the
minority in the study, and the drug-placebo comparison in this population being confounded by
the presence of adjunct antiepileptic drug treatment in both arms.
Special Populations
Women of Childbearing Potential / Contraception: There was no clinically relevant
interaction between lacosamide and oral contraceptives (ethinylestradiol and levonorgestrel) in
clinical studies (see DRUG INTERACTIONS, Drug-Drug Interactions, Oral
Contraceptives).
Pregnant Women: There are no studies with lacosamide in pregnant women. Studies in animals
did not indicate any teratogenic effects in rats or rabbits, but embryotoxicity was observed in rats
and rabbits at maternal toxic doses (see TOXICOLOGY, Reproduction Studies).
Since the potential risk for humans is unknown, lacosamide should not be used during pregnancy
unless the benefit to the mother clearly outweighs the potential risk to the foetus. If women
decide to become pregnant while taking lacosamide, the use of this product should be carefully
re-evaluated.
Pregnancy Registry: Physicians are advised to recommend that pregnant patients taking
Alembic-Lacosamide enroll in the North American Antiepileptic Drug Pregnancy Registry. This
can be done by calling the toll free number 1-888-233-2334, and must be done by patients
themselves. Information on the registry can also be found at the following website:
http://www.aedpregnancyregistry.org/
Nursing Women: It is unknown whether lacosamide is excreted in human breast milk. Animal
studies have shown excretion of lacosamide in breast milk. Because many drugs are excreted
into human milk, a decision should be made whether to discontinue nursing or to discontinue
lacosamide, taking into account the importance of the drug to the mother.
Fertility: No adverse effects on male or female fertility or reproduction were observed in rats at
doses producing plasma exposures (AUC) up to approximately 2 times the plasma AUC in
humans at the maximum recommended human dose (MRHD) of 400 mg/day.
Geriatrics (≥ 65 years of age): The experience with lacosamide in elderly patients with epilepsy
is limited. Although no dose reduction is necessary in elderly patients, caution should be
exercised during dose titration and age-associated decreased renal clearance with an increase in
AUC levels should be considered in elderly patients (see DOSAGE AND ADMINISTRATION

______________________________________________________________________________
Page 9 of 38
and ACTION AND CLINICAL PHARMACOLOGY, Special Populations and Conditions,
Geriatrics).
Pediatrics (< 18 years of age): Alembic-Lacosamide is not indicated for use in pediatrics (< 18
years of age) as there is insufficient data on safety and efficacy of the drug in this population (see
INDICATIONS and DOSAGE AND ADMINISTRATION).
Monitoring and Laboratory Tests
See WARNINGS AND PRECAUTIONS, Cardiac Rhythm and Conduction Abnormalities.
ADVERSE REACTIONS
Adverse Drug Reaction Overview
In controlled adjunctive therapy clinical trials in patients with partial-onset seizures, 924 patients
received lacosamide tablets. In the controlled monotherapy clinical trial in patients with partial-
onset seizures, 444 patients received at least one dose of lacosamide tablets.
Some of the most frequently reported adverse reactions in controlled clinical trials with
lacosamide treatment were dizziness, headache, nausea, and vision-related events (e.g. diplopia,
blurred vision). They were dose-related and usually mild to moderate in intensity.
The adverse event profile for the monotherapy clinical trial was similar to that of the adjunctive
therapy trials with some exceptions (see below).
Clinical Trial Adverse Drug Reactions
Because clinical trials are conducted under very specific conditions, the adverse reaction rates
observed in the clinical trials may not reflect the rates observed in practice and should not be
compared to the rates in the clinical trials of another drug. Adverse drug reaction information
from clinical trials is useful for identifying drug-related adverse events and for approximating
rates.
Adjunctive Therapy and Monotherapy
Table 1 gives the incidence of treatment-emergent adverse events that occurred in ≥1% of adult
patients with partial-onset seizures in the total lacosamide group (n=944) and for which the
frequency was greater than placebo, in controlled adjunctive therapy clinical trials. The majority
of adverse events were reported with a maximum intensity of ‘mild’ or ‘moderate’.
Table 1: Treatment-Emergent Adverse Event Incidence in Double-Blind, Placebo-
Controlled Adjunctive Therapy Partial-Onset Seizure Trials (Events ≥1% of Patients in the
total Lacosamide group and More Frequent Than in the Placebo Group).
MedDRA
System Organ Class/
Preferred
Term
Placebo
N=364
%
200 mg/day
N=270
%
400 mg/day
N=471
%
600 mg/day
N=203
%

______________________________________________________________________________
Page 10 of 38
MedDRA
System Organ Class/
Preferred
Term
Placebo
N=364
%
200 mg/day
N=270
%
400 mg/day
N=471
%
600 mg/day
N=203
%
Ear and labyrinth disorders
Vertigo
1
5
3
4
Tinnitus
1
0
2
2
Eye disorders
Diplopia
2
6
10 16
Vision blurred
3
2
9
16
Conjunctivitis <1
2
<1
0
Gastrointestinal disorders
Nausea
4
7
11 17
Vomiting
3
6
9
16
Diarrhoea
3
3
5
4
Constipation
1
1
2
4
Flatulence
0
3
2
1
Dyspepsia
1
1
2
2
Toothache
1
2
2
1
Dry Mouth
1
1
1
2
Hypoaesthesia oral
0
0
1
1
General disorders and administration site conditions
Fatigue
6
7
7
15
Gait disturbance <1 <1
2
4
Asthenia
1
2
2
4
Irritability
1
1
2
2
Chest pain
1
2
1
2
Pyrexia
1
2
1
1
Feeling drunk
0
0
1
3
Oedema peripheral
0
1
<1
2
Feeling abnormal <1
0
1
2
Infections and infestations
Nasopharyngitis
6
6
8
4
Bronchitis
0
2
1
1
Rhinitis <1 <1
1
1
Ear infection <1
1
1
0
Cystitis <1
1
<1
1

______________________________________________________________________________
Page 11 of 38
MedDRA
System Organ Class/
Preferred
Term
Placebo
N=364
%
200 mg/day
N=270
%
400 mg/day
N=471
%
600 mg/day
N=203
%
Gastroenteritis
0
1
<1
0
Injury, poisoning and procedural complications
Contusion
3
3
4
2
Skin laceration
2
2
3
3
Fall <1
1
2
1
Head injury <1
2
1
1
Joint sprain
0
1
1
2
Investigations
Positive rombergism
0
1
1
2
Gamma-
glutamyltransferase
increased
<1
2
<1
1
White blood cell count
decreased
<1
0
<1
2
Metabolism and nutrition disorders
Decreased appetite <1 <1
2
3
Hypercholesterolaemia <1
1
1
1
Musculoskeletal and connective tissue disorders
Muscle spasms <1
1
1
2
Neck pain <1
1
1
1
Nervous system disorders
Dizziness
8
16 30 53
Headache
9
11 14 12
Ataxia
2
4
7
15
Somnolence
5
5
8
8
Tremor
4
4
6
12
Nystagmus
4
2
5
10
Balance disorder
0
1
5
6
Memory Impairment
2
1
2
6
Cognitive disorder <1 <1
2
2
Hypoaesthesia
1
2
2
2
Dysarthria <1 <1
1
3
Disturbance in
attention
1
0
1
2

______________________________________________________________________________
Page 12 of 38
MedDRA
System Organ Class/
Preferred
Term
Placebo
N=364
%
200 mg/day
N=270
%
400 mg/day
N=471
%
600 mg/day
N=203
%
Psychiatric disorders
Depression
1
2
2
2
Insomnia
1
2
2
1
Confusional state
1
0
2
3
Mood altered <1
1
1
2
Respiratory, thoracic and mediastinal disorders
Dyspnoea <1
0
1
1
Epistaxis
0
1
1
0
Skin and subcutaneous tissue disorders
Pruritus
1
3
2
3
Hyperhidrosis <1
0
1
2
Table 2: Incidence of Most Common Dose-Related Treatment-Emergent Adverse Events in
Double-Blind, Placebo-Controlled Adjunctive Therapy Partial-Onset Seizure Trials
(Events ≥1% of Patients in the total Lacosamide group and More Frequent Than in the
Placebo Group).
MedDRA
Preferred
Term
Placebo
N=364
%
200 mg/day
N=270
%
400 mg/day
N=471
%
600 mg/day
N=203
%
Diplopia
2
6
10 16
Vision blurred
3
2
9
16
Nausea
4
7
11 17
Vomiting
3
6
9
16
Dizziness
8
16 30 53
Ataxia
2
4
7
15
Tremor
4
4
6
12
Nystagmus
4
2
5
10
Cardiac
Dose-dependent prolongations in PR interval with lacosamide have been observed in clinical
studies in patients and in healthy subjects (see ACTION AND CLINICAL
PHARMACOLOGY). In controlled adjunctive therapy clinical trials in patients with partial-
onset seizures, asymptomatic first-degree AV block was observed as an adverse reaction in 0.4%
(4/944) of patients randomized to receive lacosamide and 0% (0/364) of patients randomized to
receive placebo. In the controlled monotherapy clinical trial in patients with partial-onset
______________________________________________________________________________
Page 13 of 38
seizures, first-degree AV block was reported in 1.6% (6/382) of lacosamide-treated patients aged
less than 65 years of age and in 4.8% (3/62) of lacosamide-treated patients older than 65 years of
age. In clinical trials in patients with diabetic neuropathy, asymptomatic first-degree AV block
was observed as an adverse reaction in 0.6% (8/1393) of patients receiving lacosamide and 0%
(0/470) of patients receiving placebo. No second or higher degree AV block was seen in
lacosamide treated epilepsy patients in controlled clinical trials. In clinical trials in patients with
diabetic neuropathic pain, second-degree AV block has been rarely reported (<0.1%) (see
WARNINGS AND PRECAUTIONS). However, cases with second and third degree AV block
associated with lacosamide treatment have been reported in post-marketing experience (see Post-
Market Adverse Drug Reactions).
Syncope
In the monotherapy clinical trial comparing lacosamide to carbamazepine (controlled release),
syncope was reported in 7/444 (1.6%) lacosamide treated patients and 1/442 (0.2%)
carbamazepine (controlled-release) treated patients (see WARNINGS AND PRECAUTIONS,
Syncope).
Elderly
In the monotherapy study comparing lacosamide to carbamazepine (controlled release), the
safety profile of lacosamide in elderly patients (≥ 65 years of age) appeared to be similar to that
observed in patients less than 65 years of age. However, a higher incidence of fall (9.7% vs.
0.8%), diarrhea (6.5% vs. 1.3%) and tremor (6.5% vs. 0.3%) was reported in elderly patients
compared to younger adult patients.
Less Common Clinical Trial Adverse Drug Reactions (<1%):
Other adverse events reported by <1% of patients with partial-onset seizures in the total
lacosamide group in placebo-controlled adjunctive therapy clinical trials that occurred more
frequently than in the placebo group were:
Eye disorders: eye irritation
Nervous system disorders: hypokinesia
Vascular disorders: hot flush
Other Adverse Reactions in Patients with Partial-Onset Seizures
The following is a list of treatment-emergent adverse events reported by patients treated with
lacosamide in all clinical trials in patients with partial-onset seizures, including controlled trials
and long-term open-label extension trials. Events addressed in other tables or sections are not
listed here.
Events included in this list from the controlled trials occurred more frequently on drug than on
placebo and/or were based on consideration of lacosamide pharmacology, frequency above that
expected in the population, seriousness, and likelihood of a relationship to lacosamide. Events
are further classified within system organ class.
Blood and lymphatic system disorders: neutropenia, anemia
Cardiac disorders: palpitations
Investigations: alanine aminotransferase increased
______________________________________________________________________________
Page 14 of 38
Nervous system disorders: paresthesia, cerebellar syndrome
Discontinuation Due to Adverse Events in Pre-marketing Controlled Clinical Studies
In controlled adjunctive therapy clinical trials in patients with partial-onset seizures, the rate of
discontinuation as a result of an adverse event was 8% and 17% in patients randomized to
receive lacosamide at doses of 200 and 400 mg/day, respectively (placebo: 5%). At lacosamide
doses of 600 mg/day, 29% of the patients discontinued the trials due to adverse events. The
adverse events most commonly (≥1% in the lacosamide total group and greater than placebo)
leading to discontinuation were dizziness, coordination abnormal, vomiting, diplopia, nausea,
vertigo, and vision blurred. Other adverse events that led to discontinuation (<1% in the
lacosamide total group and greater than placebo) were typically CNS related and included
tremor, nystagmus, fatigue, balance disorder, and disturbance in attention.
In the controlled monotherapy clinical trial in patients with partial-onset seizures, the rate of
discontinuation as a result of an adverse event was 10.6% for patients treated with lacosamide
and 15.6% for patients treated with active comparator [carbamazepine (controlled-release)]. The
adverse event most commonly (≥1% in the lacosamide treatment group) leading to
discontinuation was dizziness (1.4%).
Comparison of Gender and Race: The overall adverse event rate was similar in male and
female patients. Although there were few non-Caucasian patients, no differences in the
incidences of adverse events compared to Caucasian patients were observed.
Abnormal Hematologic and Clinical Chemistry Findings:
Abnormalities in liver function tests have been observed in controlled trials with lacosamide in
adult patients with partial-onset seizures who were taking 1 to 3 concomitant anti-epileptic drugs.
Elevations of ALT to ≥3x ULN (upper limit of normal) occurred in 0.7% (7/935) of lacosamide
patients and 0% (0/356) of placebo patients. One case of hepatitis with transaminases >20x ULN
was observed in one healthy subject 10 days after lacosamide treatment completion, along with
nephritis (proteinuria and urine casts). Serologic studies were negative for viral hepatitis.
Transaminases returned to normal within one month without specific treatment. At the time of
this event, bilirubin was normal. The hepatitis/nephritis was interpreted as a delayed
hypersensitivity reaction to lacosamide.
Drug Abuse and Dependence/Liability
Lacosamide showed no signs of abuse potential in three rat models. After prolonged
administration to rats and dogs, there was no tolerance to lacosamide’s pharmacological actions
and abrupt cessation of treatment did not produce symptoms of psychological or physical
dependence.
In a human abuse potential study, single doses of 200 mg and 800 mg lacosamide produced
euphoria-type subjective responses that differentiated statistically from placebo; at 800 mg, these
euphoria-type responses were statistically indistinguishable from those produced by alprazolam.
The duration of the euphoria-type responses following lacosamide was less than that following
alprazolam. A high rate of euphoria was also reported as an adverse event in the human abuse
potential study following single doses of 800 mg lacosamide (15% [5/34]) compared to placebo

______________________________________________________________________________
Page 15 of 38
(0%) and in two pharmacokinetic studies following single and multiple doses of 300-800 mg
lacosamide (ranging from 6% [2/33] to 25% [3/12]) compared to placebo (0%). However, the
rate of euphoria reported as an adverse event in the lacosamide development program at
therapeutic doses was less than 1%.
Abrupt termination of lacosamide in clinical trials with diabetic neuropathic pain patients
produced no signs or symptoms that are associated with a withdrawal syndrome indicative of
physical dependence. However, psychological dependence cannot be excluded due to the ability
of lacosamide to produce euphoria-type adverse events in humans.
Post-Market Adverse Drug Reactions
Since the first global approval of lacosamide on 29 August 2008 through 28 February 2018, there
are approximately 1, 424,796 patient-years of exposure to lacosamide. In addition to the adverse
events reported during clinical studies and listed above, the following adverse events have been
reported in post-marketing experience. Table 3 is based on post-market spontaneous adverse
event reports. The percentages shown are calculated by dividing the number of adverse events
reported to the company by the estimated number of patient years exposed to lacosamide.
Because these adverse events are reported spontaneously from a population of uncertain size, it
is not possible to reliably estimate their frequency. Furthermore, a causal relationship between
lacosamide and the emergence of these events has not been clearly established.
Table 3: Post-Market Spontaneous Adverse Event Reports
Adverse Events Reported Frequency
Uncommon
<1% and ≥0.1%
Rare
<0.1% and
≥0.01%
Very rare <0.01%
Immune system disorders
Drug hypersensitivity
reactions
X
Multiorgan hypersensitivity
reactions
1
X
Blood and lymphatic system disorders
Leukopenia
X
Thrombocytopenia
X
Agranulocytosis
X
Cardiovascular disorders
Bradycardia
X
Atrioventricular block
X
Atrial fibrillation
X
Atrial flutter
X
Cardiac arrest
X
Cardiac failure
X
Myocardial infarction
X

______________________________________________________________________________
Page 16 of 38
Adverse Events Reported Frequency
Uncommon
<1% and ≥0.1%
Rare
<0.1% and
≥0.01%
Very rare <0.01%
Ventricular tachyarrhythmia
X
Hepatobiliary disorders
Liver function test abnormal
X
Hepatic enzyme increased (> 2x ULN)
X
Hepatitis
X
Metabolism and nutrition disorders
Hyponatremia
X
Nervous system disorders
Ataxia
X
Syncope
X
Seizure
X
Psychiatric disorders
Euphoric mood
X
Suicide attempt
X
Suicidal ideation
X
Aggression
X
Agitation
X
Psychotic disorder
X
Insomnia
X
Hallucination
X
Skin and subcutaneous tissue disorders
Rash
X
Angioedema
X
Urticaria
X
Stevens-Johnson Syndrome
X
Toxic Epidermal Necrolysis
X
Alopecia
X
1
Includes related preferred term DRESS (Drug Reaction with Eosinophilia and Systemic Symptoms)
Cardiac disorders: Second and third degree AV block, ventricular tachyarrhythmia, atrial
fibrillation and atrial flutter associated with lacosamide treatment have been reported in post-
marketing experience (see WARNINGS AND PRECAUTIONS, Cardiac Rhythm and
Conduction Abnormalities).
______________________________________________________________________________
Page 17 of 38
Hepatic/Biliary/Pancreatic: Post-marketing reports of abnormal liver enzyme values, liver
injury, acute hepatic failure (including hepatic encephalopathy and hepatic coma) and jaundice
have been received in patients taking lacosamide either alone, or in conjunction with other
medications. Rare cases of clinically significant liver injury that were considered probably or
possibly related to lacosamide have been reported.
Nervous system disorders: Seizure. Cases of seizure worsening (including occurrence of status
epilepticus) have been reported.
DRUG INTERACTIONS
Lacosamide should be used with caution in patients treated with medicinal products known to be
associated with PR prolongation including sodium channel blocking antiepileptic drugs,
pregabalin, beta-blockers and in patients treated with antiarrhythmic drugs (see WARNINGS
AND PRECAUTIONS, Cardiac Rhythm and Conduction Abnormalities).
In Vitro Assessment of Drug Interactions
In vitro metabolism studies indicate that lacosamide does not induce the enzyme activity of drug
metabolizing cytochrome P450 isoforms CYP1A2, 2B6, 2C9, 2C19 and 3A4 at concentrations
(12.5 μg/mL) close to the human peak plasma concentration (10.9 μg/mL, C
max
, steady state at
maximum recommended human dose (MRHD) of 400 mg/day). At concentrations 10 times
higher (125 μg/mL), enzyme activities were less than 2-fold increased. Lacosamide did not
inhibit CYP 1A1, 1A2, 2A6, 2B6, 2C8, 2C9, 2D6, 2E1, 3A4/5 at concentrations up to 1000-fold
greater than the C
max
for 400 mg/day. The inhibitory concentrations (IC50) of CYP3A4, 3A5,
2C9 and 1A1 by lacosamide are at least 70-fold higher than the C
max
for 400 mg/day.
In vitro data suggest that lacosamide has the potential to inhibit CYP2C19 at therapeutic
concentrations (60% inhibition at 25μg/mL). However, an in vivo evaluation in healthy subjects
showed no inhibitory effect of lacosamide (600 mg/day administered as 300 mg BID dosing) on
the single dose pharmacokinetics of omeprazole (40 mg).
Lacosamide is a CYP2C19 substrate. The relative contribution of other CYP isoforms or non-
CYP enzymes in the metabolism of lacosamide is not clear.
Lacosamide was not a substrate or inhibitor for P-glycoprotein.
Since <15% of lacosamide is bound to plasma proteins, a clinically relevant interaction with
other drugs through competition for protein binding sites is unlikely.
In Vivo Assessment of Drug Interactions
Drug-drug interaction studies in healthy subjects showed no pharmacokinetic interactions
between lacosamide and carbamazepine, valproic acid, digoxin, metformin, omeprazole,
midazolam, or an oral contraceptive containing ethinylestradiol and levonorgestrel. There was no
evidence for any relevant drug-drug interaction of lacosamide with common AEDs in the
placebo-controlled adjunctive therapy clinical trials in patients with partial-onset seizures.

______________________________________________________________________________
Page 18 of 38
The lack of pharmacokinetic interaction does not rule out the possibility of pharmacodynamic
interactions, particularly among drugs that affect the heart conduction system.
Drug – Drug Interactions
Drug- Interaction Studies with AEDs:
Effect of lacosamide tablets on concomitant AEDs: Lacosamide tablets 400 mg/day had no
influence on the pharmacokinetics of 600 mg/day valproic acid and 400 mg/day carbamazepine
in healthy subjects.
The placebo-controlled adjunctive therapy clinical studies in patients with partial-onset seizures
showed that steady-state plasma concentrations of levetiracetam, carbamazepine, carbamazepine
epoxide, lamotrigine, topiramate, oxcarbazepine monohydroxy derivative (MHD), phenytoin,
valproic acid, phenobarbital, gabapentin, clonazepam, and zonisamide were not affected by
concomitant intake of lacosamide tablets at 200 to 600 mg/day.
Effect of concomitant AEDs on lacosamide tablets:
Drug-drug interaction studies in healthy subjects showed that 600 mg/day valproic acid had no
influence on the pharmacokinetics of 400 mg/day lacosamide tablets. Likewise, 400 mg/day
carbamazepine had no influence on the pharmacokinetics of lacosamide tablets (400 mg/day) in
a healthy subject study. Population pharmacokinetics results in patients with partial-onset
seizures showed small reductions (approximately 25% lower) in lacosamide plasma
concentrations when lacosamide tablets (200 to 600 mg/day) was co-administered with
carbamazepine, phenobarbital or phenytoin.
Drug-Drug Interaction Studies with Other Drugs:
Digoxin
Lacosamide tablets (400 mg/day) did not affect pharmacokinetics of digoxin (0.5 mg once daily)
in a study in healthy subjects. There was no effect of digoxin on the pharmacokinetics of
lacosamide.
Metformin
There were no clinically relevant changes in metformin levels following co-administration of
lacosamide tablets (400 mg/day). Metformin (500 mg three times a day) had no effect on the
pharmacokinetics of lacosamide (400 mg/day) in healthy subjects.
Omeprazole
Omeprazole is a CYP2C19 substrate and inhibitor.
Omeprazole (40 mg once daily) increased the AUC of lacosamide by 19% (300 mg, single dose),
which is unlikely to be clinically significant. Lacosamide (600 mg/day) did not affect the single-
dose pharmacokinetics of omeprazole (40 mg) in healthy subjects.
Midazolam

______________________________________________________________________________
Page 19 of 38
Midazolam is a CYP3A4 substrate.
Lacosamide tablets administered as a single 200 mg dose or repeated doses of 400 mg/day (200
mg BID) to healthy subjects had no clinically relevant effect on the AUC of midazolam, but
slightly increased the C
max
over time (30% after 13 days).
Warfarin
Co-administration of warfarin as a single 25 mg dose with lacosamide 400 mg/day (200 mg BID)
to healthy subjects had no clinically relevant change in the pharmacokinetics and
pharmacodynamics of warfarin.
Oral Contraceptives
In an interaction trial in healthy subjects, there was no clinically relevant interaction between
lacosamide (400 mg/day) and the oral contraceptives ethinylestradiol (0.03 mg) and
levonorgestrel (0.15 mg). Progesterone concentrations were not affected when the medicinal
products were co-administered (see WARNINGS AND PRECAUTIONS, Women of
Childbearing Potential/Contraception).
Drug-Food Interactions
Lacosamide tablets are completely absorbed after oral administration. Food does not affect the
rate or extent of absorption.
Drug-Herb Interactions
Interactions with herbal products have not been evaluated.
Drug-Laboratory Interactions
Interactions with laboratory tests have not been observed.
DOSAGE AND ADMINISTRATION
General Considerations
Alembic-Lacosamide may be taken with or without food.
Film-coated tablets
The film-coated tablets are taken orally twice a day. For further directions for use, see the
DOSAGE AND ADMINISTRATION, Recommended Dose and Dosage Adjustment section
of the product monograph.
Recommended Dose and Dosage Adjustment
Monotherapy
The recommended starting dose is 100 mg twice a day (200 mg/day), with or without food.
Depending on patient response and tolerability, the dose can be further increased at weekly
intervals by 50 mg twice a day (100 mg/day), to a maximum recommended maintenance daily
______________________________________________________________________________
Page 20 of 38
dose of 300 mg twice a day (600 mg/day). In the monotherapy trial, the majority of patients who
completed the Evaluation Phase of the study and remained seizure free received lacosamide 200
or 400 mg/day (see CLINICAL TRIALS).
In patients having reached lacosamide ≥400mg/day and who need an additional antiepileptic
drug, the dosing that is recommended for adjunctive therapy below should be followed.
Maximum recommended daily dose for adjunctive therapy is 400 mg/day.
Adjunctive Therapy
The recommended starting dose for Alembic-Lacosamide is 50 mg twice a day, with or without
food, which should be increased to an initial therapeutic dose of 100 mg twice a day after one
week. Depending on patient response and tolerability, the maintenance dose can be further
increased by 50 mg twice a day every week, to a maximum recommended daily dose of 400 mg
(200 mg twice a day). Doses above 400 mg/day do not confer additional benefit, are associated
with more severe and substantially higher frequency of adverse reactions and are not
recommended (see OVERDOSAGE, Non-acute Overdose in Humans).
Discontinuation
In accordance with current clinical practice, if Alembic-Lacosamide has to be discontinued, it is
recommended this be done gradually (e.g. taper the daily dose by 200 mg/week).
Initiation
Lacosamide therapy can be initiated with either oral or intravenous (IV) administration.
Patients with Renal Impairment
No dose adjustment is necessary in patients with mild or moderate renal impairment (creatinine
clearance (CL
CR
) >30 mL/min). A maximum dose of 300 mg/day is recommended for patients
with severe renal impairment (CL
CR
≤30 mL/min) and in patients with end-stage renal disease. In
all patients with any degree of renal impairment, the dose titration should be performed with
caution (see ACTION AND CLINICAL PHARMACOLOGY, Special Populations and
Conditions, Renal Impairment).
Following a 4-hour hemodialysis treatment, AUC of lacosamide tablets was reduced by
approximately 50%. Thus, dosage supplementation of up to 50% following hemodialysis may be
considered. Treatment of patients with end-stage renal disease should be made with caution as
there is limited clinical experience in subjects (n=8) and no experience in patients, and there is
accumulation of a metabolite (with no known pharmacological activity).
Patients with Hepatic Impairment
The dose titration should be performed with caution in patients with mild to moderate hepatic
impairment. A maximum dose of 300 mg/day is recommended for patients with mild or
moderate hepatic impairment. The pharmacokinetics of lacosamide tablets has not been
evaluated in severe hepatic impairment. Alembic-Lacosamide is not recommended in patients
with severe hepatic impairment (see ACTION AND CLINICAL PHARMACOLOGY,
Special Populations and Conditions, Hepatic Impairment).
Geriatrics (≥65 years of age)

______________________________________________________________________________
Page 21 of 38
Clinical experience with lacosamide tablets in elderly patients with epilepsy is limited. Although
no dose reduction is necessary in elderly patients, caution should be exercised during dose
titration and age-associated decreased renal clearance with an increase in AUC levels should be
considered in elderly patients (see ACTION AND CLINICAL PHARMACOLOGY, Special
Populations and Conditions, Geriatrics).
Pediatrics (<18 years of age)
The safety and effectiveness of lacosamide tablets in pediatric patients <18 years has not been
established, and therefore its use in this patient population is not indicated (see INDICATIONS
and WARNINGS AND PRECAUTIONS, Special Populations, Pediatrics).
Missed Dose
If the patient misses a dose by a few hours, they should be instructed to take Alembic-
Lacosamide as soon as they remember. If it is close to their next dose, they should be instructed
to take their medication at the next regular time. Patients should not take two doses at the same
time.
OVERDOSAGE
For management of a suspected drug overdose, contact your regional Poison Control
Centre.
Signs, Symptoms, and Laboratory Findings of Acute Overdose in Humans
Lowest known lethal dose: estimated 7g (age 56, male) (see below)
The types of adverse events experienced by patients exposed to acute lacosamide tablets
overdose during pre-marketing clinical trials were mostly similar to those observed in patients
administered therapeutic doses of lacosamide tablets.
Following doses above 400 mg/day up to 800 mg/day, the more commonly reported adverse
events were related to the central nervous system (dizziness, headache, fatigue) and the
gastrointestinal system (nausea and vomiting).
There has been a single case of intentional overdose in a clinical trial by a patient who self-
administered 12000 mg lacosamide tablets along with large doses of zonisamide, topiramate, and
gabapentin. The patient was initially comatose, had second degree AV block, seizures, and was
hospitalized. An EEG revealed epileptic waveforms. The patient recovered 2 days later. From the
9 cases in pre-marketing clinical studies exposed to an acute lacosamide tablets overdose >800
mg, none resulted in death.
Decreased visual acuity was reported in one case from a clinical trial of lacosamide tablets
overdose at 1050 mg within a single day. The event was considered non-serious and resolved the
following day.

______________________________________________________________________________
Page 22 of 38
In post-marketing experience, events reported following acute single overdoses ranging between
800 mg and 12000 mg were dizziness, nausea, vision abnormalities, seizures (generalized tonic-
clonic seizures, status epilepticus) cardiac conduction disorders, shock and coma. Fatal cardiac
arrest, shock and multi-organ failure were reported following acute overdoses of 7000 mg of
lacosamide tablets.
There have also been post-marketing reports of seizures and loss of consciousness in patients
with acute single lacosamide tablets overdoses between 400 mg and 1200 mg.
Non-acute Overdose in Humans
Non-acute lacosamide tablets overdose has also been reported. The great majority of these cases
were in patients receiving daily lacosamide tablets doses ≤ 800 mg for various durations.
Adverse events observed after supratherapeutic doses included vision abnormalities (blurred
vision, diplopia, nystagmus), cardiac arrhythmia, status epilepticus, convulsions and increased
seizure frequency and duration. For example, in one case, after receiving lacosamide tablets 900
mg/day for 23 days, a patient experienced increased seizure duration and frequency. The
maximum recommended daily dose of Alembic-Lacosamide as adjunctive and monotherapy in
patients with partial onset seizures is 400 mg and 600 mg respectively. Higher doses are not
recommended (see DOSAGE AND ADMINISTRATION).
Treatment or Management of Overdose
There is no specific antidote for overdose with lacosamide tablets. Standard decontamination
procedures should be followed. General supportive care of the patient is indicated including
monitoring of vital signs and observation of the clinical status of patient. A Poison Control
Centre should be contacted for up to date information on the management of overdose with
Alembic-Lacosamide. Standard hemodialysis procedures result in significant clearance of
lacosamide tablets (reduction of systemic exposure by 50% in 4 hours). Hemodialysis has not
been performed in the few known cases of overdose, but may be helpful based on the patient's
clinical state or in patients with significant renal impairment.
ACTION AND CLINICAL PHARMACOLOGY
Mechanism of Action
The precise mechanism by which lacosamide exerts its antiepileptic effect in humans is unknown
(see Product Monograph, Part II: DETAILED PHARMACOLOGY, Preclinical Pharmacology,
for experimental in vitro and in vivo data in animals).
Pharmacodynamics
A pharmacokinetic-pharmacodynamic (efficacy) analysis was performed based on the pooled
data from the 3 controlled adjunctive therapy efficacy trials for partial-onset seizures.
Lacosamide exposure is correlated with the reduction in seizure frequency. However, in group
analyses, doses above 400 mg/day, when administered as adjunctive therapy, do not appear to
confer additional benefit and are associated with more severe and substantially higher frequency
of adverse reactions.

______________________________________________________________________________
Page 23 of 38
Cardiac Electrophysiology
Electrocardiographic effects of lacosamide tablets were determined in a double-blind,
randomized clinical pharmacology ECG trial of 247 healthy subjects. Chronic oral doses of 400
and 800 mg/day were compared with placebo and a positive control (400 mg moxifloxacin).
Lacosamide did not prolong QTc interval and did not have a dose-related or clinically important
effect on QRS duration. Lacosamide produced a dose-related increase in mean PR interval. At
steady-state, the time of the maximum observed mean PR interval corresponded with t
max
. The
placebo-subtracted maximum increase in PR-interval (at t
max
) was 7.3 ms for the 400 mg/day
group and 11.9 ms for the 800 mg/day group.
For patients with partial-onset seizures who participated in the controlled adjunctive therapy
trials, the placebo-subtracted maximum increase in PR interval for a 400 mg/day lacosamide
dose was 3.1 ms. For patients with diabetic neuropathic pain who participated in controlled trials,
the placebo-subtracted maximum increase in PR-interval for a 400 mg/day lacosamide dose was
8.3 ms (see WARNINGS AND PRECAUTIONS and ADVERSE REACTIONS).
Pharmacokinetics
The pharmacokinetics of lacosamide has been studied in healthy adult subjects (age range 18 to
87), adults with partial-onset seizures, adults with diabetic neuropathy, and subjects with renal
and hepatic impairment. A summary of lacosamide’s pharmacokinetic parameters in healthy
subjects is provided in Table 4.
Lacosamide is completely absorbed after oral administration with negligible first-pass effect with
a high absolute bioavailability of approximately 100%. The maximum lacosamide plasma
concentrations occur approximately 0.25 to 4 hours post-dose after oral dosing, and elimination
half-life is approximately 13 hours. Steady state plasma concentrations are achieved after 3 days
of twice daily repeated administration. Pharmacokinetics of lacosamide is dose proportional
(100-800 mg) and time invariant, with low inter- and intra-subject variability. Compared to
lacosamide, the major metabolite, O-desmethyl metabolite, has a longer T
max
(0.5 to 12 hours)
and elimination half-life (15-23 hours) but has no known pharmacologic activity.
Table 4: Summary of Lacosamide’s Pharmacokinetic Parameters in Healthy Subjects
C
max
(µg/mL)
Arithmetic
Mean
t
1/2
(h)
Arithmetic
Mean
AUC
T
(µg/mL*h)
Arithmetic
Mean
t
max
(h)
Median
(range)
Oral Tablet 200mg 5.03 13.96 88.61
0.75
(0.25-4.00)
Absorption: Lacosamide is rapidly and completely absorbed after oral administration. The oral
bioavailability of lacosamide tablets is approximately 100%. Following oral administration, the
plasma concentration of unchanged lacosamide increases rapidly and reaches C
max
about 0.25 to
4 hours post-dose. Food does not affect the rate and extent of absorption.

______________________________________________________________________________
Page 24 of 38
After intravenous administration (30-60 minutes), C
max
is reached at the end of infusion. The
plasma concentration increases proportionally with dose after oral (100-800 mg) and intravenous
(50-300 mg) administration.
Distribution: The volume of distribution is approximately 0.6 L/kg. Lacosamide is less than
15% bound to plasma proteins.
Metabolism: The metabolism of lacosamide has not been completely characterized.
Approximately 95% of the dose is excreted in the urine as drug and metabolites. The major
compounds excreted in urine are unchanged lacosamide (approximately 40% of the dose) and its
O-desmethyl metabolite, which has no known pharmacological activity (less than 30%). A
structurally unknown polar fraction (about 20%) was also found in urine, but was detected only
in small amounts (0-2%) in human plasma of some subjects. Small amounts (0.5-2%) of
additional metabolites were also found in the urine. The plasma exposure of the major human
metabolite (AUC), O-desmethyl-lacosamide, is approximately 15% of the drug product,
lacosamide.
CYP2C19, CYP2C9 and CYP3A4 are mainly responsible for the formation of the O-desmethyl
metabolite. However, no clinically relevant difference in lacosamide exposure was observed
comparing its pharmacokinetics in extensive metabolisers (EMs, with a functional CYP2C19)
and poor metabolisers (PMs, lacking a functional CYP2C19). Furthermore, an interaction trial
with omeprazole (CYP2C19-inhibitor) demonstrated no clinically relevant changes in
lacosamide plasma concentrations indicating that the importance of this pathway is minor. No
other enzymes have been identified to be involved in the metabolism of lacosamide.
Elimination: Lacosamide is primarily eliminated from the systemic circulation by renal
excretion and biotransformation. After oral and intravenous administration of 100 mg
radiolabeled lacosamide, approximately 95% of radioactivity administered was recovered in the
urine and less than 0.5% in the feces. The elimination half-life of the unchanged drug is
approximately 13 hours and is not altered by different doses, multiple dosing or intravenous
administration. The pharmacokinetics are dose-proportional and time-invariant, with low intra-
and inter-subject variability. Following twice daily dosing, steady state plasma concentrations
are achieved after a 3 day period. The plasma concentration increases with an accumulation
factor of approximately 2.
Special Populations and Conditions
Geriatrics (≥ 65 years of age): In a study in elderly men and women, the AUC was about 30
and 50% increased compared to young men, respectively. This is partly related to lower body
weight. The body weight normalized difference is 26 and 23%, respectively. An increased
variability in exposure was also observed. The renal clearance of lacosamide was only slightly
reduced in elderly subjects in this study.
Pediatrics (<18 years of age): Pharmacokinetics of lacosamide have not been established in
pediatric patients.

______________________________________________________________________________
Page 25 of 38
Gender: Lacosamide tablets clinical trials indicate that gender does not have a clinically relevant
influence on the pharmacokinetics of lacosamide.
Race: Approximately 90% of the patient population in epilepsy trials was Caucasian. There are
no clinically relevant differences in the pharmacokinetics of lacosamide between Asian, Black,
and Caucasian subjects.
Renal impairment: Lacosamide and its major metabolite are eliminated from the systemic
circulation primarily by renal excretion.
The AUC of lacosamide was increased approximately 25% in mildly (CL
CR
50-80 mL/min) and
moderately (CL
CR
30-50 mL/min), and 60% in severely (CL
CR
≤30mL/min) renally impaired
patients compared to subjects with normal renal function (CL
CR
>80mL/min), whereas C
max
was
unaffected. No dose adjustment is considered necessary in mildly and moderately renal impaired
subjects. A maximum dose of 300 mg/day is recommended for patients with severe renal
impairment (CL
CR
≤30mL/min) and in patients with end stage renal disease.
Hemodialysis
Lacosamide is effectively removed from plasma by hemodialysis. Following a 4-hour
hemodialysis treatment, AUC of lacosamide is reduced by approximately 50%. Therefore dosage
supplementation of up to 50% following hemodialysis should be considered. In all renal
impaired patients, the dose titration should be performed with caution.
Hepatic impairment: Lacosamide undergoes metabolism. Subjects with moderate hepatic
impairment (Child-Pugh B) showed higher plasma concentrations of lacosamide (approximately
50-60% higher AUC compared to healthy subjects). A maximum dose of 300 mg/day is
recommended for patients with mild to moderate hepatic impairment. Patients with mild to
moderate hepatic impairment should be titrated with caution and observed closely during dose
titration. Patients with co-existing hepatic and renal impairment of any degree should also be
monitored closely during dose titration.
The pharmacokinetics of lacosamide has not been evaluated in patients with severe hepatic
impairment. Lacosamide tablets use in patients with severe hepatic impairment is not
recommended (see DOSAGE AND ADMINISTRATION and ACTION AND CLINICAL
PHARMACOLOGY, Special Populations and Conditions, Renal Impairment).
CYP2C19 Polymorphism: There are no clinically relevant differences in the pharmacokinetics
of lacosamide between CYP2C19 poor metabolizers and extensive metabolizers. Results from a
trial in poor metabolizers (PM) (N=4) and extensive metabolizers (EM) (N=8) of cytochrome
P450 (CYP) 2C19 showed that lacosamide plasma concentrations were similar in PMs and EMs,
but plasma concentrations and the amount excreted into urine of the O-desmethyl metabolite
were about 70% reduced in PMs compared to EMs.
STORAGE AND STABILITY
Store at room temperature (15 – 30°C).
______________________________________________________________________________
Page 26 of 38
DOSAGE FORMS, COMPOSITION AND PACKAGING
Lacosamide tablets
Alembic-Lacosamide film-coated tablets are supplied as follows:
50 mg tablet: Alembic-Lacosamide tablets 50 mg are pink, oval, film-coated tablet debossed
with “423” on one side and plain on other side. They are supplied in high density polyethylene
(HDPE) bottles of 60.
100 mg tablet: Alembic-Lacosamide tablets 100 mg are dark yellow, oval, film-coated tablet
debossed with “L424” on one side and plain on other side. They are supplied in high density
polyethylene (HDPE) bottles of 60.
150 mg tablet: Alembic-Lacosamide tablets 150 mg are salmon, oval, film-coated tablets
debossed with “L425” on one side and plain on other side. They are supplied in high density
polyethylene (HDPE) bottles of 60.
200 mg tablet: Alembic-Lacosamide tablets 200 mg are blue, oval, film-coated tablets debossed
with “L426” on one side plain on other side. They are supplied in high density polyethylene
(HDPE) bottles of 60.
Alembic-Lacosamide tablets contain the following nonmedicinal ingredients: microcrystalline
cellulose, crospovidone, hydroxypropyl cellulose, low-substituted hydroxypropyl cellulose,
colloidal silicon dioxide, magnesium stearate, hypromellose, polyethylene glycol, talc, titanium
dioxide, and dye pigments as specified below:
Alembic-Lacosamide tablets are supplied as debossed tablets and contain the following coloring
agents:
50 mg tablets: FD&C Blue #2 aluminum lake, iron oxide red, iron oxide black
100 mg tablets: iron oxide yellow
150 mg tablets: iron oxide yellow, iron oxide red, iron oxide black
200 mg tablets: FD&C Blue #2 aluminum lake

______________________________________________________________________________
Page 27 of 38
PART II: SCIENTIFIC INFORMATION
PHARMACEUTICAL INFORMATION
Drug Substance
Common name: lacosamide
Chemical name: (R)-2-acetamido-N-benzyl-3-methoxypropionamide (IUPAC)
Molecular formula and molecular mass: C
13
H
18
N
2
O
3
250.30 g/mol
Structural formula:
Physicochemical properties: Lacosamide is a white to off-white crystalline powder.
Freely soluble in dimethyl sulfoxide and in ethanol. The
melting point of lacosamide is about 145°C.
CLINICAL TRIALS
Comparative Bioavailability Studies
A double blind, randomized, two-period, two-treatment, two-sequence, crossover, balanced,
single dose oral bioequivalence study of Lacosamide Tablets 200 mg (manufactured by Alembic
Pharmaceuticals Limited, India) and VIMPAT
®
(lacosamide) 200 mg tablets (UCB Canada Inc.)
was conducted in 16 healthy adult male subjects. The test and reference products were
administered as 1 x 200 mg doses under fasting conditions. A summary of the bioavailability
data is presented in the tables below
Table 5: Summary Table of Comparative Bioavailability Data for Lacosamide
LACOSAMIDE
(1 x 200 mg)
From measured data
Geometric Mean
Arithmetic Mean (CV %)
Parameter Test* Reference
†
% Ratio of
Geometric Means
Confidence
Interval
AUC
T
(µg.hr/ mL)
99.7
101.3 (17.5)
101.2
102.6 (16.7)
98.6 96.5%; 100.7%
AUC
I
(µg.hr/ mL)
103.1
105.0 (18.9)
104.4
106.1 (18.0)
98.7 96.8%; 100.8%

______________________________________________________________________________
Page 28 of 38
LACOSAMIDE
(1 x 200 mg)
From measured data
Geometric Mean
Arithmetic Mean (CV %)
Parameter Test* Reference
†
% Ratio of
Geometric Means
Confidence
Interval
C
max
(µg/ mL)
5.5
5.6 (18.6)
5.4
5.5 (14.7)
101.7 93.5%; 110.6%
T
max
§
(h)
1.0
(0.3 - 2.3)
1.5
(0.3 - 3.0)
T
½
€
(h)
14.2 (22.6) 14.1 (18.1)
* Lacosamide Tablets 200 mg by Alembic Pharmaceuticals Ltd.
†
VIMPAT
®
(lacosamide) 200 mg tablets manufactured by UCB Canada Inc., were purchased in Canada.
§
Expressed as the median (range) only.
€
Expressed as the arithmetic mean (CV%) only.
Monotherapy
Study Demographics and Trial Design
The efficacy of lacosamide as monotherapy in partial-onset seizures was established in a
randomized, double-blind, double-dummy, positive-controlled, non-inferiority multicenter trial
in which 444 patients received lacosamide (dose range: 200 - 600 mg daily) or controlled-release
carbamazepine (dose range: 400 - 1200 mg daily; n=442). Only patients with newly or recently
diagnosed epilepsy participated in the study. Patients had to present with at least two seizures
occurring in the last 12 months prior to study entry. Patients previously treated chronically (> 2
weeks) for epilepsy with any AED in the last 6 months before study entry were not permitted in
the study. Patients ranged in age between 16 and 87 years (mean: 42 years). A total of 27
pediatric and 62 elderly patients took at least one dose of lacosamide 200 - 600 mg/day.
Approximately 54% of the patients were male. In the elderly patient population, the maintenance
lacosamide dose was 200 mg/day in 55 patients (88.7%), 400 mg/day in 6 patients (9.7%) and
the dose was escalated to 600 mg/day in 1 patient (1.6%).
The study compared doses of lacosamide 200, 400, or 600 mg/day to carbamazepine (controlled
release) 400, 800, or 1200 mg/day, used as monotherapy. The step-wise design for the study
employed 3 predefined target dose levels for both lacosamide and carbamazepine (controlled
release). Patients initiated treatment with lacosamide 100 mg/day or carbamazepine (controlled
release) 200 mg/day and study medication was subsequently up-titrated to the first target
therapeutic dose level of lacosamide 200 mg/day or carbamazepine (controlled release) 400
mg/day. In case this dose did not control seizures during the 6-month Evaluation Phase of the
study, the dose was increased to lacosamide 400 mg/day or carbamazepine (controlled release)
800 mg/day, and if this dose did not control seizures, the dose was increased to lacosamide 600
mg/day or carbamazepine (controlled release) 1200 mg/day. Following the Evaluation Phase at a
specific dose (200, 400, or 600 mg/day) for 26 weeks, patients who had remained seizure-free,
were entered into the Maintenance Phase for an additional 26 weeks.

______________________________________________________________________________
Page 29 of 38
The study completion rates were 66.9% (n=210) for the lacosamide 200 mg/day dose level,
47.1% (n=41) for the 400 mg/day dose level and 34.9% (n=15) for the 600 mg/day dose level.
Approximately 95% of the patients, who completed the 6-month Evaluation Phase and remained
seizure free, received daily lacosamide doses of 200 or 400 mg. In the study, 19 patients received
600 mg/day and remained seizure free.
The primary efficacy variable was the proportion of patients remaining seizure free for 6
consecutive months (26 consecutive weeks) of treatment following stabilization at the last
evaluated dose for each patient.
Study Results
Lacosamide met the pre-defined non-inferiority criteria and was considered to be non-inferior to
carbamazepine (controlled release) based on the primary efficacy end-point.
Among the total of all lacosamide -treated patients (n=444), approximately 56% (n=249), 13%,
(n=59) and 4% (n=19) completed the 6-month Evaluation Phase and remained seizure free at the
last evaluated lacosamide dose of 200 mg/day, 400 mg/day, and 600 mg/day, respectively.
The number and percentage of patients who completed the 6-month seizure freedom Evaluation
Phase and remained seizure free during this period are presented by treatment group overall and
by the last evaluated dose in Table 5 below. Overall, the proportion of patients who completed 6
months and remained seizure free at the last dose level was similar between the lacosamide
(73.6%) and carbamazepine (controlled release) (69.7%) treatment groups.
Table 6: Number and Percentage of the Patients Who Completed 6 Month Evaluation
Phase and Remained Seizure Free at the Last Evaluated Dose based on Full Analysis Set.
Last evaluated dose level 6-months
Parameter Lacosamide CBZ-CR
Overall, n 444 442
Seizure free for 6 months, n (%) 327 (73.6) 308 (69.7)
Dose level 1, n 314 324
Seizure free for 6 months, n (%) 249 (79.3) 235 (72.5)
Dose level 2, n 87 85
Seizure free for 6 months, n (%) 59 (67.8) 60 (70.6)
Dose level 3, n 43 33
Seizure free for 6 months, n (%) 19 (44.2) 13 (39.4)
CBZ-CR=carbamazepine (controlled release)
Note: Dose level 1= Lacosamide 200mg/day or CBZ-CR 400mg/day; Dose level 2= Lacosamide
400mg/day or CBZ-CR 800mg/day; Dose level 3= Lacosamide 600mg/day or CBZ-CR 1200mg/day.
Other efficacy end-points such as estimates of 12-month seizure freedom rates were supportive
of the primary efficacy end-point.
The 6-month seizure freedom rates observed in patients aged 65 years or older were similar
between both treatment groups and in the overall patient population.

______________________________________________________________________________
Page 30 of 38
Adjunctive Therapy
Study Demographics and Trial Design
The efficacy of lacosamide as adjunctive therapy in partial-onset seizures was established in
three 12-week, randomized, double-blind, placebo-controlled, multicenter trials involving 944
adult patients that were randomized to receive lacosamide (and 364 adult patients that were
randomized to placebo). Patients had partial-onset seizures with or without secondary
generalization and were not adequately controlled with 1 to 3 concomitant AEDs. During an 8-
week baseline period, patients were required to have an average of ≥4 partial-onset seizures per
28 days with no seizure-free period exceeding 21 days. In these 3 trials, patients ranged in age
between 16 and 71 years (mean: 38.6 years of age), had a mean duration of epilepsy of 24 years
and a median baseline seizure frequency ranging from 10 to 17 per 28 days. A total of 10
patients aged 16 to 17 years were enrolled in the trials. Fifty-one percent of the patients were
female. Overall, 84% of patients were taking 2 to 3 concomitant AEDs. Of these patients, 18%
were also receiving concurrent vagal nerve stimulation (VNS).
Study 1 compared doses of lacosamide 200, 400, and 600 mg/day and placebo in 107, 108, 106,
and 97 randomized patients, respectively. Study 2 compared doses of lacosamide 400 and 600
mg/day and placebo in 204, 97, and 104 randomized patients, respectively. Study 3 compared
doses of lacosamide 200 and 400 mg/day and placebo in 163, 159, and 163 randomized patients,
respectively. Following the 8-week Baseline Phase, patients were randomized and up-titrated by
initiating treatment at 100 mg/day (50 mg BID), and increased in weekly increments of 100
mg/day to the target dose (a 1-step back-titration of lacosamide 100 mg/day or placebo was
allowed in the case of intolerable adverse events at the end of the Titration Phase). The Titration
Phase lasted 6 weeks in Studies 1 and 2, and 4 weeks in Study 3. Following the Titration Phase,
patients received a stable dose of lacosamide for 12 weeks (Maintenance Phase). Among the
patients randomized to lacosamide, 76% completed the Treatment Phase (Titration and
Maintenance).
The primary efficacy end-point in all three trials was the reduction in seizure frequency per 28
days from Baseline to the Maintenance Phase in lacosamide arm(s) as compared to placebo. The
50% responder rate (percent of patients with at least 50% reduction in seizure frequency from
Baseline to the Maintenance Phase) as compared to placebo was a secondary endpoint.
Study Results
A statistically significant effect (in the reduction of seizure frequency from Baseline to the
Maintenance Phase) was observed with lacosamide tablets doses of 200 mg/day (Study 3), 400
mg/day (Studies 1, 2, and 3), and 600 mg/day (Studies 1 and 2). The 50% responder rates for
lacosamide tablets doses of 400 mg and 600 mg/day were also statistically significant compared
to placebo (see Table 7).
Table 7: Median Percent Reduction in Partial Seizure Frequency per 28 days and 50%
Responder Rates from Baseline to the Maintenance Phase (ITT Population).
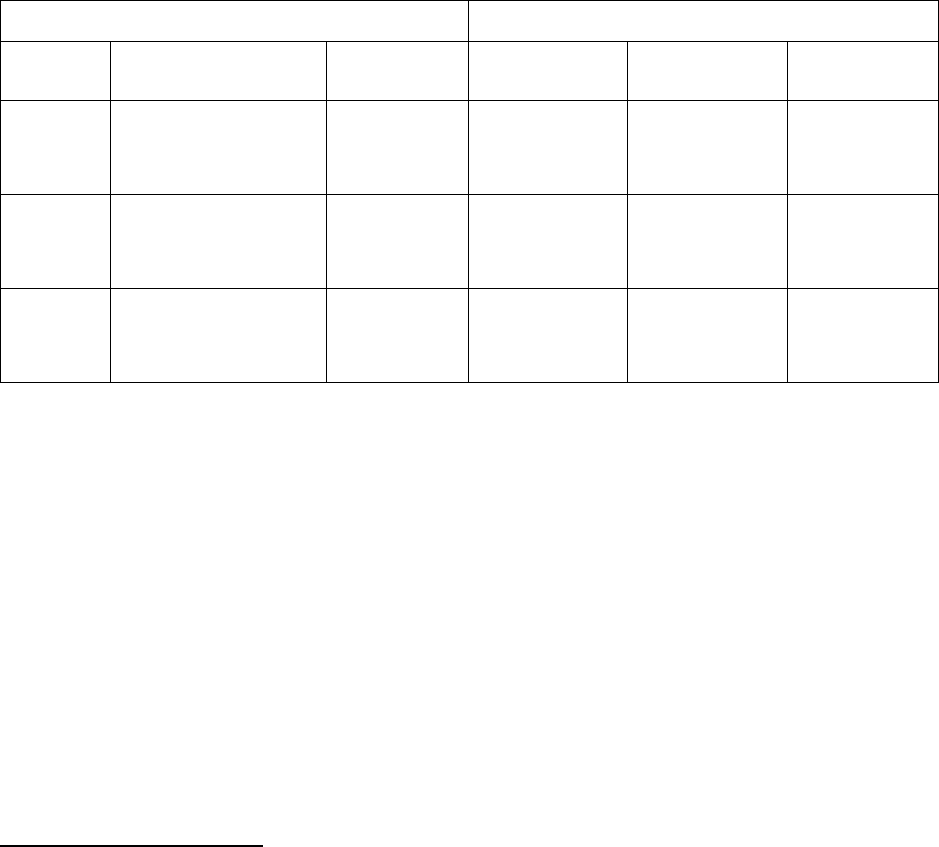
______________________________________________________________________________
Page 31 of 38
AED’s + Lacosamide (mg/day)
Study Efficacy results AED’s +
Placebo
200 400 600
1
n
Median % Reduction
50% Responders
96
10%
21.9%
107
26%
32.7%
107
39%**
41.1%**
105
40%**
38.1%*
2
n
Median % Reduction
50% Responders
104
20.8%
18.3%
--
--
--
201
37.3%**
38.3%**
97
37.8%**
41.2%**
3
n
Median % Reduction
50% Responders
159
20.5%
25.8%
160
35.3%*
35.0%
158
36.4%*
40.5%**
--
--
--
*Significant at the 0.05 level; ** Significant at the 0.01 level.
Significance reflects the percent reduction over placebo which is based on log-transformed seizure frequency from
pairwise treatment analysis of covariance (ANCOVA) models with terms for treatment, pooled site, and the baseline
period measurement and pairwise treatment logistic regression models with terms for treatment and pooled site.
A statistically significant reduction in seizure frequency from Baseline to the Treatment Phase
(i.e. Titration Phase + Maintenance Phase) was also observed with lacosamide tablets doses of
200 mg/day (Study 3), 400 mg/day (Studies 1, 2, and 3), and 600 mg/day (Studies 1 and 2)
compared to placebo. The 50% responder rates for lacosamide tablets doses of 400 mg and 600
mg/day were also statistically significant compared to placebo.
There were no significant differences in seizure control as a function of gender. Data on race
were limited (8.3% of the patients were non-Caucasian).
DETAILED PHARMACOLOGY
Preclinical Pharmacology
In vitro electrophysiological studies have shown that lacosamide selectively enhances slow
inactivation of voltage-gated sodium channels, resulting in reduced hyperexcitability of neuronal
membranes and inhibition of repetitive neuronal firing.
Lacosamide protected against seizures in a broad range of rodent models (mice and rats) of
partial and primary generalized seizures and delayed kindling development. In non-clinical
experiments lacosamide in combination with levetiracetam, carbamazepine, phenytoin,
valproate, lamotrigine, topiramate or gabapentin showed synergistic or additive anticonvulsant
effects. Lacosamide was not effective in the rat WAG/rij model of absence epilepsy and caused
mild dose-dependent increases in the number of characteristic EEG spike wave discharges for
one hour after single intraperitoneal doses of 3-30 mg/kg. A similar phenomenon also occurs in
WAG/rij rats given the other antiepileptic drugs phenytoin and carbamazepine.
A safety pharmacology study with intravenous administration of lacosamide at doses of 2-12
mg/kg in anesthetized beagle dogs showed transient increases in PR interval and QRS complex
duration and decreases in blood pressure most likely due to a cardiodepressant action as

______________________________________________________________________________
Page 32 of 38
indicated by decreases in cardiac output. There was evidence of a dose relationship. One high
dose dog (12 mg/kg) died due to a marked and sustained drop in blood pressure followed by
cardiac arrest. At the low dose, these transient changes started in the same plasma lacosamide
concentration range as after maximum recommended clinical dosing (300 mg BID).
Progressively reduced systolic, diastolic, and mean arterial blood pressure was also seen in
anesthetized Cynomolgus monkeys given up to 4 sequential intravenous lacosamide doses of 15
mg/kg. In anesthetized dogs given intravenous doses of 15-45 mg/kg (given as 1 to 3 sequential
doses) and anaesthetized monkeys given intravenous doses of 30-120 mg/kg (given as 1 to 4
sequential doses), slowing of atrial and ventricular conductivity, atrioventricular block and
atrioventricular dissociation were seen. In an in vitro assay conducted in HEK293 cells that
stably express the human-ether-à-go-go related gene (hERG), a weak 7% inhibition of hERG
current was seen only at the highest concentration (3000 μmol/L) tested. This is consistent with
the absence of changes in QT interval in safety pharmacology studies conducted in dogs and
monkeys.
TOXICOLOGY
In the toxicity studies, the plasma concentrations of lacosamide obtained were similar or only
marginally higher than those observed in patients, which leaves low or non-existing margins to
human exposure.
Acute Toxicity
Results from acute oral dose toxicity studies with lacosamide indicate a no-observed-effect-level
(NOEL) of 31.6 mg/kg in both mice and rats. The estimated LD50 values were 383 and 253
mg/kg for mice and rats, respectively. After intravenous administration the NOELs were 10 and
25 mg/kg and the estimated LD50 values were 178 and >100 mg/kg for mice and rats,
respectively. In acute toxicity studies, clinical signs at high doses included exaggerated
pharmacodynamic effects of lacosamide on the CNS such as reduced motility, ataxia,
abdominal/lateral position, loss of righting reflex, reduced muscle tone, hind limb weakness,
tremor, dyspnea and convulsions.
Long Term Toxicity
In repeated oral dose studies, lacosamide caused convulsions in mice, rats, rabbits, and dogs after
oral dosing at C
max
exposures generally only slightly higher than the C
max
at steady state of 14.5
μg/mL after the maximum recommended human dose of 300 mg BID in patients. The C
max
ratios
were as low as 3.4 in mice, 1.1 in rats, 1.8 in rabbits, and 1.4 in adult and juvenile dogs at the
lowest dose causing convulsions and as low as 1.9 in mice, less than 1.1 in rats, 0.9 in rabbits,
1.0 in adult dogs, and 0.6 in juvenile dogs at the highest dose level not associated with
convulsions. The convulsions usually occurred in the context of other significant clinical signs
including one or more of tremors, ataxia, hypoactivity, and recumbency, which also occurred at
dose levels not associated with convulsions.
Consistent with the safety pharmacology studies, lacosamide caused 13%-37% decreases in
systolic blood pressure in females in the 12 month chronic dog toxicity study at dose levels of
10-25 mg/kg/day with the C
max
at 10 mg/kg equivalent to that of humans given the maximum
recommended dose of 300 mg BID.

______________________________________________________________________________
Page 33 of 38
In the repeated dose toxicity studies, mild reversible liver changes were observed in rats starting
at about 2 times the clinical exposure. These changes included an increased organ weight,
hypertrophy of hepatocytes, increases in serum concentrations of liver enzymes and increases in
total cholesterol and triglycerides. Apart from the hypertrophy of hepatocytes, no other
histopathologic changes were observed.
Reproduction Studies
In reproductive and developmental toxicity studies in rodents and rabbits, no teratogenic effects
but an increase in numbers of stillborn pups and pup deaths in the peripartum period, and slightly
reduced live litter sizes and pup body weights were observed at maternal toxic doses in rats
corresponding to clinically relevant plasma exposure levels. Since higher exposure levels could
not be tested in animals due to maternal toxicity, data are insufficient to fully characterize the
embryofetotoxic and teratogenic potential of lacosamide. Studies in pregnant rats revealed that
lacosamide and/or its metabolites readily crossed the placental barrier.
Oral administration of lacosamide (30, 90, or 180 mg/kg/day) to rats during the neonatal and
juvenile periods of postnatal development resulted in decreased brain weights and long-term
neurobehavioral changes (altered open field performance, deficits in learning and memory). The
relevance of these observations remains equivocal. However, potential adverse effects on CNS
development cannot be ruled out. The early postnatal period in rats is generally thought to
correspond to late pregnancy in humans in terms of brain development. The no-effect dose for
developmental neurotoxicity in rats was associated with a plasma lacosamide AUC
approximately 0.4 times that in humans at the MRHD of 600 mg/day.
Carcinogenicity
There was no evidence of drug related carcinogenicity in mice or rats. Mice and rats received
lacosamide once daily by oral administration for 104 weeks at doses producing plasma exposures
(AUC) up to approximately 1 and 2.3 times, respectively, the plasma AUC in humans at the
maximum recommended human dose (MRHD) of 600 mg/day.
Mutagenicity
Lacosamide was negative in an in vitro Ames test and an in vivo mouse micronucleus assay and
an in vivo unscheduled DNA synthesis (UDS) test. In the in vivo tests, plasma exposures (AUC)
correspond to up to approximately 3 times the plasma AUC in humans at the maximum
recommended human dose (MRHD) of 600 mg/day. Lacosamide induced a positive response in
the in vitro mouse lymphoma assay at excessively high concentrations (i.e. at concentrations
above the maximum recommended concentration of 10 mM).
______________________________________________________________________________
Page 34 of 38
REFERENCES
Baulac M, Rosenow F, Toledo M, Terada K, Li T, De Backer M, Werhahn KJ, Brock M.
Efficacy, safety, and tolerability of lacosamide monotherapy versus controlled-release
carbamazepine in patients with newly diagnosed epilepsy: a phase 3, randomised, double-blind,
non-inferiority trial. Lancet Neurol 2017; 16: 43-54.
Ben-Menachem E, Biton V, Jatuzis D, Abou-Khalil B, Doty P, Rudd GD. Efficacy and safety of
oral lacosamide as adjunctive therapy in adults with partial-onset seizures. Epilepsia 2007; 1-10
48(7): 1308-1317. (Study 1)
Ben-Menachem E. Lacosamide: An investigational drug for adjunctive treatment of partial-onset
seizures. Drugs of Today 2008, 44 (1): 35-40.
Beyreuther BK, Freitag J, Heers C, Krebsfänger N, Scharfenecker U, Stöhr T. Lacosamide: A
Review of Preclinical Properties. CNS Drug Reviews 2007; Vol.13, No. 1, pp.21-42.
Biton V, Rosenfeld WE, Whitesides J, Fountain NB, Vaiciene N, Rudd GD. Intravenous
lacosamide as replacement for oral lacosamide in patients with partial-onset seizures. Epilepsia
2008; 49(3):418-424.
Chung S, Sperling MR, Biton V, Krauss G, Hebert D, Rudd GD, Doty P. Lacosamide as
adjunctive therapy for partial-onset seizures: A randomized controlled trial. Epilepsia 2010,
51(6):958–967. (Study 2)
Errington AC, Stöhr T, Heers C, Lees G. The investigational anticonvulsant LCM selectively
enhances slow inactivation of voltage-gated sodium channels. Mol Pharmacol 2008; 73:157-169.
Halász P, Kälviäinen R, Mazurikiewicz-Beldzińska M, Rosenow F, Doty P, Hebert D, Sullivan
T. Adjunctive lacosamide for partial-onset seizures: Efficacy and safety results from a
randomized controlled trial. Epilepsia 2009; 50(3): 443-453. (Study 3)
Product monograph of
Pr
VIMPAT
®
of UCB Canada Inc.; October 11, 2018, control number
218312.

IMPORTANT: PLEASE READ
______________________________________________________________________________
Page 35 of 38
PART III: CONSUMER INFORMATION
Pr
Alembic-Lacosamide
(Lacosamide Tablets)
This leaflet is part III of a three-part “Product
Monograph” published when Alembic-Lacosamide
was approved for sale in Canada and is designed
specifically for Consumers. This leaflet is a
summary and will not tell you everything about
Alembic-Lacosamide. Contact your doctor or
pharmacist if you have any questions about the
drug.
ABOUT THIS MEDICATION
What the medication is used for:
Alembic-Lacosamide is a prescription medicine used to
treat partial-onset seizures when taken on its own or
together with other seizure medicines in adults 18 years
and older.
What it does:
Alembic-Lacosamide works in the brain to block the
spread of seizure activity. The precise way that
lacosamide tablet works to treat partial-onset seizures is
unknown.
When it should not be used:
Do not take Alembic-Lacosamide if:
you are allergic to lacosamide or any of the other
ingredients in Alembic-Lacosamide tablets listed in
the “nonmedicinal ingredients” section below.
you suffer or have suffered in the past from a
certain type of heart rhythm disorder (second or
third degree AV block)
What the medicinal ingredient is:
Lacosamide
What the nonmedicinal ingredients are:
Alembic-Lacosamide Tablets nonmedicinal
ingredients: microcrystalline cellulose, crospovidone,
hydroxypropyl cellulose, low-substituted
hydroxypropyl cellulose
, colloidal silicon dioxide,
magnesium stearate, hypromellose, polyethylene
glycol, talc, titanium dioxide, and dye pigments:
50 mg tablets: FD&C Blue #2 aluminum lake, iron
oxide red, iron oxide black
100 mg tablets: iron oxide yellow
150 mg tablets: iron oxide yellow, iron oxide red, iron
oxide black
200 mg tablets: FD&C Blue #2 aluminum lake
What dosage forms it comes in:
Film-coated tablets: 50 mg, 100 mg, 150 mg and
200 mg
WARNINGS AND PRECAUTIONS
Alembic-Lacosamide may cause dizziness and
poor coordination which could increase the risk of
accidental injury or a fall. Therefore, you should be
careful until you are used to the effects this
medicine might have.
Do not drive, operate complex machinery, or
engage in other hazardous activities until you know
how Alembic-Lacosamide affects you. Ask your
doctor when it is okay to do these activities.
Alembic-Lacosamide may cause double vision and
blurred vision. If you experience visual
disturbances while taking Alembic-Lacosamide,
notify your doctor.
A small number of people being treated with anti-
epileptics such as Alembic-Lacosamide have had
thoughts of harming or killing themselves. If at any
time you have these thoughts, immediately contact
your doctor.
BEFORE you use Alembic-Lacosamide talk to
your doctor or pharmacist if:
you have any health problems, including ones
you have had in the past;
you have kidney or liver disease
you are taking any medication, including ones
you can get without a prescription;
you are taking any medicine which can cause
an abnormality on the ECG
(electrocardiogram) called increased PR
interval or heart block, for example medicines
used to treat certain types of irregular heart
beat or heart failure. If you are not sure that the
medicines you are taking could have this effect,
discuss this with your doctor (e.g.
carbamazepine, pregabalin, lamotrigine,
eslicarbazepine, beta-blockers, class I
antiarrhythmic drugs, etc.)
patients with pacemaker problems
you suffer from a severe heart disease such as
heart rhythm disorder, heart failure or heart
attack;

IMPORTANT: PLEASE READ
______________________________________________________________________________
Page 36 of 38
you are pregnant or plan to become pregnant. It
is not known if Alembic-Lacosamide may harm
your unborn baby. You and your doctor will
have to decide if Alembic-Lacosamide is right
for you while you are pregnant. If you use
Alembic-Lacosamide while you are pregnant,
ask your healthcare provider about joining the
North American Antiepileptic Drug Pregnancy
Registry by calling (888) 233-2334 (toll free).
Women who are pregnant and planning to take
Alembic-Lacosamide should call the pregnancy
registry to enable collection of valuable data
about lacosamide tablets use in pregnancy.
Information on the registry can also be found at
the following website:
http://www.aedpregnancyregistry.org/ ;
you are breastfeeding. It is not known if
lacosamide passes into breast milk and if it can
harm your baby. You and your doctor should
decide whether you should take Alembic-
Lacosamide or breastfeed, but not both.
INTERACTIONS WITH THIS MEDICATION
Tell your doctor about all the medicines you take
including prescription or non-prescription medicines,
vitamins or herbal supplements. Alembic-Lacosamide
and other medicines may affect each other. Especially
tell your doctor if you take:
any medicines that make you sleepy or dizzy
any medications to treat a heart condition
carbamazepine, pregabalin, lamotrigine,
eslicarbazepine, beta-blockers, class I
antiarrhythmic drugs, etc.
PROPER USE OF THIS MEDICATION
Alembic-Lacosamide film-coated tablets:
Alembic-Lacosamide may taken with or without
food.
Swallow the tablets whole with plenty of water.
Do not chew or crush tablets.
Usual Dose:
Alembic-Lacosamide must be taken twice a day, once
in the morning and once in the evening, at about the
same time each day.
When you take Alembic-Lacosamide on its own:
The treatment with lacosamide usually starts with 100
mg in the morning and 100 mg in the evening (200 mg
a day). After one week your dose may be increased.
The daily maintenance dose is between 200 mg and
600 mg.
When you take Alembic-Lacosamide with other
seizure medicines:
The treatment with lacosamide tablets usually
starts with a 50 mg in the morning and 50 mg in
the evening (100 mg a day). After one week your
dose may be increased. The daily maintenance
dose is between 200 mg and 400 mg.
Your doctor may use a different dose if you have
problems with your kidneys or liver .
If your doctor decides to stop your treatment with
Alembic-Lacosamide, he/she will decrease the
dose step by step. This is to prevent your
symptoms from coming back again or becoming
worse.
Do not stop taking Alembic-Lacosamide or any
other seizure medicine unless your healthcare
provider told you to. Stopping a seizure medicine
all at once can cause seizures that will not stop
(status epilepticus), a very serious problem.
Tell your healthcare provider if your seizures get
worse or if you have any new types of seizures.
Remember: This medicine has been prescribed
for you. Do not give it to anybody else.
Overdose:
In case of drug overdose, contact a health care
practitioner, hospital emergency department or
regional Poison Control Centre immediately, even if
there are no symptoms. Make sure you take your
medicine with you to show the doctor.
Missed Dose:
If you miss a dose by a few hours, take it as soon
as you remember. If it is close to your next dose,
take Alembic-Lacosamide at your next regular
time. Do not take two doses at the same time to
make up for the missed dose.
SIDE EFFECTS AND WHAT TO DO ABOUT
THEM
The most common side effects associated with the
use of Alembic-Lacosamide are:
dizziness, poor coordination
headache
nausea, vomiting, fatigue
blurred vision, double vision

IMPORTANT: PLEASE READ
______________________________________________________________________________
Page 37 of 38
If you are elderly (older than 65), you may have a
higher chance of the following side effects:
falling
diarrhea
tremors/shaking
Tell your doctor about any side effect that bothers you
or that does not go away.
SERIOUS SIDE EFFECTS, HOW OFTEN THEY
HAPPEN AND WHAT TO DO ABOUT THEM
Symptom / effect Talk with
your doctor
or pharmacist
Seek
Emergency
Medical
Attention
Only
if
severe
In
all
cases
Uncomm
on
Thoughts of
suicide or
hurting
yourself
√
Allergic
reaction:
swelling in
the mouth,
tongue, face
and throat,
itching, rash
√
Heart
rhythm
problems:
irregular
pulse, slow
pulse, rapid
pulse,
palpitations,
shortness of
breath,
feeling
lightheaded,
fainting
√
Rare
Allergic
reactions
that typically
present with
fever, rash
and swollen
lymph
nodes, and
may be
associated
with signs
and
symptoms
involving
other organs,
e.g. liver.
√
Liver
disorder or
√
SERIOUS SIDE EFFECTS, HOW OFTEN THEY
HAPPEN AND WHAT TO DO ABOUT THEM
liver injury:
itching, right
upper belly
pain, dark
urine,
yellow skin
or eyes,
unexplained
flu-like
symptoms
This is not a complete list of side effects. For any
unexpected effects while taking Alembic-
Lacosamide, contact your doctor or pharmacist.
HOW TO STORE IT
Store Alembic-Lacosamide at room
temperature, 15 to 30°C.
Keep Alembic-Lacosamide and all medicines
out of the reach and sight of children.
REPORTING SUSPECTED SIDE EFFECTS
You can report any suspected adverse reactions
associated with the use of health products to the
Canada Vigilance Program by one of the following 3
ways:
Report online at https://www.canada.ca/en/health-
canada/services/drugs-health-products/medeffect-
canada/adverse-reaction-reporting.html
Call toll-free at 1-866-234-2345
Complete a Canada Vigilance Reporting Form
and:
- Fax toll-free to 1-866-678-6789, or
- Mail to: Canada Vigilance Program
Health Canada
Postal Locator 1908C
Ottawa, ON K1A 0K9
Postage paid labels, Canada Vigilance Reporting Form
and the adverse reaction reporting guidelines are
available on the MedEffect
TM
Canada Web site at
www.healthcanada.gc.ca/medeffect.
NOTE: Should you require information related to the
management of side effects, contact your health
professional. The Canada Vigilance Program does not
provide medical advice.

IMPORTANT: PLEASE READ
______________________________________________________________________________
Page 38 of 38
MORE INFORMATION
Find the full product monograph that is prepared for
healthcare professionals and includes this Patient
Medication Information by visiting the Health Canada
website (https://health-products.canada.ca/dpd-
bdpp/index-eng.jsp) or by calling 1-888-620-5236.
This leaflet was prepared by Alembic Pharmaceuticals
Limited.
Manufactured by:
Alembic Pharmaceuticals Limited
Alembic Road,
Vadodara – 390003,
Gujarat, India
Canadian Importer and Distributor:
Alembic Pharmaceuticals Canada Ltd.
2680, Matheson Blvd. East, Unit 102
Mississauga, Ontario
L4W 0A5, Canada
Date of Preparation: December 19, 2018
